10.5 Policy Advocacy
National, state, and local policies impact nurses at all levels of care, from nurse administrators to bedside nurses, making it essential for nurses to take an active role in advocating for their clients, their profession, and their community. Nurses advocate for improved access to basic health care, enhanced funding of health care services, and safe practice environments by participating in policy discussions. Nurses also participate in state and national policy discussions affecting nursing practice. For example, nurses advocate for the removal of practice barriers so nurses can practice according to the full extent of their education, certification, and licensure; address reimbursement based on the value of nursing care; and expand funding for nursing education.[1]
When advocating, nurses must view themselves as knowledgeable professionals who have the power to influence policy and decision-makers. A nurse can advocate for improved policies through a variety of pathways. Each method provides a unique opportunity for the nurse to impact the health of individuals and communities, the profession of nursing, and the overall health care provided to clients. These are few easy ways for nurses to get involved:
- Becoming involved in professional nursing organizations
- Engaging in conversations with local, state, and federal policymakers on health care related issues
- Participating in shared governance committees regarding workplace policies
Health Care Legislative Policies
Legislative policies are external rules and regulations that impact health care practice and policy at the national, state, and local levels. These regulations seek to protect clients and nurses by defining safe practices, quality standards, and requirements for health care organizations and insurance companies. Nurses have been involved in the adoption of these rules and regulations and continue to advocate for new and updated legislation affecting health care.
Examples of federal legislation addressing health care include advocating for the Patient’s Bill of Rights, client privacy and confidentiality, improved access to health care, and protections for individuals who report unethical or illegal activities in the health care environment (i.e., whistleblower legislation). Examples of legislation at the state level includes topics such as right-to-die and physician-assisted suicide, medicinal marijuana use, and nurse-to-client staffing ratios.
Review how client rights are defined by policies at the federal, state, and organizational levels in the following box.
Client’s Rights Defined at Multiple Levels
In 1973 the American Hospital Association (AHA) adopted the Patient’s Bill of Rights. The bill has since been updated and adapted for use throughout the world in all health care settings, but, in general, it safeguards a client’s right to accurate and complete information, fair treatment, and self-determination when making health care decisions. In 2010 the Affordable Care Act was passed at the federal level. It included additional client rights and protections for health care consumers in the areas of preexisting conditions, choice of providers, and limited lifetime coverage limits imposed by insurance companies.
States further define client rights beyond federal regulations and provide specific rights of health care consumers in their state. For example, Wisconsin’s Department of Health Services defines treatment rights, protections for records privacy and access, communication rights, personal rights, and privacy rights.
Read more about Patient Rights in the American Healthcare System.
Visit the CMS web page to read more about the Affordable Care Act and the revised Patient’s Bill of Rights.
Research advocacy policies in your state. Here is Wisconsin’s law regarding client rights.
Nurses’ Roles in Legislative Policies
With over four million registered nurses in the United States, nursing has a powerful voice that can significantly influence health care legislation. Nurses have been recognized as a major influence on health care policies related to client safety and quality care. They can become involved in policy making at the state and federal level by joining a professional nursing organization, communicating with their state representatives, or running for political office to take an active role in policy creation.
Most professional nursing organizations have a legislative policy committee that reviews proposed federal and state legislation and makes recommendations for change, endorses the legislation, or leads opposition. For example, organizations such as the American Nurses Association (ANA), National League of Nursing (NLN), and state nursing associations inform members of current legislative initiatives, provide comprehensive reviews, and encourage members to contact their representatives about pending legislation.
Read more about current advocacy efforts by the Wisconsin Nurses Association.
Whistleblowing
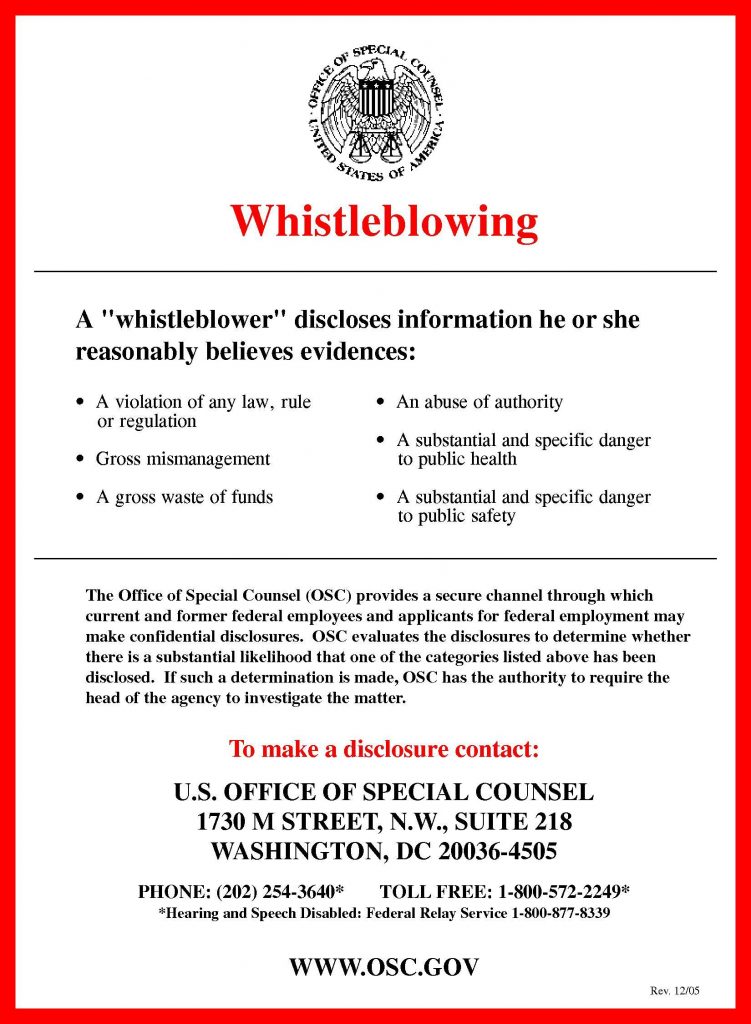
Nurses are expected to follow federal, state, and agency policies and regulations, be proactive in policy development, and speak up when policies are not being followed. When regulations and policies are not being followed, nurses must advocate for public safety by reporting the problem to a higher authority. Whistleblowing refers to reporting a significant concern to your supervisor, the federal or state agency responsible for the regulation, or in the case of criminal activity, to law enforcement agencies. A whistleblower is a person who exposes any kind of information or activity that is deemed illegal, unethical, or not correct within an organization. See Figure 10.5[2] for federal instructions regarding whistleblowing.
Whistleblowing typically begins with reporting the wrongdoing to a supervisor and following the internal chain of command. This first step of reporting allows the organization to correct the issue internally. However, there may be situations where an individual may need to directly report to an external authority, such as a State Board of Nursing or another regulatory agency. For example, any person who has knowledge of conduct by a licensed nurse violating state or federal law may report the alleged violation to the State Board of Nursing where the conduct occurred.
Acting as a whistleblower can be a difficult decision because the individual may be labelled “disloyal” or potentially face retaliatory actions by the accused individual or organization. Although there are legal protections for whistleblowers, these types of actions may occur. Read important information from the ANA regarding whistleblowing in the following box.
ANA Information Regarding Whistleblowing[3]
- If you identify an illegal or unethical practice, reserve judgment until you have adequate documentation to establish wrongdoing.
- Do not expect those who are engaged in unethical or illegal conduct to welcome your questions or concerns about this practice.
- Seek the counsel of someone you trust outside of the situation to provide you with an objective perspective.
- Consult with your state nurses’ association or legal counsel if possible before taking action to determine how best to document your concerns.
- Remember, you are not protected in a whistleblower situation from retaliation by your employer until you blow the whistle.
- Blowing the whistle means that you report your concern to the national and/or state agency responsible for regulation of the organization for which you work or, in the case of criminal activity, to law enforcement agencies as well.
- Private groups, such as The Joint Commission or the National Committee for Quality Assurance, do not confer protection. You must report to a state or national regulator.
- Although it is not required by every regulatory agency, it is a good rule of thumb to put your complaint in writing.
- Document all interactions related to the whistleblowing situation and keep copies for your personal file.
- Keep documentation and interactions objective.
- Remain calm and do not lose your temper, even if those who learn of your actions attempt to provoke you.
- Remember that blowing the whistle is a very serious matter. Do not blow the whistle frivolously. Make sure you have the facts straight before taking action.
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- “Whistleblowing.pdf’” by United States Office of Special Counsel is in the Public Domain ↵
- American Nurses Association. Things to know about whistle blowing. https://www.nursingworld.org/practice-policy/workforce/things-to-know-about-whistle-blowing/ ↵
A person who exposes any kind of information or activity that is deemed illegal, unethical, or not correct within an organization.

