6.12 Blood Coagulation Modifiers
Open Resources for Nursing (Open RN)
This section will discuss medications that affect blood coagulation and includes several types of medications including anticoagulants, antiplatelets, and thrombolytics, as well as their associated reversal agents.
Anticoagulants prevent the formation of a clot by inhibiting certain types of clotting factors. Anticoagulants include the following drug classes: heparins or unfractionated heparin and low molecular weight heparin (LMWH), warfarin (Coumadin), selective factor Xa inhibitors (rivaroxaban), and direct thrombin inhibitors (dabigatran). Antiplatelets include aspirin and other aggregation inhibitors such as clopidogrel, and thrombolytics include alteplase (tPA). All these types of medications are included on the List of High Alert Medications (HAMs) by the Institute for Safe Medication Practices (ISMP) that require special safeguards to reduce the risk of errors or adverse effects.[1]
The most common anticoagulant errors in acute hospital settings are administration mistakes, including incorrect dosage calculation and infusion rates. The Health Research and Educational Trust focuses on reducing harm related to HAMs by 50% and recommends the following interventions to achieve this goal:
- Educate staff based on evidence and best practices.
- Use standardized order sets and protocols.
- Perform medication reconciliation at all transitions.
Specific interventions regarding anticoagulant therapy include standardization of protocols for withholding and restarting warfarin perioperatively, including pharmacists on rounds to provide decision support for staff administering HAMs and to reduce prescribing errors, pharmacist monitoring of anticoagulants, and pharmacist notification when rescue medications are given.[2]
According to the Institute for Safe Medication Practices (ISMP) 2016 Annual Report, there is also a high risk of acute injuries for patients taking anticoagulants outside of the hospital setting. Anticoagulants are commonly used by the elderly to reduce the risk of ischemic stroke, with an estimated 3.8 million people taking oral anticoagulants in 2016. CDC data show that adverse effects of oral anticoagulants account for more emergency department visits than any other class of drugs. Adverse effects range from gastrointestinal bleeding to cerebral hemorrhages, resulting in over 3,000 deaths in 2016.[3]
Since 1954, warfarin has been a standard but hazardous treatment for preventing blood clots. Warfarin requires close laboratory monitoring and individual dose adjustments based on PT and INR lab results. When the pharmaceutical industry began marketing modern replacements for warfarin, including dabigatran (Pradaxa), rivaroxaban (Xarelto), and apixaban (Eliquis), they designed them to be easier to use than warfarin because no laboratory monitoring was required, but not necessarily safer. It is vital for nurses to provide thorough patient and caregiver education for patients prescribed anticoagulants at home. Suggested patient education topics are included for each type of medication below.
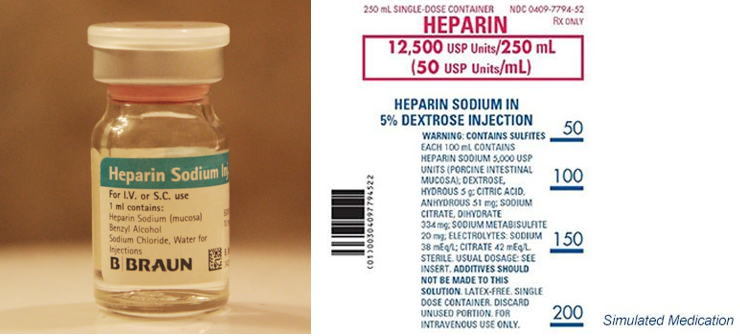
Heparin Sodium
Heparin sodium is an anticoagulant that can be injected or used intravenously and is formulated in several dosages. (See Figure 6.25.)[4] Due to heparin being a high-alert medication, hospitals use several processes for storing and labeling the medication to help prevent errors. It is also important to note that there is a type of heparin flush often referred to as “Hep-Lock” that is used to maintain the patency of central lines. The dosage of heparin in heparin IV flushes is much different than the heparin dose used as an intravenous medication to prevent or treat a blood clot.
Most hospitals have weight-based protocols for IV heparin administration that titrate a patient’s dosage to be within a therapeutic range based on the results of a lab test called Partial thromboplastin time (PTT). PTT is a blood test that looks at how long it takes for blood to clot. Patients receiving heparin subcutaneous injections to prevent DVTs (deep vein thrombosis) do not require PTT monitoring.
Mechanism of Action
Heparin inhibits the activated coagulation factors involved in the clotting sequence, particularly Xa and IIa. Heparin also prevents the formation of a stable fibrin clot by inhibiting the activation of the fibrin stabilizing factor. Heparin does not have fibrinolytic activity; therefore, it will not breakdown existing clots.
Indications for Use
IV heparin is commonly indicated for the treatment of deep venous thromboembolism (DVT) or pulmonary embolism. It is also indicated for use during an acute myocardial infarction. Subcutaneous heparin is commonly indicated to prevent DVT or embolization caused by atrial fibrillation. Heparin IV flushes (“Hep-Locks”) are used to maintain the patency of central IV lines.
Nursing Considerations Across the Lifespan
When bleeding requires the reversal of heparinization, protamine sulfate by slow infusion will neutralize heparin sodium.
A higher incidence of bleeding has been reported in patients over 60 years of age, especially women.
Fatal hemorrhages have occurred due to medication errors. Carefully examine all heparin products to confirm the correct dose prior to the administration of the drug.
IV heparin therapy requires close monitoring of frequent partial thromboplastin time (PTT) results to ensure dosage is in therapeutic range and to reduce the risk of overdose with associated bleeding. Dosage is considered adequate when the activated partial thromboplastin time (APTT) is 1.5 to 2 times the normal or when the whole blood clotting time is elevated approximately 2.5 to 3 times the control value.
This drug is contraindicated in patients with a history of Heparin-Induced Thrombocytopenia (HIT) and Heparin-Induced Thrombocytopenia and Thrombosis (HITT). HIT is a condition where platelets drop 30% or more below a patient’s baseline after heparin is administered and can lead to HITT where thrombi are formed.
Use with caution with medication that affects the coagulation cascade due to additive effects that increase the risk of bleeding. When a patient is receiving IV heparin therapy to treat a blood clot, it may be overlapped with oral warfarin to establish anticoagulation therapy after discharge. See more information about this process under the “Warfarin” section.
Adverse/Side Effects
There is a high risk of bleeding that can lead to hemorrhaging. Notify prescribing provider immediately of new signs of bleeding or bruising or sudden changes in vital signs that indicate internal bleeding, such as decreasing blood pressure with an associated increase in heart rate.
Some patients may develop Heparin-Induced Thrombocytopenia (HIT) or Heparin-Induced Thrombocytopenia and Thrombosis (HITT); therefore, heparin should be immediately discontinued.
Patient Teaching & Education
Notify health care staff immediately of new signs of bleeding or bruising. Remind physicians and dentists that they are receiving heparin before any surgery or invasive procedure is scheduled.[5] Patients should avoid medications containing aspirin or NSAIDS. Bleeding precautions should be taken, including the avoidance of IM injections, use of a soft toothbrush, and elective razor.[6]
Now let’s take a closer look at the medication grid for heparin in Table 6.12a.[7]
Table 6.12a Heparin Medication Grid
| Class/
Subclass |
Prototype-
generic |
Administration Considerations | Therapeutic Effects | Adverse/Side Effects |
|---|---|---|---|---|
| Anticoagulant | heparin | Injection (subq) or IV
Carefully examine all heparin products to confirm the correct choice prior to administration Closely monitor PTT levels in IV therapy to ensure in therapeutic range Protamine sulfate is the reversal agent |
Prevent or treat clots | High risk of bleeding
Risk of gastrointestinal or cerebral hemorrhage, especially in elderly Risk of Heparin-Induced Thrombocytopenia (HIT) and Heparin-Induced Thrombocytopenia and Thrombosis (HITT) |
Low Molecular Weight Heparin (LMWH)
Enoxaparin (Lovenox) is a low molecular weight heparin (LMWH) that is supplied in a prefilled syringe (see Figure 6.26).[8] LMWH heparin formulations do not require lab monitoring.

Mechanism of Action
Enoxaparin is a low molecular weight heparin, which has antithrombotic properties with a higher ratio of anti-Factor Xa to anti-Factor IIa activity compared to heparin.
Indications for Use
It is indicated for the prevention and treatment of deep vein thrombosis (DVT), which may lead to pulmonary embolism (PE). It is also used in combination with aspirin for the treatment of acute myocardial infarction.
Nursing Considerations Across the Lifespan
Enoxaparin is administered subcutaneously and preferably in the abdomen for best absorption.
Safety and effectiveness have not been established in pediatric patients. The risk of bleeding increases with age, especially if used concurrently with antiplatelet medications.
Use with caution in patients with renal impairment; risk of bleeding is increased. A dosage adjustment is recommended for patients with severe renal impairment.
Overdosage can be neutralized with a slow IV infusion of protamine sulfate.
Adverse/Side Effects
Black Box Warning: Epidural or spinal hematomas may occur in patients who are anticoagulated with low molecular weight heparins (LMWH) and are receiving neuraxial anesthesia or undergoing spinal puncture. These hematomas may result in long-term or permanent paralysis.
There is a risk of bleeding and hemorrhaging, especially following percutaneous coronary revascularization procedures or with concurrent medication conditions such as recent GI ulcer. It may cause Heparin-Induced Thrombocytopenia (HIT) or Heparin-Induced Thrombocytopenia with Thrombosis (HITT).[9]
Patient Teaching & Education
Notify health care staff immediately of new signs of bleeding or bruising. Remind physicians and dentists that they are receiving heparin before any surgery or invasive procedure is scheduled.[10] Patients should avoid medications containing aspirin or NSAIDS.[11]
Now let’s take a closer look at the medication grid on enoxaparin in Table 6.12b.[12]
Table 6.12b Enoxaparin Medication Grid
| Class/
Subclass |
Prototype-
generic |
Administration Considerations | Therapeutic Effects | Adverse/Side Effects |
|---|---|---|---|---|
| Anticoagulant | enoxaparin | Use with caution in patients with kidney disease.
If used for a patient undergoing neuraxial anesthesia or a spinal puncture, monitor frequently for neurological impairment. If neurological compromise is noted, urgent treatment is necessary |
Prevention or treatment of DVT or PE | Bleeding
Risk of hemorrhage Thrombocytopenia, HIT, or HITT |
Warfarin
Warfarin (Coumadin) is an oral anticoagulant formulated in various strengths in different colors to help prevent errors when patients self-administer different dosages at home (see Figure 6.27[14]). Close monitoring of prothrombin time (PT) or international normalized ratio (INR) is required.

Mechanism of Action
Warfarin acts by inhibiting the synthesis of vitamin K-dependent clotting factors, which include Factors II, VII, IX, and X and the anticoagulant proteins C and S.
Indications for Use
Warfarin is indicated for the following:
- Prophylaxis and treatment of venous thrombosis and its extension, pulmonary embolism (PE).
- Prophylaxis and treatment of thromboembolic complications associated with atrial fibrillation (AF) and/or cardiac valve replacement.
- Reduction in the risk of death, recurrent myocardial infarction (MI), and thromboembolic events such as stroke or systemic embolization after myocardial infarction.
Nursing Considerations Across the Lifespan
Warfarin is contraindicated in pregnant women except for those with mechanical heart valves; it can cause fetal harm.
Vitamin K is the reversal agent. Fresh frozen plasma may be considered if the requirement to reverse the effects of warfarin sodium is urgent.
Close monitoring of prothrombin time (PT) or international normalized ratio (INR) is required. Therapeutic INR ranges from 2.0 to 3.5, depending on the indication.
In hospitalized patients receiving heparin therapy, there is often a period of overlap where the patient is prescribed both IV heparin and warfarin until the INR reaches therapeutic range. At that point, the IV heparin is discontinued.
Warfarin has significant interactions with many medications; read drug label information before administering.
Warfarin sodium is contraindicated in patients with many conditions, including, but not limited to:
- Hemorrhagic tendencies or blood dyscrasias
- Recent or contemplated surgery of the central nervous system or eye, or traumatic surgery resulting in large open surfaces
Bleeding tendencies associated with:
- Active ulceration or overt bleeding of the gastrointestinal, genitourinary, or respiratory tracts
- Central nervous system hemorrhage
- Cerebral aneurysms and dissecting aorta
- Pericarditis and pericardial effusions
- Bacterial endocarditis
Adverse/Side Effects
- Black Box Warnings: Warfarin can cause major or fatal bleeding. Perform regular monitoring of INR in all treated patients. Drugs, dietary changes, and other factors affect INR levels achieved with warfarin therapy. Instruct patients about prevention measures to minimize risk of bleeding and to report signs and symptoms of bleeding. Warfarin can cause acute kidney injury and bleeding risks are increased in patients with liver disease.
Patient Education
Advise patients to:
- Avoid alcohol, cranberries, and grapefruit as they increase the effect of warfarin and the risk for bleeding.
- Strictly adhere to the prescribed dosage schedule.
- Follow INR monitoring guidelines as provided by the prescriber.
- Avoid any activity or sport that may result in traumatic injury.
- Tell their provider if they experience frequent falls because warfarin can increase their risk for bleeding in the brain.
- Eat a normal, balanced diet to maintain a consistent intake of vitamin K (such as green, leafy vegetables).
- Tell all health care professionals and dentists that they are taking warfarin, especially before surgery or dental procedures.
- Use electric razors instead of straight razors.
- Carry identification stating that they are taking warfarin.
- Notify their provider immediately if any unusual bleeding or symptoms occur, such as pain, swelling or discomfort, prolonged bleeding from cuts, increased menstrual flow or vaginal bleeding, nosebleeds, bleeding of gums from brushing, unusual bleeding or bruising, red or dark brown urine, red or tar black stools, headache, dizziness, or weakness.[15]
Now let’s take a closer look at the medication grid on warfarin in Table 6.12c.[16]
Table 6.12c Warfarin Medication Grid
| Class/
Subclass |
Prototype-
generic |
Administration Considerations | Therapeutic Effects | Adverse/Side Effects |
|---|---|---|---|---|
| Anticoagulant | warfarin | Oral route
Vitamin K is the antidote Monitor INR results before administering medication Use with caution in patients with liver disease |
Prevent DVT or PE | Bleeding
Hemorrhage |
Critical Thinking Activity 6.12

A patient who was treated in the hospital for DVT in his left leg has been prescribed warfarin.
1. The patient asks, “Will the warfarin dissolve the clot in my leg?” What is the nurse’s best response?
The nurse plans to assess the patient’s lab work before administering the warfarin.
2. What blood test(s) are important to monitor for patients taking warfarin, and what is the therapeutic range?
The nurse knows that the patient will need to monitor his diet when taking warfarin.
3. What dietary instructions should be provided to the patient?
The nurse plans to provide patient education regarding this newly prescribed medication.
4. Outline the topics to cover with this high-risk medication.
5. What is the reversal agent for warfarin?
Note: Answers to the Critical Thinking activities can be found in the “Answer Key” sections at the end of the book.
Rivaroxaban
Rivaroxaban (Xarelto) is a selective Xa inhibitor.
Mechanism of Action
Rivaroxaban is a selective inhibitor of factor Xa and indirectly inhibits platelet aggregation induced by thrombin.
Indications for Use
Rivaroxaban is indicated for prevention or treatment of DVT and PE. In combination with aspirin, it is indicated to reduce the risk of major cardiovascular events such as cardiovascular (CV) death, myocardial infarction (MI) and stroke and in patients with chronic coronary artery disease (CAD) or peripheral artery disease (PAD).
Nursing Considerations Across the Lifespan
For overdose, activated charcoal can be used to reduce absorption and Andexxa is a reversal agent.
Avoid in patients with moderate to severe liver impairment. Report any unusual bleeding or bruising.
Adverse/Side Effects
Black Box Warning: Epidural or spinal hematomas may occur in patients who are anticoagulated with rivaroxaban and are receiving neuraxial anesthesia or undergoing spinal puncture. These hematomas may result in long-term or permanent paralysis.
Risk of bleeding can be fatal.[17]
Patient Teaching & Education
Patients should report any signs of unusual bleeding or bruising to the healthcare provider. The patient should also notify the provider of all prescriptions, OTC medications, vitamins, and herbal products.[18]
Now let’s take a closer look at the medication grid on rivaroxaban in Table 6.12d.[19]
Table 6.12d Rivaroxaban Medication Grid
| Class/
Subclass |
Prototype-
generic |
Administration Considerations | Therapeutic Effects | Adverse/Side Effects |
|---|---|---|---|---|
| Selective Xa Inhibitors | rivaroxaban | Activated charcoal or Andexxa can be used in overdose
Avoid in patients with liver impairment |
Prevent DVT and PE and and risk of severe cardiovascular events | Bleeding
Epidural or spinal hematomas if neuraxial anesthesia or spinal puncture |
Dabigatran
Dabigatran (Pradaxa) is a direct-acting thrombin inhibitor.
Mechanism of Action
Dabigatran is a competitive, direct thrombin inhibitor. Because thrombin enables the conversion of fibrinogen into fibrin during the coagulation cascade, its inhibition prevents the development of a thrombus.
Indications for Use
This drug is used to prevent or treat deep vein thromboses (DVT) or pulmonary emboli (PE).
Nursing Considerations Across the Lifespan
Overdose: Idarucizumab, a specific reversal agent, is available.
Safety and effectiveness in pediatric patients have not been established.
Adverse/Side Effects
Black Box Warning: Epidural or spinal hematomas may occur in patients who are anticoagulated with dabigatran and are receiving neuraxial anesthesia or undergoing spinal puncture. These hematomas may result in long-term or permanent paralysis.
Risk of bleeding can be fatal.[20]
Patient Teaching & Education
Patients should report any signs of unusual bleeding or bruising to the healthcare provider. Additionally, dabigatran bottles should be disposed of four months after opening. The patient should also notify the provider of all prescriptions, OTC medications, vitamins, and herbal products.[21]
Now let’s take a closer look at the medication grid for dabigatran in Table 6.12e.[22]
Table 6.12e Dabigatran Medication Grid
| Class/
Subclass |
Prototype-
generic |
Administration Considerations | Therapeutic Effects | Adverse/Side Effects |
|---|---|---|---|---|
| Direct-acting thrombin inhibitors | dabigatran | Idarucizumab is a specific reversal agent | Prevent or treat DVT or PE | Risk of bleeding that can be fatal
Epidural or spinal hematomas if receiving neuraxial anesthesia or undergoing spinal puncture |
Antiplatelets
Acetylsalicylic acid (aspirin) and clopidogrel (Plavix) are antiplatelet medications.
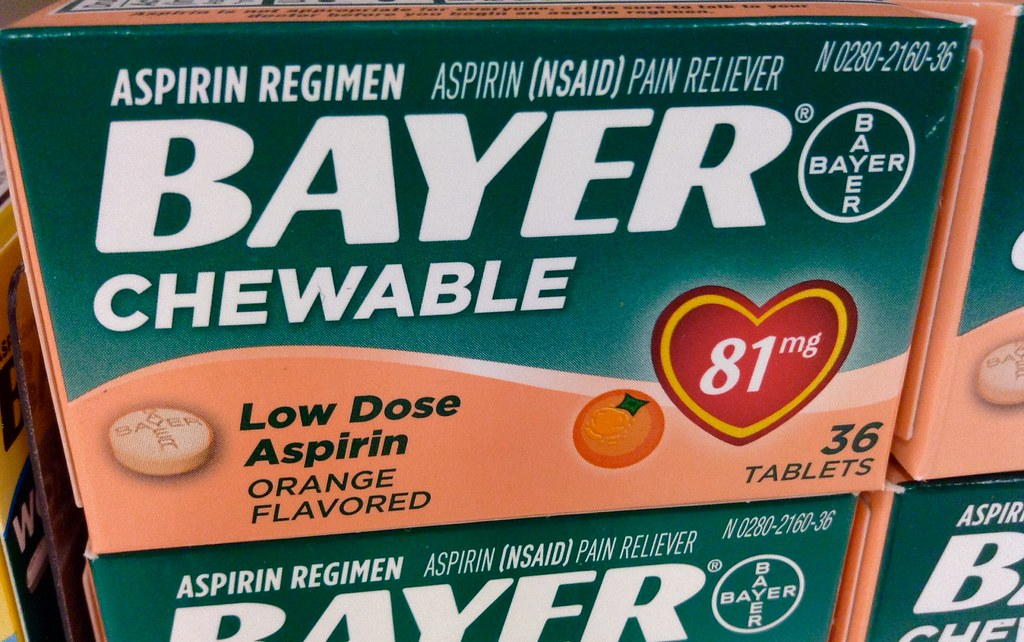
During an active myocardial infarction (heart attack), chewable aspirins are used due to their rapid absorption (see Figure 6.28[23]).
Mechanism of Action
Aspirin inhibits platelet activation and aggregation.
Indications for Use
Aspirin is indicated in patients with established peripheral arterial disease or a history of recent myocardial infarction (MI) or stroke to reduce the rate of MI and stroke. It is also indicated to reduce the rate of myocardial infarction (MI) and stroke in patients with ST-elevation and non–ST-segment elevation ACS.
Nursing Considerations Across the Lifespan
It is important to remember that the effects of these medications last the life of the platelet (7-10 days), so aspirin will need to be withheld for several days before surgery or certain procedures to prevent excessive bleeding. In elderly patients, there is an increased risk of bleeding events with concurrent use of clopidogrel plus aspirin. Aspirin is contraindicated in children under the age of 12 with flu-like symptoms due to the risk of Reye’s syndrome.
Overdose is irreversible.
Clopidogrel is metabolized to its active metabolite by CYP2C19. Concomitant use of drugs that inhibit the activity of this enzyme results in reduced plasma concentrations of the active metabolite of clopidogrel and a reduction in platelet inhibition.
Adverse/Side Effects
Increased risk of bleeding.
Black Box Warning: Reduced effectiveness for patients referred to as “CYP2C19 poor metabolizers.”
Patient Teaching & Education
Patients should report tinnitus, unusual bleeding of the gums, bruising, or blood in the stool to the healthcare provider immediately. While on antiplatelet therapy, patients should avoid alcohol to prevent gastric irritation. Additionally, patients should avoid NSAIDs while receiving antiplatelet therapy.[24]
Now let’s take a closer look at the medication grid for acetylsalicylic acid and clopidogrel in Table 6.12f.[25]
Table 6.12f Acetylsalicylic Acid and Clopidogrel Medication Grid
| Class/
Subclass |
Prototype-
generic |
Administration Considerations | Therapeutic Effects | Adverse/Side Effects |
|---|---|---|---|---|
| Antiplatelets | acetylsalicylic acid (Aspirin) | Administer with food to reduce risk of GI upset and bleeding
Monitor for bleeding Effects last for 7-10 days |
Reduce risk of MI and stroke | Increased risk of bleeding |
Alteplase (tPA)
Alteplase (tPA) is a thrombolytic used to break up clots. It has a very short half-life of 5 minutes so it can open a clogged artery rapidly. It is often given with heparin to prevent reocclusion of the affected blood vessel. There is also a smaller dosage form that is used to flush clogged IV or arterial lines.[26]
Mechanism of Action
Alteplase binds to fibrin in a thrombus and converts the entrapped plasminogen to plasmin, thus breaking down the clot.
Indications for Use
Alteplase is indicated for the acute treatment of myocardial infarction (MI), stroke, or massive pulmonary embolism (PE). It is also used to clear central lines such as a peripherally inserted central line catheter (PICC).
Nursing Considerations Across the Lifespan
The drug is contraindicated in situations in which the risk of significant bleeding is greater than the potential benefit such as:
- Active internal or intracranial bleeding
- History of recent stroke
- Recent (within 3 months) intracranial or intraspinal surgery or serious head trauma
- Presence of intracranial conditions that may increase the risk of bleeding (e.g., some neoplasms, arteriovenous malformations, or aneurysms)
- Current severe uncontrolled hypertension
Significant post-administration monitoring is performed due to the risk of life-threatening bleeding.
Adverse/Side Effects
This drug can cause significant, sometimes fatal, internal or external bleeding, especially at arterial and venous puncture sites. Avoid intramuscular injections and perform venipunctures carefully and only as required. It can increase the risk of thrombo-embolic events in patients with high likelihood of left heart thrombus, such as patients with atrial fibrillation.
Patient Teaching & Education
Patients must institute bleeding precautions to prevent complications of therapy.[27]
Now let’s take a closer look at the medication grid for alteplase in Table 6.12g.[28]
Table 6.12g Alteplase Medication Grid
| Class/
Subclass |
Prototype-
generic |
Administration
Considerations |
Therapeutic Effects | Adverse/Side Effects |
|---|---|---|---|---|
| Thrombolytic | alteplase (tPA) | Contraindicated in many conditions where the risk of bleeding outweighs the potential benefit | Break down a life-threatening clot in MI, stroke, or massive PE | Risk of severe bleeding that can be fatal |
- Institute for Safe Medication Practices (ISMP). (2018). ISMP List of High-Alert Medications in Acute Care Settings. https://www.ismp.org/sites/default/files/attachments/2018-08/highAlert2018-Acute-Final.pdf. ↵
- Anderson, P. & Townsend, T. (2015) Preventing high-alert medication errors in hospital patients. Nurse Today, 10(5). https://www.americannursetoday.com/wp-content/uploads/2015/05/ant5-CE-421.pdf ↵
- Institute for Safe Medication Practices (ISMP). (2017). QuarterWatch™ (2016 Annual Report) Part II: Oral Anticoagulants—The Nation’s Top Risk of Acute Injury from Drugs. https://www.ismp.org/resources/quarterwatchtm-2016-annual-report-part-ii-oral-anticoagulants-nations-top-risk-acute. ↵
- "Heparin Sodium sample.jpg" by LHcheM is licensed under CC BY-SA 3.0 and "Heparin in Dextrose Injection" by Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- This work is a derivative of Daily Med by U.S. National Library of Medicine in the public domain. ↵
- uCentral from Unbound Medicine. https://www.unboundmedicine.com/ucentral ↵
- This work is a derivative of Daily Med by U.S. National Library of Medicine in the public domain. ↵
- "syringe-disposable-syringe-blister-103059" by stux is licensed under CC0 ↵
- This work is a derivative of Daily Med by U.S. National Library of Medicine in the public domain. ↵
- This work is a derivative of Daily Med by U.S. National Library of Medicine in the public domain. ↵
- uCentral from Unbound Medicine. https://www.unboundmedicine.com/ucentral ↵
- This work is a derivative of Daily Med by U.S. National Library of Medicine in the public domain. ↵
- This work is a derivative of Daily Med by U.S. National Library of Medicine in the public domain. ↵
- "Warfarintablets5-3-1.jpg" by Gonegonegone is licensed under CC BY-SA 3.0 ↵
- This work is a derivative of Daily Med by U.S. National Library of Medicine in the public domain. ↵
- This work is a derivative of Daily Med by U.S. National Library of Medicine in the public domain. ↵
- This work is a derivative of Daily Med by U.S. National Library of Medicine in the public domain. ↵
- uCentral from Unbound Medicine. https://www.unboundmedicine.com/ucentral ↵
- This work is a derivative of Daily Med by U.S. National Library of Medicine in the public domain. ↵
- This work is a derivative of Daily Med by U.S. National Library of Medicine in the public domain. ↵
- uCentral from Unbound Medicine. https://www.unboundmedicine.com/ucentral ↵
- This work is a derivative of Daily Med by U.S. National Library of Medicine in the public domain. ↵
- "Bayer Aspirin Low Dose" by Mike Mozart is licensed under CC BY 2.0 ↵
- uCentral from Unbound Medicine. https://www.unboundmedicine.com/ucentral ↵
- This work is a derivative of Daily Med by U.S. National Library of Medicine in the public domain. ↵
- McCuistion, L., Vuljoin-DiMaggio, K., Winton, M, & Yeager, J. (2018). Pharmacology: A patient-centered nursing process approach. pp. 443-454. Elsevier. ↵
- uCentral from Unbound Medicine. https://www.unboundmedicine.com/ucentral ↵
- This work is a derivative of Daily Med by U.S. National Library of Medicine in the public domain. ↵
Any substance that opposes coagulation.
A blood test used to monitor how long it takes for a patient’s blood to clot. Used for patients receiving IV heparin therapy to achieve therapeutic range.
A blood test used to monitor the effects of warfarin.
A blood test used to monitor the effects of warfarin and to achieve therapeutic range, generally between 2.0 and 3.5 based on the indication.

