10.4 Nursing Process for Analgesics and Musculoskeletal Medications
Open Resources for Nursing (Open RN)
Now that we have reviewed basic concepts related to pain and several disorders requiring analgesic or musculoskeletal medication, let’s consider the nursing process and how it applies to these types of medications.
Assessment
Although there are numerous details to consider when administering medications, it is important to always first think about what you are giving and why?
First, let’s think of why?
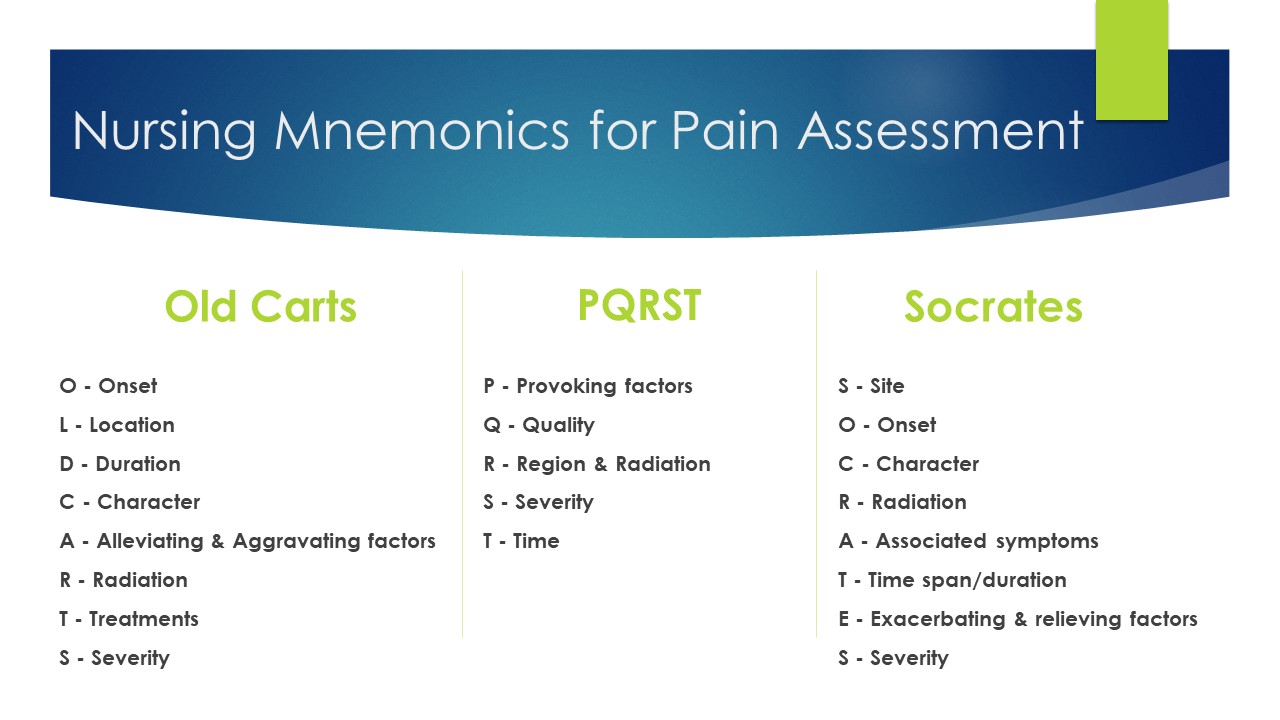
Analgesic medications are given to alleviate pain. An important piece of your nursing assessment should be to assess the patient’s pain level. The patient’s pain level is what the patient says it is. This is accomplished by using a pain scale. Always find out the acceptable pain level for your patient. See Figure 10.5[1] for common nursing mnemonics for pain assessment.
Visual pain scales have been developed as a tool of communication about pain with children through patients at end of life. See Figure 10.6[2] for the FACES Pain Rating Scale. To use this scale, use the following evidence-based instructions. Explain to the patient that each face represents a person who has no pain (hurt), some, or a lot of pain. “Face 0 doesn’t hurt at all. Face 2 hurts just a little. Face 4 hurts a little more. Face 6 hurts even more. Face 8 hurts a whole lot. Face 10 hurts as much as you can imagine, although you don’t have to be crying to have this worst pain.” Ask the person to choose the face that best represents the pain they are feeling.
Additional baseline information to collect prior to administration of any analgesic or musculoskeletal medication includes any history of allergy or previous adverse response.
![Wong-Baker FACES Foundation (2020). Wong-Baker FACES® Pain Rating Scale. Retrieved [Date] with permission from http://www.WongBakerFACES.org Image of Wong-Baker FACES pain rating scale](https://wtcs.pressbooks.pub/app/uploads/sites/10/2019/12/image6.png)
Figure 10.6. The Wong-Baker FACES Pain Rating Scale. Used with permission from http://www.WongBakerFACES.org.
Implementation of Interventions
With the administration of analgesic or musculoskeletal medications, it is important to always perform the five rights (right patient, medication, dose, route, and time) and to check for allergies prior to administration. Prior to administration, it is important to consider the best route of administration for this patient at this particular time. For example, if the patient is nauseated and vomiting, then an oral route may not be effective. See Figure 10.7 for a list of common opioid medications ranging from use for moderate to severe pain.[3] When administering opioid medications, it is important to remember that these medications are controlled substances with special regulations regarding storage, auditing counts, and disposal or wasting of medication. See more information about controlled substances in the “Legal/Ethical” chapter.
Common Opioid Analgesics
Generic Name |
Trade Name(s) |
Route |
Adult Dosage |
|---|---|---|---|
| codeine/acetaminophen | Tylenol #3 | PO | 30 mg/300 mg |
| fentanyl | Duragesic
Sublimaze |
Transdermal
IM IV |
12 mcg-100mcg/hr
0.5-1 mcg/kg 0.5-1 mcg/kg |
| hydrocodone/acetaminophen | Lortab
Norco Vicodin |
PO
PO PO |
5 mg/300mg or 325 mg
10 mg/320mg or 325 mg
|
| hydromorphone | Dilaudid | PO
Rectal SubQ, IM & IV |
4-8 mg
3 mg 1.5 mg (may be increased) |
| morphine | Duramorph, MS Contin, Oramorph SR, & Roxanol-T | PO & Rectal
SubQ, IM, & IV |
30 mg (may be increased)
4-10 mg (may be increased) |
| oxycodone
oxycodone/acetaminophen |
Oxy IR, Oxycontin & Oxy-FAST
Percocet & Roxicet |
PO
PO |
5 mg-10 mg (may be increased)
5 mg/325 mg |
Figure 10.7 Table of Common Opioid Analgesics
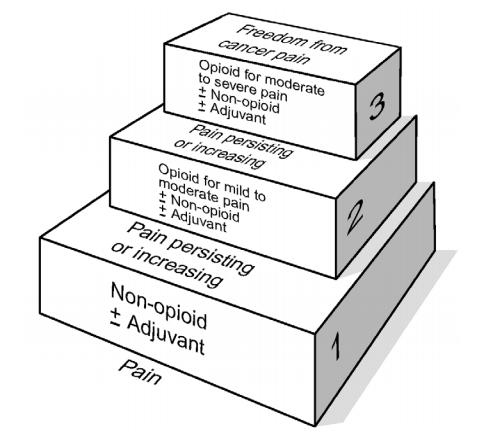
A general rule of thumb when administering analgesics is to use the least invasive medication that is anticipated to treat the level of pain reported by the patient. The WHO ladder was originally developed for selection of analgesics for patients with cancer but illustrates the concept that pain control should be based on the level indicated by the patient. See Figure 10.8[4] for an image of the WHO ladder. For example, if a patient reports a pain level of “2,” then it is appropriate to start at the lowest rung of the ladder and administer a non-opioid. However, it may be clinically indicated to start at “Level 3” on the WHO ladder for patients who present with severe, difficult pain.
It is important to anticipate any common side effects and the expected outcome of the medication, as well as considerations regarding what to teach the patient and their family regarding the medications.
Evaluation
It is important to always evaluate the patient’s response to the medication. With analgesic medications, the nurse should assess for decrease in pain 30 minutes after IV administration and 60 minutes after oral medication. If the patient’s pain level is not acceptable, the nurse should investigate alternate treatment modalities. These modalities may include, but not limited to, aromatherapy, repositioning the patient, hot or cold treatments, and listening to music. As the nurse is the patient advocate, the healthcare provider may have to be informed if the patient’s pain is not being controlled by analgesics. One of the adverse effects of opioid analgesics is respiratory depression. The nurse should evaluate the respiratory rate and pulse oximetry after administration of the medication. Other common side effects of opioid analgesic medications are constipation or nausea. The nurse may need to consider administering other medications that treat the side effects of analgesic medication.
- "Mnemonics for Pain Assessment" by Julie Teeter is licensed under CC BY-SA 4.0 ↵
- Wong-Baker FACES Foundation (2020). Wong-Baker FACES® Pain Rating Scale. Retrieved [2020] with permission from http://www.WongBakerFACES.org ↵
- Vallerand, A. & Sanoski, C. A. (2019). Davis’s Drug Guide for Nurses (16th ed.). F.A. Davis Company. ↵
- World Health Organization. Cancer pain relief. 2nd ed. Geneva: WHO; 1996. ↵

