8.4 Health Care Reimbursement Models
As discussed in the previous section, hospitals and health care providers are paid for services provided to individuals by government insurance programs (such as Medicare and Medicaid), private insurance companies, or people using their out-of-pocket funds. Traditionally, health care institutions were paid based on a “fee-for-service” model. For example, if a client was admitted to a hospital with pneumonia, the hospital billed that individual’s insurance program for the cost of care.
However, as part of a recent national strategy to reduce health care costs, insurance providers have transitioned to “Pay for Performance” reimbursement models that are based on overall agency performance and client outcomes.
Pay for Performance
Pay for Performance, also known as value-based payment, refers to reimbursement models that attach financial incentives to the performance of health care agencies and providers. Pay for Performance models tie higher reimbursement payments to positive client outcomes, best practices, and client satisfaction, thus aligning payment with value and quality.[1] Nurses support higher reimbursement levels to their employers based on their documentation related to nursing care plans and achievement of expected client outcomes.
There are two Pay for Performance models. The first model rewards hospitals and providers with higher reimbursement payments based on how well they perform on process, quality, and efficiency measures. The second model penalizes hospitals and providers for subpar performance by reducing reimbursement amounts.[2] For example, Medicare no longer reimburses hospitals to treat clients who acquire certain preventable conditions during their hospital stay, such as pressure injuries or urinary tract infections associated with use of catheters.[3]
The Centers for Medicare and Medicaid Services (CMS), spurred by the Affordable Care Act, has led the way in value-based payment with a variety of payment models. CMS is the largest health care funder in the United States with almost 40% of overall health care spending for Medicare and Medicaid. CMS developed three Pay for Performance models that impact hospitals’ reimbursement by Medicare. These models are called the Hospital Value-Based Purchasing Program, the Hospital Readmissions Reduction Program, and the Hospital-Acquired Condition Reduction Program. Private insurers are also committed to performance-based payment models. In 2017 Forbes reported that almost 50% of insurers’ reimbursements were in the form of value-based care models.[4]
Hospital Value-Based Purchasing Program
The Hospital Value-Based Purchasing Program (VBP) was designed to improve health care quality and client experience by using financial incentives that encourage hospitals to follow established best clinical practices and improve client satisfaction scores via client satisfaction surveys. Reimbursement is based on hospital performance on measures divided into four quality domains: safety, clinical care, efficiency and cost reduction, and client and caregiver-centered experience.[5] The VBP program rewards hospitals based on the quality of care provided to Medicare clients and not just the quantity of services that are provided. Hospitals may have their Medicaid payments reduced by up to 2% if not meeting the quality metrics.
Read more about client satisfaction surveys.
Hospital Readmissions Reduction Program
The Hospital Readmissions Reduction Program (HRRP) penalizes hospitals with higher rates of client readmissions compared to other hospitals. HRRP was established by the Affordable Care Act and applies to clients with specific conditions, such as heart attacks, heart failure, pneumonia, chronic obstructive pulmonary disease (COPD), hip or knee replacements, and coronary bypass surgery. Hospitals with poor performance receive a 3% reduction of their Medicare payments. However, it was discovered that hospitals with higher proportions of low-income clients were penalized the most, so Congress passed legislation in 2019 that divided hospitals into groups for comparison based on the socioeconomic status of their client populations.[6]
Hospital-Acquired Condition Reduction Program
The Hospital-Acquired Condition Reduction Program (HACRP) was established by the Affordable Care Act. This Pay for Performance model reduces payments to hospitals based on poor performance regarding client safety and hospital-acquired conditions, such as surgical site infections, hip fractures resulting from falls, and pressure injuries. This model has saved Medicare approximately $350 million per year.[7]
The HACRP model measures the incidence of hospital-acquired conditions, including central line-associated bloodstream infections (CLABSI), catheter-associated urinary tract infections (CAUTI), surgical site infections (SSI), Methicillin-Resistant Staphylococcus Aureus (MRSA), and Clostridium Difficile (C. diff).[8] As a result, nurses have seen changes in daily practices based on evidence-based practices related to these conditions. For example, stringent documentation is now required for clients with Foley catheters that indicates continued need and associated infection control measures.
Other CMS Pay for Performance Models
CMS has created other value-based payment programs for agencies other than hospitals, including the End-Stage Renal Disease (ESRD) Quality Initiative Program, the Skilled Nursing Facility Value-Based Program (SNFVBP), the Home Health Value-Based Program (HHVBP), and the Value Modifier (VM) Program. The VM program is aimed at Medicare Part B providers who receive high, average, or low ratings based on quality and cost measurements as compared to peer agencies.
Impacts of Value-Based Payment
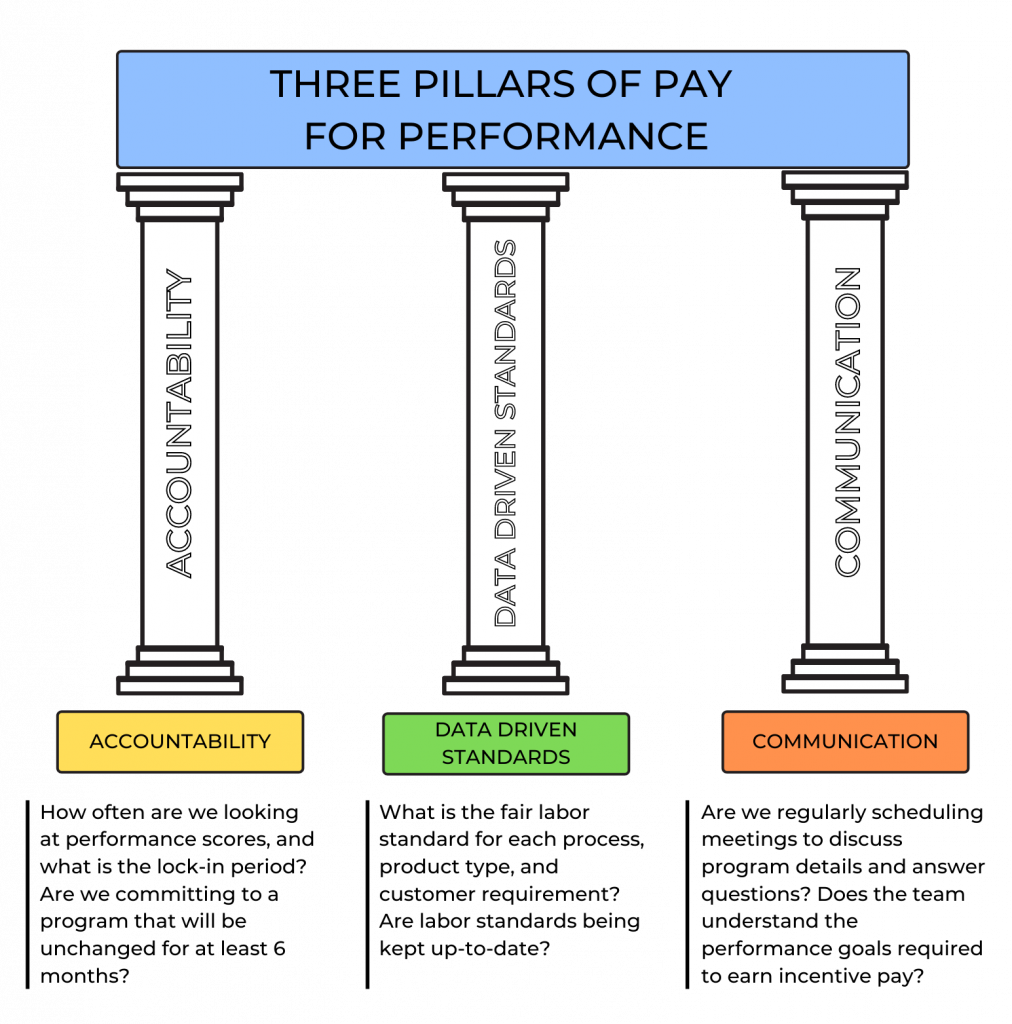
Pay for Performance (i.e., value-based payment) stresses quality over quantity of care and allows health care payers to use reimbursement to encourage best clinical practices and promote positive health outcomes. It focuses on transparency by using metrics that are publicly reported, thus incentivizing organizations to protect and strengthen their reputations. In this manner, Pay for Performance models encourage accountability and consumer-informed choice.[9] See Figure 8.8[10] for an illustration of Pay for Performance.
Pay for Performance models have reduced health care costs and decreased the incidence of poor client outcomes. For example, 30-day hospital readmission rates have been falling since 2012, indicating HRRP and HACRP are having an impact.[11]
However, there are also disadvantages to value-based payment. As previously discussed, initial research indicated hospitals with higher proportions of low-income clients were being penalized the most, resulting in additional legislation to compare hospital performance in groups based on their clients’ socioeconomic status. Nursing leaders continue to emphasize strategies that further address social determinants of health and promote health equity.[12] Read more about equity and social determinants of health in the following subsection.
Nursing Considerations
Nurses have a direct impact on activities related to quality care and reimbursement rates received by their employer. There are several categories of actions nurses can take to improve quality client care, reduce costs, and improve reimbursement. By incorporating these actions into their daily care, nurses can help ensure the funding they need to provide quality client care is received by their employer and resources are allocated appropriately to their clients.
The following categories of actions to improve quality of care are based on the Institute of Medicine (IOM) report To Err Is Human: Building a Safer Health Care System and Crossing the Quality Chasm[13]:
- Effectiveness and Efficiency: Nurses support their institution’s effectiveness and efficiency with individualized nursing care planning, good documentation, and care coordination. With accurate and timely documentation and care coordination, there is reduced care duplication and waste. Coordinating care also helps to reduce the risk of hospital readmissions.
- Timeliness: Nurses positively impact timeliness by prioritizing and delegating care. This helps reduce client wait times and delays in care. Read more about these concepts in the “Delegation and Supervision” and “Prioritization” chapters in this book.
- Safety: Nurses pay attention to their clients’ changing conditions and effectively communicate these changes with appropriate health care team members. They take any concerns about client care up the chain of command until their concerns are resolved.
- Client-Centered Care: Nurses support this quality measure by ensuring nursing care plans are individualized for each client. Effective care plans can improve client compliance, resulting in improved client outcomes.
- Evidence-Based Practice: Nurses provide care based on evidence-based practice. Evidence-Based Practice (EBP) is defined by the American Nurses Association as, “A lifelong problem-solving approach that integrates the best evidence from well-designed research studies and evidence-based theories; clinical expertise and evidence from assessment of the health care consumer’s history and condition, as well as health care resources; and client, family, group, community, and population preferences and values.”[14] EBP is a component of Scholarly Inquiry, one of the ANA’s Standards of Professional Practice. Nurses’ implementation of EBP ensures proper resources are allocated to the appropriate clients. EBP promotes safe, efficient, and effective health care.[15],[16] Read more information about EBP in the “Quality and Evidence-Based Practice” chapter of this book.
- Equity: Health care institutions care for all members of their community regardless of client demographics and their associated social determinants of health (SDOH). SDOH are conditions in the places where people live, learn, work, and play that affect a wide range of health risks and outcomes. Health disparities in communities with poor SDOH have been consistently documented in reports by the Agency for Healthcare Research and Quality (AHRQ).[17]
Nurses address negative determinants of health by advocating for interventions that reduce health disparities and promote the delivery of equitable health care resources. The term health disparities describes the differences in health outcomes that result from SDOH. Advocating for resources that enhance quality of life can significantly influence a community’s health outcomes. Examples of resources that promote health include safe and affordable housing, access to education, public safety, availability of healthy foods, local emergency/health services, and environments free of life-threatening toxins.
A related term is health care disparity that refers to differences in access to health care and insurance coverage. Health disparities and health care disparities can lead to decreased quality of life, increased personal costs, and lower life expectancy. More broadly, these disparities also translate to greater societal costs, such as the financial burden of uncontrolled chronic illnesses. An example of nurses addressing health care disparities are nurse practitioners providing health care according to their scope of practice to underserved populations in rural communities.
The ANA promotes nurse advocacy in workplaces and local communities. There are many ways nurses can promote health and wellness within their communities through a variety of advocacy programs at the federal, state, and community level.[18] Read more information in the “Advocacy” chapter of this book and additional information about advocacy and reducing health disparities in the following boxes.
Read more about ANA Policy and Advocacy.
Read more about addressing health disparities in the “Diverse Patients” chapter in Open RN Nursing Fundamentals, 2e.
- Pay for Performance. (2018). NEJM catalyst. https://catalyst.nejm.org/doi/full/10.1056/CAT.18.0245 ↵
- Pay for Performance. (2018). NEJM catalyst. https://catalyst.nejm.org/doi/full/10.1056/CAT.18.0245 ↵
- James, J. (2012). Pay-for-performance. Health Affairs. https://www.healthaffairs.org/do/10.1377/hpb20121011.90233/full/ ↵
- Pay for Performance. (2018). NEJM catalyst. https://catalyst.nejm.org/doi/full/10.1056/CAT.18.0245 ↵
- Pay for Performance. (2018). NEJM catalyst. https://catalyst.nejm.org/doi/full/10.1056/CAT.18.0245 ↵
- Pay for Performance. (2018). NEJM catalyst. https://catalyst.nejm.org/doi/full/10.1056/CAT.18.0245 ↵
- Pay for Performance. (2018). NEJM catalyst. https://catalyst.nejm.org/doi/full/10.1056/CAT.18.0245 ↵
- Pay for Performance. (2018). NEJM catalyst. https://catalyst.nejm.org/doi/full/10.1056/CAT.18.0245 ↵
- Pay for Performance. (2018). NEJM catalyst. https://catalyst.nejm.org/doi/full/10.1056/CAT.18.0245 ↵
- “Pillars of Pay Performance.png” by Meredith Pomietlo for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- Pay for Performance. (2018). NEJM catalyst. https://catalyst.nejm.org/doi/full/10.1056/CAT.18.0245 ↵
- Pay for Performance. (2018). NEJM catalyst. https://catalyst.nejm.org/doi/full/10.1056/CAT.18.0245 ↵
- Avalere Health LLC. (2015). Optimal nurse staffing to improve quality of care and patient outcomes: Executive summary [White paper]. https://cdn2.hubspot.net/hubfs/4850206/ANA/NurseStaffingWhitePaper_Final.pdf?__hstc=53609399.b25284991e95c5d4f1c55a49e826489f.1612299494138.1628353446072.1628356381954.16&__hssc=53609399.3.1628356381954&__hsfp=1865500357 ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- Stevens, K. (2013). The impact of evidence-based practice in nursing and the next big ideas. OJIN: The Online Journal of Issues in Nursing, 18(2). https://ojin.nursingworld.org/MainMenuCategories/ANAMarketplace/ANAPeriodicals/OJIN/TableofContents/Vol-18-2013/No2-May-2013/Impact-of-Evidence-Based-Practice.html ↵
- Centers for Disease Control and Prevention. (2020). Social determinants of health: Know what affects health. https://www.cdc.gov/socialdeterminants/index.htm ↵
- Agency for Healthcare Research and Quality. (2021). 2019 national healthcare quality and disparities report. https://www.ahrq.gov/research/findings/nhqrdr/nhqdr19/index.html ↵
A reimbursement model, also known as value-based payment, that attaches financial incentives based on the performance of health care agencies and providers.
A lifelong problem-solving approach that integrates the best evidence from well-designed research studies and evidence-based theories; clinical expertise and evidence from assessment of the health care consumer’s history and condition, as well as health care resources; and patient, family, group, community, and population preferences and values.
Conditions in the places where people live, learn, work, and play, such as unstable housing, low income areas, unsafe neighborhoods, or substandard education that affect a wide range of health risks and outcomes.
Differences in health outcomes that result from social determinants of health (SDOH).
Differences in access to health care and insurance coverage.

