9.3 Measuring and Improving Quality
Now that we have discussed the various ways that quality health care is defined, let’s discuss how quality care is measured, evaluated, and improved.
Utilization Review
Thinking back to value-based reimbursement models discussed in the “Health Care Economics” chapter, recall how health care agencies are reimbursed from Medicare, Medicaid, and private insurance based on their quality performance measures. A utilization review is an investigation of health care services performed by doctors, nurses, and other health care team members to ensure money is not wasted covering unnecessary or inefficient expenditures for proper treatment. Utilization review also allows organizations to objectively measure how their health care services and resources are being used to best meet their patients’ needs. Information from patients’ medical records is analyzed, along with patient demographics, to evaluate resource allocation, efficiency, and quality of health promotion initiatives.[1] See Figure 9.3[2] for an illustration of utilization review related to costs.

Using Informatics to Promote Quality
Utilization review relies on the collection of meaningful data from health records to determine if quality metrics are being met. Informatics refers to using information and technology to communicate, manage knowledge, mitigate error, and support decision-making.[3] Informatics allows members of the health care team to share, store, and analyze health-related information. Nurses have an important role in informatics. Nursing informatics is the science and practice of integrating nursing knowledge with information and communication technologies to promote the health of people, families, and communities worldwide.[4] It is a nursing specialty with certification available from the ANCC. See Figure 9.4[5] for an artistic rendition of informatics.

These are several benefits of using informatics in health care[6]:
- Improvement of Patient Safety: Informatics allows for up-to-date information sharing by both the patient and members of the health care team. Using informatics can help to reduce the occurrence of medication errors, as well as monitor patient side effects and overall health status. For example, barcode scanning has reduced medication errors by ensuring the correct dose is administered to the correct patient at the correct time.
- Reduction of Delays in Care: Some health care informatics systems allow for direct communication between health care team members and patients. The ability to ask and answer questions without needing to schedule an office appointment promotes the ability for care to be delivered efficiently in a cost-effective manner.
- Reduction of Waste: The use of informatics to share information between care team members reduces waste associated with duplication of tests or exams when more than one provider is on the care team. Additionally, patients can request their records be shared with health providers from other health organizations, which reduces duplication and unnecessary spending across the nation.
- Promotion of Patient-Centered Care: Many informatics systems have “patient portal” options where the patient and/or designated personnel are able to be active participants in the care planning and health promotion processes. Informatics offers an inclusive environment for patients to communicate and share directly with their care team regardless of physical location and timing.
- Support of Quality Improvement: The continuous process of quality improvement requires the ability to collect and analyze data in a systematic and reliable manner. Using informatics provides members of the health care team a secure place to store data, as well as the ability to review in a timely manner.
Quality Indicators
The National Database of Nursing Quality Indicators (NDNQI) was developed as a national nursing database used to evaluate quality in nursing care. This database was purchased by Press Ganey in 2014. In collaboration with the American Nursing Association (ANA), the original NDNQI database established nurse-sensitive quality indicators such as these[7]:
- Nursing Care Hours Per Patient Day
- Hospital-Acquired Pressure Injuries
- RN Job Satisfaction
Nurses use quality indicators to support practice changes with evidence directly related to improved patient outcomes.
Quality Improvement
Quality Improvement (QI) is a systematic process using measurable data to improve health care services and the overall health status of patients.[8] QI is one of the competencies of the Quality and Safety Education (QSEN) project and defined as, “using data to monitor the outcomes of care processes and using improvement methods to design and test changes to continuously improve the quality and safety of health care systems.”[9]
The overall goal of the QI process is to improve the quality and safety of health care. The process of quality improvement is very similar to the nursing process, but its purpose is to answer these three main questions:
- What are we trying to accomplish?
- How will we know if a change is an improvement?
- What changes can we make that will result in an improvement?
See Figure 9.5[10] for an illustration of the quality improvement process.
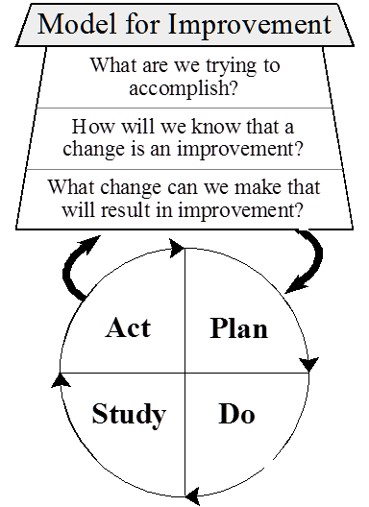
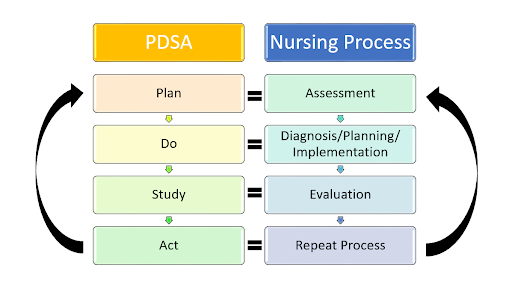
To answer these questions, QI is a continuous process in which a project is planned, interventions are implemented, data is collected, results are studied, and outcomes are evaluated. The process is repeated after additional planning. During the QI process, four key steps are used to evaluate current patient care and determine if changes are needed. These components are referred to as Plan, Do, Study, and Act:
- Plan: The first step in the QI process is to identify what you will be testing or focusing on and what will be measured. Similar to the nursing process where subjective and objective data are collected, the nurse determines what data will be needed during the QI process. The nurse also determines a timeline for the QI project, such as one year, including a specific framework for when data is collected and when it will be reviewed. For example, fall rates will decrease 10% in one year.
- Do: After the plan is determined, the nurse works with a health care team to implement the project and ensure data collection occurs.
- Study: During this phase, the nurse works with the health care team to review and analyze the data that was collected and determine if the outcomes were achieved or not.
- Act: In the fourth step of the QI process, the team discusses the outcomes. In this step the team identifies barriers, strengths, and weaknesses and then decides if additional changes are needed in nursing practice. The QI process is continuous, so the QI team uses outcome findings to continue the process of Plan, Do, Study, and Act to ensure safe, quality patient care.
PDSA Fall Rates Example
Reducing Patient Fall Rates
Objective: Decrease the patient fall rate in the hospital by 10% within one year.
Plan
- Identify the Focus: The QI project will focus on reducing patient falls in the hospital.
- Determine What to Measure: The primary metric will be the fall rate, calculated as the number of falls per 1,000 patient days.
- Collect Data: Baseline fall rates will be collected for the past year to understand current performance.
- Set Goals: Aim to reduce the fall rate by 10% within one year.
- Develop a Timeline:
- Initial Planning and Baseline Data Collection: Month 1
- Intervention Implementation: Months 2-4
- Data Collection and Monitoring: Months 2-12
- Initial Data Analysis: Month 6
- Final Data Analysis and Review: Month 12
Do
- Implement Interventions: Conduct fall prevention training sessions for all nursing staff. Ensure that patient rooms are free from clutter and that non-slip mats are in place. Install bed alarms and provide non-slip socks for patients. Implement a protocol for frequent rounding, especially for high-risk patients.
- Data Collection: Continuously collect data on fall incidents, including the circumstances of each fall.
Study
- Data Analysis: Review the fall rates monthly and compare them to the baseline data. Analyze trends and identify any patterns in the fall incidents. Determine if the interventions are associated with a reduction in fall rates.
2. Outcome Evaluation: Assess whether the goal of a 10% reduction in fall rates is being met. Identify any unexpected outcomes.
Act
- Discuss Outcomes: Hold meetings with the health care team to discuss the results. Identify barriers to successful implementation (e.g., lack of compliance with protocols, insufficient training). Recognize strengths (e.g., effective use of bed alarms, positive feedback from staff).
- Make Adjustments: If the fall rate has not decreased as expected, identify additional changes that might be needed (e.g., more frequent training, adjusting the rounding protocol). If successful, consider ways to further enhance the fall prevention program.
- Continuous Improvement: Use the findings to plan the next cycle of improvements. Set new goals based on the outcomes and continue the PDSA cycle to maintain and further improve patient safety
See Figure 9.6[11] for an illustration comparing the QI process to the nursing process.
It is important to note that quality improvement is different from nursing research. QI evaluates processes in place and determines if changes are needed, whereas the goal of research is to identify new innovations in nursing practice.[12]
Barriers to Quality Improvement
Barriers to quality improvement (QI) in health care organizations can be multifaceted, arising from a range of systemic, cultural, and practical challenges. One of the primary barriers is resistance to change among health care professionals. This resistance can stem from a lack of understanding of QI principles, fear of additional workload, or skepticism about the effectiveness of new practices. Overcoming this barrier requires robust education and training programs that highlight the benefits of QI initiatives and provide staff with the skills and knowledge needed to implement changes effectively. Also, having transparent conversations, discussing the process steps, and engaging staff questions are paramount.[13]
Another significant barrier is inadequate data management systems. Quality improvement relies heavily on accurate and timely data to identify areas for improvement, track progress, and measure outcomes. However, many health care organizations struggle with fragmented or outdated information systems that hinder data collection and analysis. Investing in modern, integrated health information technologies can facilitate better data management and support QI efforts. It also saves significant manpower and staff resources, allowing for more rapid identification of issues and trends.[14]
Resource constraints also pose a substantial challenge to quality improvement in health care. Financial limitations, staffing shortages, and limited time can impede the ability to implement and sustain QI initiatives. Organizations may find it difficult to allocate the necessary resources for training, process redesign, and continuous monitoring. Addressing this barrier often requires strategic planning, prioritization of QI projects, and seeking external funding or partnerships to support initiatives. Many organizations may have quality departments while others may utilize nursing staff to complete QI initiatives.[15]
Cultural factors in health care organizations can also impede quality improvement. Organizational culture that does not prioritize patient safety and continuous improvement can undermine QI efforts. This barrier can be addressed by fostering a culture of transparency, accountability, and collaboration. Leadership plays a crucial role in setting the tone and demonstrating a commitment to quality improvement. Engaging all levels of staff in QI processes and celebrating successes can help build a positive culture that supports ongoing improvement.[16]
Lastly, regulatory and policy constraints can limit the scope and flexibility of QI initiatives. Health care organizations operate within a complex regulatory environment that can sometimes create barriers to innovative practices. Navigating these regulations while attempting to implement QI can be challenging. Advocacy for policy changes that support QI, along with a thorough understanding of existing regulations, can help organizations find ways to work within or adapt to these constraints.[17]
- Institute of Medicine (US) Committee on Utilization Management by Third Parties, Gray, B. H., & Field, M. J., (Eds.). (1989). Controlling costs and changing patient care? The role of utilization management. National Academies Press. https://www.ncbi.nlm.nih.gov/books/NBK235000 ↵
- “Analyzing_Financial_Data_(5099605109).jpg” by Dave Dugdale is licensed under CC BY-SA 2.0 ↵
- QSEN Institute. (n.d.). QSEN competencies: Quality improvement (QI). https://qsen.org/competencies/pre-licensure-ksas/#quality_improvement ↵
- AMIA. (n.d.). Informatics: Research and practice. https://amia.org/about-amia/why-informatics/informatics-research-and-practice ↵
- “informatics-1322241_1920.jpg” by mariojsantos at Pixabay.com is licensed under CC0 ↵
- Otokiti, A. (2019). Using informatics to improve healthcare quality. International Journal of Health Care Qual Assurance, 32(2), 425-430. https://doi.org/10.1108/ijhcqa-03-2018-0062 ↵
- Montalvo, I. (2007). The National Database of Nursing Quality Indicators (NDNQI). The Online Journal of Issues in Nursing, 12(3). https://ojin.nursingworld.org/MainMenuCategories/ANAMarketplace/ANAPeriodicals/OJIN/TableofContents/Volume122007/No3Sept07/NursingQualityIndicators.aspx ↵
- Study.com. (n.d.). What is economics? - Definition, history, timeline & importance [Video]. https://study.com/academy/lesson/what-is-economics-definition-history-timeline-importance.html ↵
- QSEN Institute. (n.d.). QSEN competencies: Quality improvement (QI). https://qsen.org/competencies/pre-licensure-ksas/#quality_improvement ↵
- “Model_for_Improvement.jpg” by Cliffnorman is licensed under CC BY-SA 4.0 ↵
- “Comparison_QI Process_Nursing Process.jpg” by Amy Tyznik, MPTC for Open RN is licensed under CC BY 4.0 ↵
- Agency for Healthcare Research and Quality. (2013, May). Module 4. Approaches to quality improvement. Practice facilitation handbook. https://www.ahrq.gov/ncepcr/tools/pf-handbook/mod4.html ↵
- Giannitrapani, K., Satija. A., Ganesh, A., Gamboa, R., Fereydooni, S., Hennings, T., Chandrashekaran, S., Mickelsen, J., DeNatale, M., Spruijt, O., Bhatnagar, S., & Lorenz, K. A. (2021). Barriers and facilitators of using quality improvement to foster locally initiated innovation in palliative care services in India. Journal of General Internal Medicine, 36(2), 366-373. https://doi.org/10.1007/s11606-020-06152-y. ↵
- Giannitrapani, K., Satija. A., Ganesh, A., Gamboa, R., Fereydooni, S., Hennings, T., Chandrashekaran, S., Mickelsen, J., DeNatale, M., Spruijt, O., Bhatnagar, S., Lorenz, K. A. (2021). Barriers and facilitators of using quality improvement to foster locally initiated innovation in palliative care services in India. Journal of General Internal Medicine, 36(2), 366-373. https://doi.org/ 10.1007/s11606-020-06152-y. ↵
- Alexander, C., Tschannen, D., Argetsinger, D., Hakim, H., & Milner, K. A. (2022). A qualitative study on barriers and facilitators of quality improvement engagement by frontline nurses and leaders. Journal of Nursing Management, 30(3), 694-701. https://doi.org/10.1111/jonm.13537. ↵
- Alexander, C., Tschannen, D., Argetsinger, D., Hakim, H., & Milner, K. A. (2022). A qualitative study on barriers and facilitators of quality improvement engagement by frontline nurses and leaders. Journal of Nursing Management, 30(3), 694-701. https://doi.org/10.1111/jonm.13537. ↵
- Alexander, C., Tschannen, D., Argetsinger, D., Hakim, H., & Milner, K. A. (2022). A qualitative study on barriers and facilitators of quality improvement engagement by frontline nurses and leaders. Journal of Nursing Management, 30(3), 694-701. htttps://doi.org/10.1111/jonm.13537. ↵
An investigation by insurance agencies and other health care funders on services performed by doctors, nurses, and other health care team members to ensure money is not wasted covering things that are unnecessary for proper treatment or are inefficient.
Using information and technology to communicate, manage knowledge, mitigate error, and support decision-making.
The science and practice integrating nursing, its information and knowledge, with information and communication technologies to promote the health of people, families, and communities worldwide.
A systematic process using measurable data to improve health care services and the overall health status of patients.

