11.5 Transitioning to the RN Role
Reality Shock
As a new graduate transitions into the role of being a registered nurse (RN), it is very common to experience something called “reality shock.” Although Kramer’s “Reality Shock” theory is several decades old, it continues to apply to new nurses transitioning to their new role through a process of learning and growing. Kramer’s Reality Shock theory characterizes four phases of transitioning into a new role referred to as the honeymoon, shock, recovery, and resolution phases[1]:
- Honeymoon phase: The first phase occurs when the newly graduated RN is excited to join the nursing profession and it is everything they imagined. During this phase, the new nurse is typically paired up with a preceptor RN to orient them to the new role.
- Shock phase: The second phase is when the new RN is the most vulnerable. They are moved off orientation and independently perform tasks without the guidance of their preceptor. The RN role is often more difficult than the new nurse previously imagined. The new RN realizes their expectations associated with the nursing role may be inconsistent with the actual responsibilities. During this phase, negative feelings regarding their new profession may arise, and the new RN is at greatest risk for leaving the unit or quitting.
- Recovery phase: The third phase is when new RNs begin to have positive feelings towards their profession again. During this phase, the new RN is able to reflect on their experiences and develop a clear understanding of their responsibilities and role expectations. The novice RN typically experiences decreased tension and anxiety and begins to assist other RNs as needed.
- Resolution phase: The fourth and final phase is usually at the end of the first year of the new position. The new RN can visualize how the role contributes to the profession, and work expectations are easily met.
Transitioning Into Practice
Over the years, the National Council of State Boards of Nursing (NCSBN) has researched the complex issue of retaining new nursing graduates and found the inability of new nurses to properly transition into practice can have grave consequences. New nurses care for sicker clients in increasingly complex health settings and feel increased stress levels. As a result, new nurses are involved in more client safety and practice errors than experienced nurses. It has been reported by the NCSBN that within the first year of employment, 25% of novice RNs leave their nursing positions.[2]
There are several potential strategies for helping new nurses transition into practice. The first step of the transition is being aware of “reality shock” and the phases of the transition process. A thorough orientation process with an experienced preceptor is a traditional strategy for transitioning into a new nursing position. A newer strategy being implemented in some agencies is a nurse residency program.
Orientation may last anywhere from one to four months, but can be longer depending on the specialty (e.g., Intensive Care or Labor and Delivery). Orientation is based on the new nurse’s demonstration and completion of competencies. During this time, the novice RN will work with a preceptor to experience all aspects of the role.
Preceptors are experienced and competent RNs who serve as a role model and a resource to a newly hired nurse. Preceptors have the knowledge, skills, and the ability to coach the new RN into the nursing role and answer their questions. The preceptor also evaluates a new hire’s performance and provides feedback for improvement.
Nurse residency programs provide additional professional development support for all newly licensed nurses. Nurse residency programs vary from institution to institution, but many start around the time the new graduate ends their orientation with a preceptor and continue to provide routine support throughout the year. Residency programs are structured to provide a variety of learning opportunities, including nursing skill development, peer networking, and mentorship. The goal of nurse residency programs is to provide organizational support for newly licensed nurses during the critical phase of transitioning from student to professional nurse.[3] See Figure 11.5[4] for an image of new nurses participating in a nurse residency program.

Benner’s Novice to Expert Theory
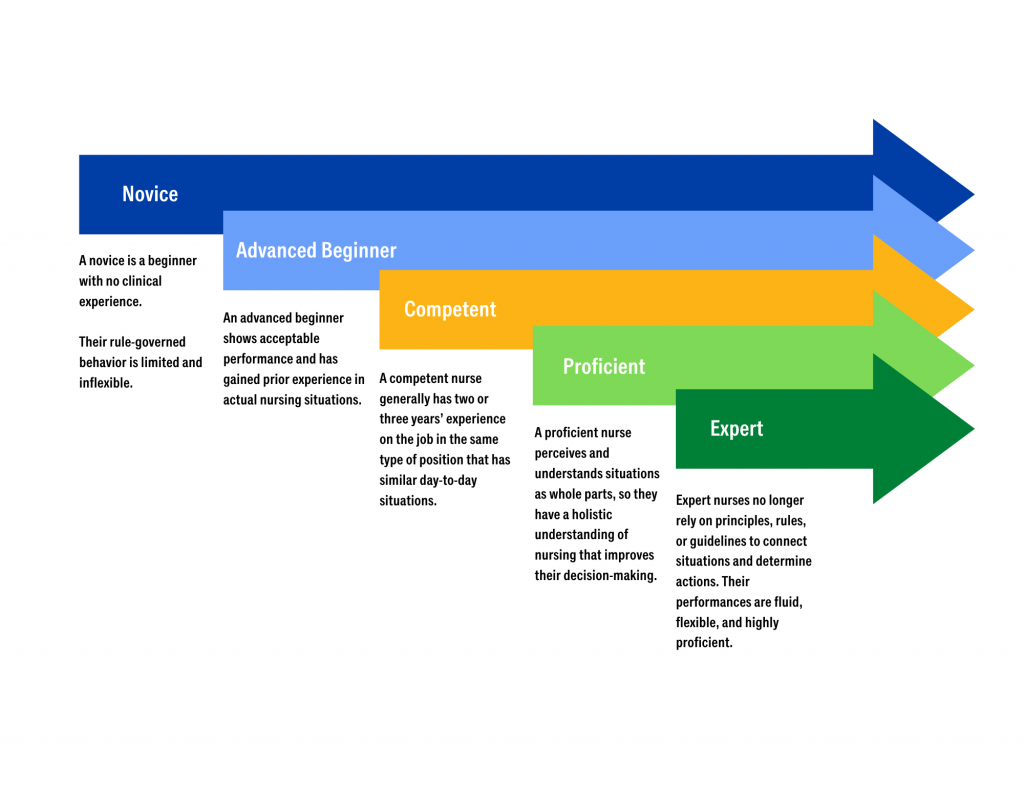
As a nursing graduate transitions into a new nursing role, a well-known theory called “Benner’s Novice to Expert Theory” explains how new hires develop skills and a holistic understanding of client care over time, resulting from a combination of a strong educational foundation and thorough clinical experiences. See Figure 11.6[5] for an illustration of Benner’s Novice to Expert Theory. Benner’s theory identifies five levels of nursing experience: novice, advanced beginner, competent, proficient, and expert.[6]
- A novice is a beginner with no clinical experience. They are taught general rules to help perform tasks, and their rule-governed behavior is limited and inflexible. In other words, they are told what to do and simply follow instructions.
- An advanced beginner shows acceptable performance and has gained prior experience in actual nursing situations. This experience helps the nurse recognize recurring patterns of client symptoms and behaviors. An advanced beginner begins to formulate strategies, based on their previous experiences, to guide actions.
- A competent nurse generally has two or three years’ experience on the job in the same type of position that has similar day-to-day situations. Competent nurses become aware of long-term goals and gain perspective from planning their own actions. This helps them achieve greater efficiency and organization.
- A proficient nurse perceives and understands situations as whole parts, so they have a holistic understanding of nursing that improves their decision-making. Proficient nurses have learned what to expect in various client situations and how to modify plans as needed.
- Expert nurses no longer rely on principles, rules, or guidelines to connect situations and determine actions. They have a deeper background of experience and an intuitive grasp of clinical situations. Their performances are fluid, flexible, and highly proficient.[7]
Mentorship
The value of mentorship in the nursing profession is immense, impacting both the personal and professional development of nurses and the overall quality of client care. Mentorship involves experienced nurses providing guidance, support, and knowledge to less experienced or new nurses, fostering their growth and integration into the profession. This relationship is essential for building a competent, confident, and resilient nursing workforce.[8]
One of the primary benefits of mentorship is the enhancement of clinical skills and knowledge. Experienced mentors share their expertise, clinical insights, and practical tips with mentees, helping them develop critical thinking and problem-solving abilities. This hands-on learning experience is invaluable, as it bridges the gap between theoretical knowledge and practical application. Through mentorship, new nurses gain confidence in their clinical competencies, leading to improved client care and safety.[9]
Mentorship also plays a crucial role in professional development. Mentors guide mentees in setting career goals, navigating career paths, and pursuing continuing education opportunities. They offer advice on advancing in the profession, whether through specialization, leadership roles, or academic achievements. This guidance helps nurses achieve their professional aspirations and contribute more effectively to the health care system. Additionally, mentors often serve as role models, demonstrating the qualities and behaviors essential for success in nursing.[10]
The supportive nature of mentorship fosters emotional and psychological well-being. The transition from nursing school to clinical practice can be challenging and stressful. Having a mentor provides new nurses with a trusted confidant who offers encouragement, listens to concerns, and provides constructive feedback. This support system helps reduce feelings of isolation and burnout, promoting job satisfaction and retention. Mentors can also help new nurses develop coping strategies and resilience, which are critical for long-term success in the demanding field of health care.[11]
Mentorship contributes to the creation of a positive and collaborative workplace culture. By fostering strong relationships between experienced and novice nurses, mentorship programs encourage teamwork, mutual respect, and knowledge sharing. This collaborative environment enhances communication, reduces errors, and improves overall client outcomes. Furthermore, a culture of mentorship promotes lifelong learning and continuous improvement, essential elements for maintaining high standards of care in a rapidly evolving health care landscape. For mentors, the experience is also enriching and rewarding. Mentoring provides opportunities for professional growth, leadership development, and personal satisfaction. It allows experienced nurses to reflect on their own practices, stay current with new trends and technologies, and contribute to the future of the nursing profession. The act of mentoring fosters a sense of purpose and fulfillment, reinforcing the mentor’s commitment to the profession and enhancing their own career satisfaction.[12]
Mentorship is a cornerstone of the nursing profession, offering substantial benefits to individual nurses, health care organizations, and clients. It enhances clinical skills, supports professional development, fosters emotional well-being, and promotes a positive workplace culture. By investing in mentorship programs, health care organizations can ensure the growth and success of their nursing staff, ultimately leading to higher quality care and better client outcomes.
- Kramer, M. (1974). Reality shock: Why nurses leave nursing. C. V. Mosby Co. ↵
- NCSBN. (n.d.). Transition to practice: Why transition to practice (TTP)? http://www.ncsbn.org/transition-to-practice.htm ↵
- Ackerson, K., & Stiles, K. A. (2018). Value of nurse residency programs in retaining new graduate nurses and their potential effect on the nursing shortage. The Journal of Continuing Education in Nursing, 49(6). https://doi.org/10.3928/00220124-20180517-09 ↵
- “1637163589.jpg" by Monkey Business Images is used under license from Shutterstock.com ↵
- “Novice to Expert.png” by Meredith Pomietlo for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- Nursing Theory. (2020). Dr. Patricia Benner novice to expert - nursing theorist. https://nursing-theory.org/nursing-theorists/Patricia-Benner.php ↵
- Nursing Theory. (2020). Dr. Patricia Benner novice to expert - nursing theorist. https://nursing-theory.org/nursing-theorists/Patricia-Benner.php ↵
- ANA. (2024). Mentorship in nursing: Benefits & why it's essential. https://www.nursingworld.org/content-hub/resources/nursing-resources/benefits-of-mentorship-in-nursing/#:~:text=As%20a%20mentor%2C%20you'll,be%20conducted%20formally%20or%20informally. ↵
- ANA. (2024). Mentorship in nursing: Benefits & why it's essential. https://www.nursingworld.org/content-hub/resources/nursing-resources/benefits-of-mentorship-in-nursing/#:~:text=As%20a%20mentor%2C%20you'll,be%20conducted%20formally%20or%20informally. ↵
- ANA. (2024). Mentorship in nursing: Benefits & why it's essential. https://www.nursingworld.org/content-hub/resources/nursing-resources/benefits-of-mentorship-in-nursing/#:~:text=As%20a%20mentor%2C%20you'll,be%20conducted%20formally%20or%20informally. ↵
- ANA. (2024). Mentorship in nursing: Benefits & why it's essential. https://www.nursingworld.org/content-hub/resources/nursing-resources/benefits-of-mentorship-in-nursing/#:~:text=As%20a%20mentor%2C%20you'll,be%20conducted%20formally%20or%20informally. ↵
- ANA. (2024). Mentorship in nursing: Benefits & why it's essential. https://www.nursingworld.org/content-hub/resources/nursing-resources/benefits-of-mentorship-in-nursing/#:~:text=As%20a%20mentor%2C%20you'll,be%20conducted%20formally%20or%20informally. ↵
A structured transition process when hired into a new position that typically lasts about four months, but can be longer depending on the speciality (e.g., Intensive Care or Labor and Delivery).
Experienced and competent RNs who serve as a role model and a resource to a newly hired nurse.
A transition process that provides additional professional development for newly licensed nurses.
A theory by Dr. Patricia Benner that explains how new hires develop skills and a holistic understanding of patient care over time, resulting from a combination of a strong educational foundation and thorough clinical experiences.

