3.2 Emergency Situations
Nursing assistants must be prepared to respond to emergency situations when providing patient care. Common situations requiring immediate emergency response include heart attacks (myocardial infarctions), strokes (cerebrovascular accidents), seizures, falls, fires, and choking.
Heart Attack or Myocardial Infarction (MI)
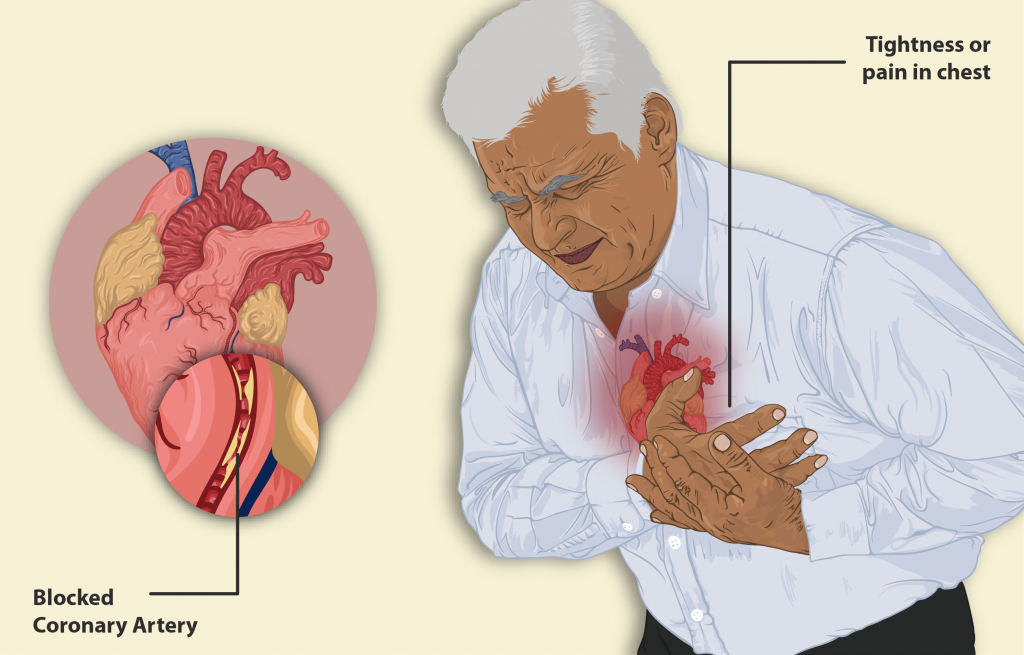
Myocardial infarction (MI) is the medical term for what is commonly referred to as a “heart attack.” It is caused by a lack of blood flow and oxygen to a region of the heart, resulting in the death of cardiac muscle cells. An MI is typically caused by a blocked coronary artery that occurs when the buildup of plaque creates a clot or when a piece of the plaque breaks off and travels to a smaller vessel, creating a blockage.
When the cardiac muscle cells are starved of oxygen and begin to die during an MI, there is typically a sudden onset of severe pain called angina beneath the sternum. This pain often radiates down the left arm or into the jaw. However, some patients (especially female patients) may not experience severe pain but instead experience symptoms that feel like indigestion. Patients may also have associated symptoms like difficulty catching their breath referred to as shortness of breath (SOB), sweating, anxiety, irregular heartbeats, nausea, vomiting, or fainting. Symptoms should be immediately reported to the nurse for emergency assessment and treatment to preserve as much of the heart as possible.[1] See Figure 3.1[2] for an illustration of a male experiencing a myocardial infarction.
View the following supplementary TED-Ed video[3] with additional information on heart attacks:
What Happens During a Heart Attack? – Krishna Sudhir.
Stroke or Cerebrovascular Attack (CVA)
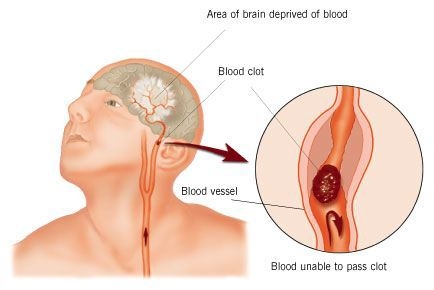
A cerebrovascular attack (CVA), often referred to as a “stroke” or “brain attack,” is caused by a lack of blood flow and oxygen to the brain, resulting in the death of brain cells within a few minutes. Similar to the cause of a heart attack, the lack of blood flow is often caused by a blockage in an artery, but in the case of a stroke, the artery is located in the brain. Strokes can also be caused by a blood vessel in the brain rupturing and bleeding, called a hemorrhagic stroke. Risk factors for strokes include smoking, high blood pressure, and cardiac arrhythmias (i.e., irregularities in heart rate and/or rhythm).
Lack of blood flow to the brain for more than a few minutes causes irreversible brain damage. The longer a person goes without treatment for a stroke, the more damage that occurs to their brain cells. Damaged brain cells can result in paralysis, cognitive impairment, difficulty speaking and understanding words, and mood swings. For this reason, it is important to recognize early signs of a stroke and obtain rapid emergency treatment.
The treatment for a stroke depends on the cause. Eighty percent of strokes occur due to a blockage of an artery in the brain. Strokes caused by a blockage are treated with thrombolytic medication (such as tPA) to dissolve the clot. See Figure 3.2[4] for an image of a stroke caused by a blockage. Hemorrhagic strokes occur due to a ruptured vessel in the brain. These types of strokes often require surgery to stop the bleeding. Stroke treatments work best if the symptoms of a stroke are recognized early and emergency treatment occurs within three hours of the onset of symptoms.[5]
Strokes typically affect one side of the brain based on where the blood flow was disrupted. Because of the brain’s anatomy, the symptoms of a stroke occur on the opposite side of the body as the affected side of the brain. For example, if a stroke occurs in the left side of the brain, the right side of the body will be affected, resulting in signs and symptoms occurring only on the right side of the body. This unilaterality (i.e., one-sidedness) of symptoms is important to recognize and report to the nurse.
The FAST acronym is used to remember early signs of a stroke:
- F: Facial drooping
- A: Arm weakness (unilateral)
- S: Slurred speech
- T: Time, meaning the quicker the response, the better the outcome
Given the central role and vital importance the brain is to life, it is critical that its blood supply remains uninterrupted. If blood flow is interrupted, even for just a few seconds, a transient ischemic attack (TIA), also called ministroke, may occur. A TIA is a temporary period of symptoms similar to those of a stroke, but they usually last only a few minutes, and they don’t cause permanent brain damage. However, TIAs can be a warning sign for a future stroke and should be reported to the nurse.
View a YouTube video[6] from the Centers for Disease Control and Prevention (CDC): Recognizing the Signs and Symptoms of Stroke
Seizure
A seizure is a transient occurrence of signs and/or symptoms due to abnormal activity in neurons in the brain. During a seizure, large numbers of brain cells are abnormally activated at the same time, like an electrical storm in the brain. This abnormal neuronal activity often affects a person’s consciousness and causes abnormal muscle movements.
Seizures are generally described in two major groups: generalized seizures and focal seizures. The difference between the types of seizures is in how and where they begin in the brain.[7]
Many symptoms can occur during a seizure. They are classified as motor or nonmotor symptoms. Motor symptoms include the following[8]:
- Sustained rhythmic jerking movements (clonic)
- Muscles becoming limp or weak (atonic)
- Body, arms, or legs becoming stiff or tense (tonic)
- Brief twitching (myoclonus)
Nonmotor symptoms are as follows[9]:
- Staring spells (absence seizures)
- Changes in sensation, emotions, thinking, or autonomic functions (nonmotor symptoms)
- Lack of movement (behavioral arrest)
When reporting a seizure to the nurse, include the following three descriptions[10]:
- The time the seizure started
- The person’s level of awareness during the seizure
- The movements that occurred during the seizure
If a resident has seizure disorder, it is typically noted in the nursing care plan. If you witness the beginning of a seizure, prepare to take quick action to reduce the chance of injury. For example, if the person is standing, the seizure can cause them to fall. You may not be able to stop the fall but try to guide them to the floor if possible. After they are on the floor, protect their head from directly hitting the floor by placing a pillow or your leg underneath their head. During the seizure, the person may bite their tongue or gag. However, do not place anything in their mouth because this will increase the risk of choking.
Immediately notify the nurse if you observe the start of a seizure and note the time it started. When the seizure has ended, carefully assist the person into bed. Due to the trauma experienced during the seizure, it is typical for the person to sleep for several hours. Some individuals with seizure disorders may also receive antianxiety medication to prevent another seizure from occurring.
View the Epilepsy Foundation’s YouTube video[11] of a person experiencing a seizure: Wendy says #ShareMySeizure.
View the Epilepsy Foundation’s YouTube video to learn more about seizure first aid[12]: Responding to Seizures: Care and Comfort First Aid.
Falls and Fall Prevention
Falls are common in adults aged 65 years and older. In the United States, about a third of older adults who live at home and about half of people living in nursing homes fall at least once a year. There are many factors that increase the risk of falling in older adults. These risk factors include mobility problems, balance disorders, chronic illnesses, and impaired vision. Many falls cause injury, ranging from mild bruising to broken bones, head injuries, and even death. In fact, falls are a leading cause of death in older adults.
If you enter a room and discover a resident has fallen, do not move them unless they are in immediate danger of further injury. Notify the nurse as soon as you observe the situation so the resident can be assessed and treated. Typically, a mechanical lift will be used to raise the resident from the floor to prevent injury to themselves and staff.
As a nursing assistant, there are several actions you can take to prevent falls. Keep the environment clean and free of clutter that can cause imbalance while a resident is ambulating (i.e., walking). If a spill is noted on the floor, it should be cleaned up immediately. Whenever residents are standing or walking, be sure they are wearing nonskid footwear (i.e., shoes or socks with rubberized soles). Use ordered assistive devices, such as gait belts and walkers, when moving a resident. If a resident wears glasses or hearing aids, make sure they are functioning, clean, and properly fitted for the resident so the resident can safely assess their surroundings when moving.[13] Additional information on fall risk and preventing falls can be found in Chapter 9.
Fire
In Chapter 2 you learned about agencies that govern health care, such as the Occupational Safety and Health Administration (OSHA). OSHA provides fire regulations and guidelines for every place of employment. This knowledge is essential for keeping residents safe in health care settings due to their limited mobility. Compliance to these regulations when responding to fires is commonly reviewed during the survey process.
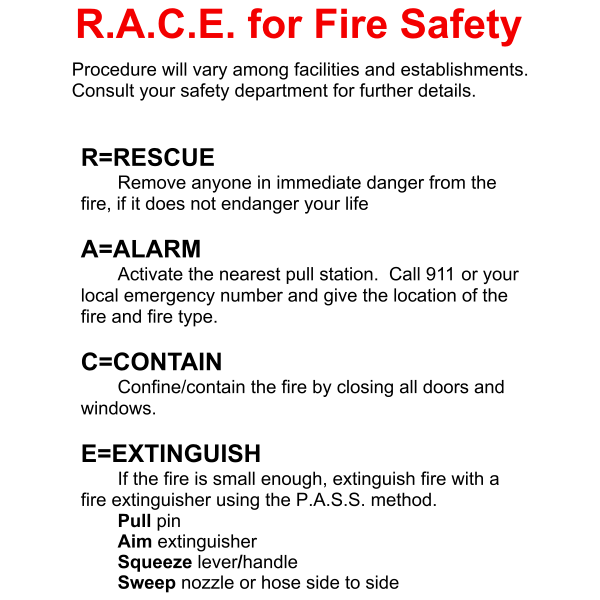
The response to a fire can be remembered by the RACE and PASS acronyms. See Figure 3.3[14] for using the PASS method with a fire extinguisher.
- R: Rescue anyone in immediate danger from the fire if it doesn’t endanger your life.
- A: Activate the alarm by pulling the nearest fire alarm or calling 911.
- C: Contain the fire by closing all doors and windows.
- E: Extinguish the fire if it is small enough using a fire extinguisher and the PASS method. If the fire cannot be extinguished, then evacuate patients and oneself from the area. The PASS method includes the following actions:
- P: Pull the pin on the fire extinguisher.
- A: Aim the extinguisher nozzle at the base of the fire.
- S: Squeeze or press the handle.
- S: Sweep from side to side at the base of the flame until the fire appears to be out.
View the UC San Diego Health’s YouTube video[15] on using RACE + PASS: RACE + PASS Training.
Choking and Airway Clearance
Choking is a common cause of unintentional injury and death. Over half of the people who die from choking are over the age of 70.[16] Food is often responsible for choking incidents in the elderly, especially those who have difficulty swallowing or have dentures. Many people who have dementia or who have had a previous stroke have difficulty swallowing. If you see any signs of choking, immediately notify the nurse and take action to clear the person’s airway.
If you are in a setting without a nurse present, it is important for you to know what to do and how to rescue someone who is choking. If a person is continuing to cough forcefully, encourage continued coughing to clear the object. However, a person who can’t cough, speak, or breathe needs immediate help. Ask the person if they are choking and let them know you will use abdominal thrusts, known as the Heimlich maneuver, to help them clear their airway and breathe. (Keep in mind the Heimlich maneuver is not recommended for children younger than 1.) See Figure 3.4[17] for an image of the Heimlich maneuver.
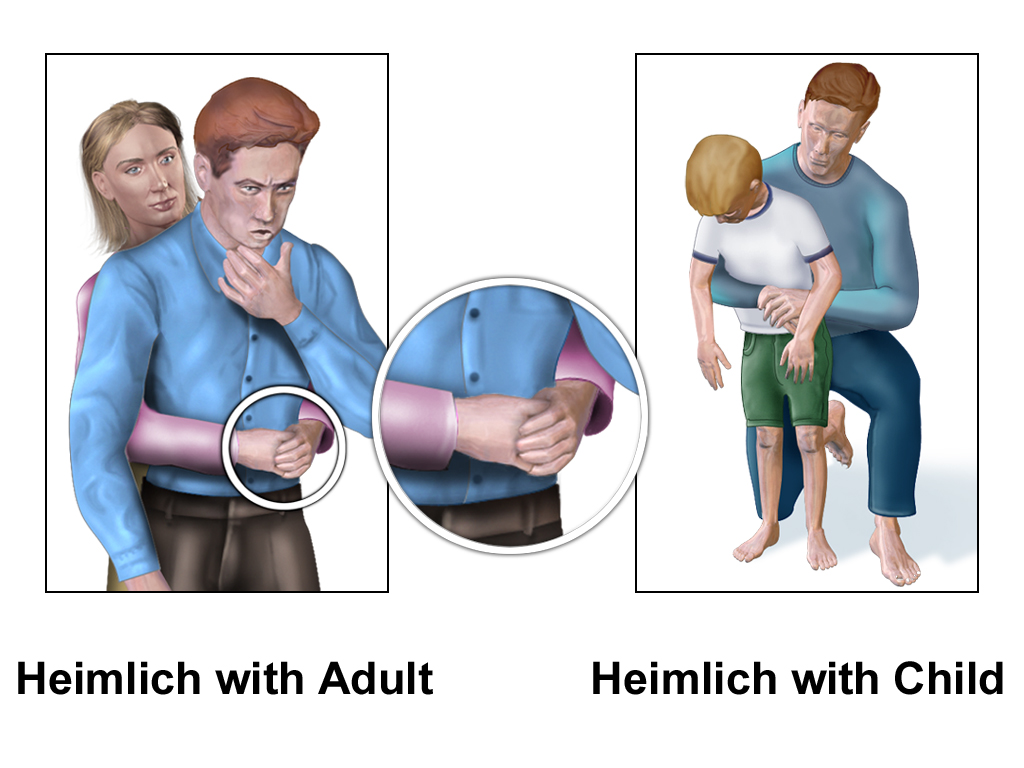
To perform the Heimlich maneuver, perform the following steps[18]:
- Stand behind the victim with one leg forward between the victim’s legs. If the person is sitting in a wheelchair or not able to stand, lean them forward in the chair and stand behind them.
- For a child, move down to their level and keep your head to one side.
- Reach around the abdomen and locate the navel.
- Place the thumb side of your fist against the abdomen just above the navel.
- Grasp your fist with your other hand and thrust inward and upward into the victim’s abdomen with quick jerks.
- For a responsive pregnant victim, any victim you cannot get your arms around, or for anyone in whom abdominal thrusts are not effective, give chest thrusts while standing behind them. Avoid squeezing the ribs with your arms.
- Continue thrusts until the victim expels the object or becomes unresponsive.
- If the person becomes unconscious, perform standard cardiopulmonary resuscitation (CPR) with chest compressions and rescue breaths.
- After choking stops, seek medical attention for the client.
View the “Skills Checklist: Choking Maneuver” with an associated video of performing the Heimlich maneuver.
- This work is a derivative of Nursing Pharmacology by Chippewa Valley Technical College and is licensed under CC BY 4.0 ↵
- “A man having a Heart Attack.png” by https://www.myupchar.com/en is licensed under CC BY-SA 4.0. ↵
- TED-Ed. (2017, February 14). What happens during a heart attack? - Krishna Sudhir [Video]. YouTube. All rights reserved. https://youtu.be/3_PYnWVoUzM ↵
- “Stroke Diagram” by ConstructionDealMkting is licensed under CC BY 2.0 ↵
- Centers for Disease Control and Prevention. (2020, August 28). Stroke. https://www.cdc.gov/stroke/signs_symptoms.htm ↵
- Centers for Disease Control and Prevention (CDC). (2015, October, 26). Recognize the Signs and Symptoms of Stroke. [Video]. YouTube. All rights reserved. https://youtu.be/cx5G1VdC9UA ↵
- Epilepsy Foundation. (2020). Types of seizures. https://www.epilepsy.com/learn/types-seizures ↵
- Epilepsy Foundation. (2020). Types of seizures. https://www.epilepsy.com/learn/types-seizures ↵
- Epilepsy Foundation. (2020). Types of seizures. https://www.epilepsy.com/learn/types-seizures ↵
- Epilepsy Foundation. (2020). Types of seizures. https://www.epilepsy.com/learn/types-seizures ↵
- Epilepsy Foundation. (2016, November 16). Wendy says #ShareMySeizure (30 sec) [Video]. YouTube. All rights reserved. https://youtu.be/KYQXSam1kww ↵
- Epilepsy Foundation. (2015, November 17). Responding to seizures: Care and comfort first aid [Video]. YouTube. All rights reserved. https://youtu.be/PAl9LDq9yas ↵
- MedlinePlus [Internet]. Bethesda (MD): National Library of Medicine (US). Stroke signs and symptoms; [reviewed 2020, Aug 28; cited 2021, Dec 3]. https://medlineplus.gov/lab-tests/fall-risk-assessment/ ↵
- “RACE-Safety--Arvin61r58.png” by unknown at Freesvg.org is licensed under CC0 1.0 ↵
- UCSD Visual Media Group. (2019, January 18). RACE + PASS training [Video]. YouTube. All rights reserved. https://youtu.be/pVHFdEivyNE ↵
- National Safety Council. (n.d.). Choking prevention and rescue tips. https://www.nsc.org/home-safety/safety-topics/choking-suffocation ↵
- “Heimlich_Adult_%26_Child.png” by BruceBlaus is licensed under CC BY-SA 4.0 ↵
- National Safety Council. (n.d.). Choking prevention and rescue tips. https://www.nsc.org/home-safety/safety-topics/choking-suffocation ↵
The medical term for what is commonly referred to as a “heart attack,” caused by a lack of blood flow and oxygen to the heart.
Sudden chest pain beneath the sternum (breastbone) associated with a heart attack (myocardial infarction), often radiating down the left arm in male patients. Angina is not as common in female patients.
Difficulty breathing or a feeling of not being able to catch one’s breath.
The medical term for what is commonly referred to as a “stroke,” caused by a lack of blood flow and oxygen to the brain.
Irregularities in a person’s heart rate and/or rhythm.
Medication (such as tPA) used to dissolve clots in arteries.
An acronym used to remember the early signs of a stroke: Facial drooping, Arm weakness, Slurred speech, and Time (meaning the quicker the response, the better the outcome).
A TIA is a temporary period of symptoms similar to those of a stroke, but they usually last only a few minutes and they don’t cause permanent brain damage.
A transient occurrence of signs and/or symptoms due to abnormal neuronal activity in the brain.
Walking.
Shoes or socks with rubberized soles used to prevent falls.
Devices such as gait belts and walkers that are used when moving a patient.
An acronym for responding to a fire.
An acronym for using a fire extinguisher.
A procedure used for someone who is choking that uses abdominal thrusts to clear the airway so they can breathe.

