8.3 Disorders of the CNS System
Open Resources for Nursing (Open RN)
Now that we have reviewed basic concepts of neurotransmitters and their function, let’s review common CNS disorders.
Additional supplementary videos about mental disorders are available at:
Khan Academy[1]
Anxiety
Anxiety disorders are a group of conditions marked by pathological or extreme anxiety or dread. People with anxiety experience disturbances of mood, behavior, and most systems in the body, making them unable to continue with everyday activities. Many feel anxious most of the time for no apparent reason.[2]
Anxiety is different from fear. Fear is a person’s response to an event or object. The psychiatric disorder of anxiety occurs when the intensity and duration of anxiety does not match the potential for harm or threat to the affected person. Anxiety can be expressed with physical symptoms or behaviorally.[3]
Signs and Symptoms of Anxiety
- Aches
- Pains
- Stomach aches
- Headaches
- Heart racing or pounding
- Trembling
- Sweating
- Difficulty concentrating (see Figure 8.5)[4]
- Increased agitation
- Crying [5],[6]

Treatment can include non-pharmacological interventions as well as medications. Non-pharmacological interventions to decrease anxiety include relaxation techniques such as deep breathing, exercise, psychotherapy, support groups, or cognitive behavioral therapy. Anti-anxiety medications can also be used to help both verbal and nonverbal clients feel a much-needed sense of peace. [7],[8]
Learn more about anxiety from the National Institute of Mental Health’s website.
Depression
Depression is a frequent problem, affecting up to 5% of the population. To be diagnosed with depression, five of the following symptoms must be present during the same two-week period and represent a change from previous functioning. The symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning. The symptoms of depression cannot be due to effects of a substance or from bereavement.[9]
Signs and Symptoms of Depression
- Depressed mood
- Diminished interest
- Weight loss when not dieting or weight gain
- Insomnia or hypersomnia
- Agitation
- Fatigue or loss of energy
- Feeling of worthlessness
- Inappropriate guilt
- Diminished ability to concentrate
- Recurrent thoughts of death, suicidal ideation, or suicide attempt[10],[11]
Treatment of depression may include medication, psychotherapy, cognitive therapy, electroconvulsive therapy (ECT), and group therapy. Patients who are depressed may not report symptoms unless specifically asked, and they may be suicidal. Using assessment techniques to gather information about the history of each patient’s depression, support system, specific triggering events, psychosocial assessment, and risk for harm to self or others is imperative. Each patient’s response to medication is unpredictable, and often medications will need to be adjusted based on reported symptoms.[12],[13]
Learn more about depression from the National Institute of Mental Health’s website.
Bipolar
Bipolar affective disorder is marked by serious mood swings. Typically, patients experience extreme highs (called mania or hypomania) alternating with extreme lows (depression). See the “Depression” section for signs and symptoms of depression. People feel normal only in the periods between the highs and lows. For some people, the cycles occur so rapidly that they hardly ever feel a sense of control over their mood swings.[14]
Signs and Symptoms of a Manic Episode
- Rapid speech
- Hyperactivity
- Reduced need for sleep
- Flight of ideas
- Grandiosity
- Poor judgement
- Aggression/hostility
- Risky sexual behavior
- Neglect basic self-care
- Decreased impulse control [15],[16]
Treatment for a patient diagnosed with bipolar may include medication, safety initiatives during acute mania, ECT, psychotherapy, and support groups. The severity of manic and depressive episodes varies for each patient. Assessing if a patient is a danger to others or themselves is the priority. People with bipolar may need assistance with impulse control during times when they are in a manic state.[17]
Learn more about bipolar disorder from the National Institute of Mental Health’s website.
Schizophrenia
Schizophrenia affects people from all walks of life and usually first appears between the ages of 15 and 30. Not everyone will experience the same symptoms, but many symptoms are common such as withdrawing, hearing voices, talking to oneself, seeing things that are not there, neglecting personal hygiene, and showing low energy.[18]
Schizophrenia refers to a group of severe, disabling psychiatric disorders marked by withdrawal from reality, illogical thinking, delusions (fixed false beliefs that cannot be changed through reasoning), hallucinations (hearing, seeing, smelling, tasting, or feeling touched by things that are not there), and flat affect (lack of observable expressions of emotions, monotone voice, expressionless face, immobile body).[19]
Signs and Symptoms of Schizophrenia
There are three types of symptoms related to schizophrenia: positive, negative, and cognitive.
Positive Symptoms
Note that in this context, the word positive is not the same as good. Rather, positive symptoms are psychotic and demonstrate how the individual has lost touch with reality. Positive symptoms include:
- Delusions
- Hallucinations
- Disorganized thinking and behavior
Delusions fall into several categories. Individuals with a persecutory delusion may believe they are being tormented, followed, tricked, or spied on. Individuals with a grandiose delusion may believe they have special powers. Individuals with a reference delusion may believe that passages in books, newspapers, television shows, song lyrics, or other environmental cues are directed toward them. In delusions of thought withdrawal or thought insertion, individuals believe others are reading their mind, their thoughts are being transmitted to others, or outside forces are imposing their thoughts or impulses on them.[20]
Hallucinations may include hearing, seeing, smelling, tasting, or feeling as if they have been touched by things that are not there.[21]
Negative Symptoms
Negative symptoms are those characteristics that should be there but are lacking. Negative symptoms include:
- Apathy (lack of interest in people, things, activities)
- Lack of motivation
- Blunted affect
- Poverty of speech (brief replies)
- Anhedonia (lack of interest in activities once enjoyed)
- Avoidance of relationships
Keep in mind that the inability to show emotion associated with a blunted affect does not reflect an inability to feel emotion. Similarly, it is helpful to understand that withdrawing from others is a coping mechanism for an individual with schizophrenia and not a rejection of those who initiate contact.[22]
Cognitive
Cognitive symptoms are a change in thought pattern and include:
- Poor decision making
- Loss of memory
- Distracted
- Difficulty focusing
Treatment for a patient diagnosed with schizophrenia may include medications to control positive and/or negative signs and symptoms and nonpharmacological interventions such as limit setting, therapeutic communication, ECT, and psychotherapy. Key assessments for a patient with schizophrenia include examination for hallucinations and delusions, use of additional substances (alcohol or drugs), safety, their support system, and a medication review with a focus on compliance with their therapeutic regimen. [23],[24],[25]
Learn more about schizophrenia from the National Institute of Mental Health’s website.
Attention-Deficit / Hyperactivity Disorder
Attention-deficit/hyperactivity disorder (ADHD) is characterized by hyperactivity, lack of impulse control, and/or lack of attention that interferes with how a person functions. ADHD is often diagnosed during childhood, but signs and symptoms can last through adulthood.
Signs and Symptoms of ADHD
- Hyperactivity
- Inability to concentrate(see Figure 8.6)[26]
- Difficulty with self-control
- Lack of emotional control
A child with ADHD may have difficulty sitting still and focusing at school or have emotional outbursts. These behaviors often impact their life. Medication, psychotherapy, behavior management, and family support all play a large part in helping an individual with ADHD. Additional resources for parents are also helpful.[27],[28]
Learn more about ADHD from the National Institute of Mental Health’s website.
Seizures
The official definition of a seizure is “a transient occurrence of signs and/or symptoms due to an abnormal excessive or synchronous neuronal activity in the brain.” This means that during a seizure, large numbers of brain cells are activated abnormally at the same time. It is like an electrical storm in the brain. They may alter consciousness and produce abnormal motor activity. There are different classifications of seizures based on severity of symptoms.[29]
Signs and Symptoms of Seizures
Motor Symptoms
- Jerking (clonic)
- Muscles becoming limp or weak (atonic)
- Tense or rigid muscles (tonic)
- Brief muscle twitching (myoclonus)
- Epileptic spasms
Non-motor Symptoms
- Changes in sensation, emotions, thinking, or autonomic functions
- Lack of movement
Classification of Seizures
Seizures are classified in many ways, beginning with whether they are partial or generalized seizures.
Partial Seizures
Partial seizures have focal onset on one side of the brain. They are further classified into simple, complex, or secondarily generalized:
- Simple partial seizures are most common. They may also affect sensory and autonomic systems.
- Complex partial seizures include impairment of consciousness, with or without motor activity or other signs.
- Simple or complex partial seizures may become secondarily generalized, producing a tonic-clonic seizure.
Generalized Seizures
Generalized seizures have bilateral onset on both sides of the brain and are typified by petit mal seizures, which can be recognized by clinical characteristics as well as interictal EEG abnormalities. [30],[31],[32],[33]
Status Epilepticus
Status epilepticus is a state of repeated or continuous seizures. It is often defined operationally as a single seizure lasting more than 20 minutes or repeated seizures without recovery of consciousness. Prolonged status epilepticus leads to irreversible brain injury and has a very high rate of mortality. The goal of therapy should be to achieve control of a seizure within 60 minutes or less. Pharmacological treatment of seizures is very successful in the majority of cases, but it requires accurate diagnosis and classification of seizures. Medication management of seizures may include CNS depressants, benzodiazepines or barbiturates, or anticonvulsants such as phenytoin.[34]
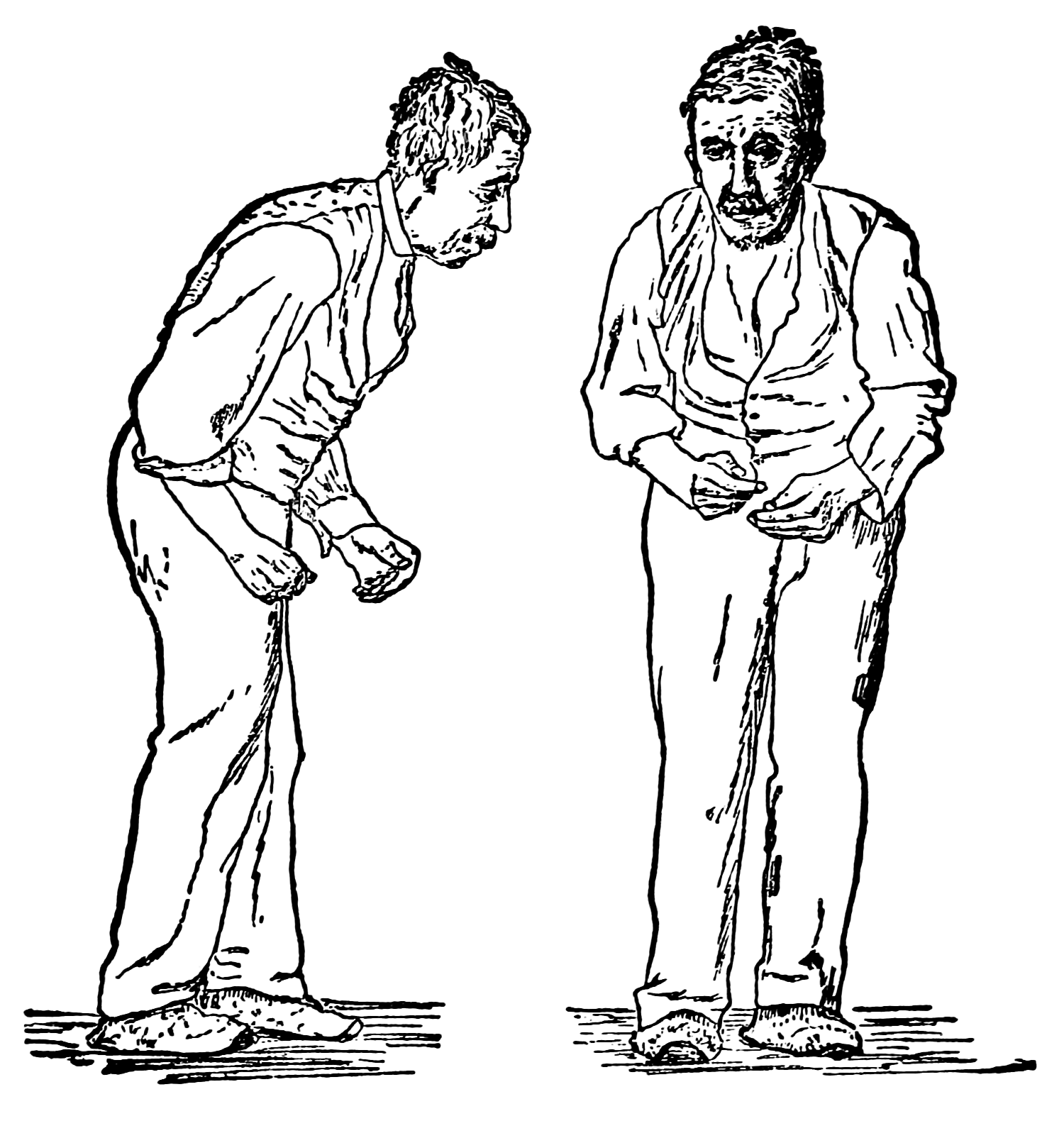
Parkinson’s Disease
Parkinson’s disease is a progressive disease of the nervous system that impairs one’s ability to move. The typical onset for Parkinson’s disease is middle to later stages of life. This disease worsens over time and has no cure. The cause of this disease is unknown, but it is known that it is characterized by a loss of dopaminergic neurons.[35],[36]
Signs and Symptoms of Parkinson’s Disease
- Tremor at rest
- Bradykinesia
- Muscle rigidity
- Postural instability
- Gait disturbance
- Dystonia
- Ophthalmoplegia
- Active mood disorders
See Figure 8.7 for a typical posture associated with Parksinon’s disease.[37] Treatment for a patient with Parkinson’s disease often includes medication to increase dopamine in the brain to slow the progression of the disease.
Potential new treatment of proteins in Alzheimers and Parkinson’s disease
The underlying cause of some neurodegenerative diseases, such as Alzheimer’s and Parkinson’s, appears to be related to proteins—specifically, to proteins behaving badly. One of the strongest theories of what causes Alzheimer’s disease is based on the accumulation of beta-amyloid plaques, dense conglomerations of a protein that is not functioning correctly. Parkinson’s disease is linked to an increase in a protein known as alpha-synuclein that is toxic to the cells of the substantia nigra nucleus in the midbrain.
For proteins to function correctly, they are dependent on their three-dimensional shape. The linear sequence of amino acids folds into a three-dimensional shape that is based on the interactions between and among those amino acids. When the folding is disturbed and proteins take on a different shape, they stop functioning correctly. But the disease is not necessarily the result of functional loss of these proteins; rather, these altered proteins start to accumulate and may become toxic. For example, in Alzheimer’s the hallmark of the disease is the accumulation of these amyloid plaques in the cerebral cortex. The term coined to describe this sort of disease is “proteopathy” and it includes other diseases. Creutzfeld-Jacob disease, the human variant of the disease known as mad cow disease, also involves the accumulation of amyloid plaques, similar to Alzheimer’s. Diseases of other organ systems can fall into this group as well, such as cystic fibrosis or type 2 diabetes. Recognizing the relationship between these diseases has suggested new therapeutic possibilities. Interfering with the accumulation of the proteins, and possibly as early as their original production within the cell, may unlock new ways to alleviate these devastating diseases.[38]
- Introduction to Mental Disorders by Khan Academy is licensed under CC BY-NC-SA 3.0. ↵
- This work is a derivative of Supporting Individuals with Intellectual Disability & Mental illness by Sheri Melrose is licensed under CC BY 4.0. ↵
- This work is a derivative of Supporting Individuals with Intellectual Disability & Mental illness by Sheri Melrose is licensed under CC BY 4.0. ↵
- "stress-2902537_960_720.jpg" by TheDigitalArtist is licensed under CC0 1.0 ↵
- This work is a derivative of Supporting Individuals with Intellectual Disability & Mental illness by Sheri Melrose is licensed under CC BY 4.0. ↵
- Mayo Clinic Staff. (2018, May 4). Anxiety disorders. https://www.mayoclinic.org/diseases-conditions/anxiety/symptoms-causes/syc-20350961 ↵
- This work is a derivative of Supporting Individuals with Intellectual Disability & Mental illness by Sheri Melrose is licensed under CC BY 4.0. ↵
- McCuistion, L., Vuljoin-DiMaggio, K., Winton, M, & Yeager, J. (2018). Pharmacology: A patient-centered nursing process approach. pp. 227-305) ↵
- This work is a derivative of Principles of Pharmacology by LibreTexts licensed under CC BY-NC-SA 4.0. ↵
- This work is a derivative of Daily Med by U.S. National Library of Medicine in the public domain. ↵
- Mayo Clinic Staff. (2018, February 3). Depression. https://www.mayoclinic.org/diseases-conditions/depression/symptoms-causes/syc-20356007 ↵
- This work is a derivative of Principles of Pharmacology by LibreTexts licensed under CC BY-NC-SA 4.0. ↵
- Varcarolis, E. M. (2017). Essentials of psychiatric mental health nursing: a communication approach to evidence-based care. pp. 255-324. Elsevier. ↵
- This work is a derivative of Supporting Individuals with Intellectual Disability & Mental illness by Sheri Melrose is licensed under CC BY 4.0. ↵
- This work is a derivative of Supporting Individuals with Intellectual Disability & Mental illness by Sheri Melrose is licensed under CC BY 4.0. ↵
- Mayo Clinic Staff. (2018, January 31)) Bipolar disorder. https://www.mayoclinic.org/diseases-conditions/bipolar-disorder/symptoms-causes/syc-20355955 ↵
- Varcarolis, E. M. (2017). Essentials of psychiatric mental health nursing: a communication approach to evidence-based care. pp. 255-324. Elsevier. ↵
- This work is a derivative of Supporting Individuals with Intellectual Disability & Mental illness by Sheri Melrose is licensed under CC BY 4.0. ↵
- This work is a derivative of Supporting Individuals with Intellectual Disability & Mental illness by Sheri Melrose is licensed under CC BY 4.0. ↵
- This work is a derivative of Supporting Individuals with Intellectual Disability & Mental illness by Sheri Melrose is licensed under CC BY 4.0. ↵
- This work is a derivative of Supporting Individuals with Intellectual Disability & Mental illness by Sheri Melrose is licensed under CC BY 4.0. ↵
- This work is a derivative of Supporting Individuals with Intellectual Disability & Mental illness by Sheri Melrose is licensed under CC BY 4.0. ↵
- This work is a derivative of Principles of Pharmacology by LibreTexts licensed under CC BY-NC-SA 4.0. ↵
- Varcarolis, E. M. (2017). Essentials of psychiatric mental health nursing: a communication approach to evidence-based care. pp. 255-324. Elsevier. ↵
- Mayo Clinic Staff. (2020, January 7) Schizophrenia. https://www.mayoclinic.org/diseases-conditions/schizophrenia/diagnosis-treatment/drc-20354449 ↵
- "RightBrainDominant.jpg" by ElisaRiva is licensed under CC0 ↵
- Mayo Clinic Staff. (2019, June 25). Attention-deficit/hyperactivity disorder (ADHD) in children. https://www.mayoclinic.org/diseases-conditions/adhd/symptoms-causes/syc-20350889 ↵
- McCuistion, L., Vuljoin-DiMaggio, K., Winton, M, & Yeager, J. (2018). Pharmacology: A patient-centered nursing process approach. pp. 227-305. Elsevier. ↵
- Epilepsy Foundation. (2016, December 22). 2017 Revised classification of seizures. https://www.epilepsy.com/article/2016/12/2017-revised-classification-seizures ↵
- This work is a derivative of Principles of Pharmacology by LibreTexts licensed under CC BY-NC-SA 4.0. ↵
- This work is a derivative of Pharmacology Notes: Nursing Implications for Clinical Practice by Gloria Velarde licensed under CC BY-NC-SA 4.0. ↵
- Mayo Clinic Staff. (2019, June 18). Seizures. https://www.mayoclinic.org/diseases-conditions/seizure/symptoms-causes/syc-20365711 ↵
- Epilepsy Foundation. (2016, December 22). 2017 Revised classification of seizures. https://www.epilepsy.com/article/2016/12/2017-revised-classification-seizures ↵
- This work is a derivative of Principles of Pharmacology by LibreTexts licensed under CC BY-NC-SA 4.0. ↵
- This work is a derivative of Neuroscience: Canadian 1st Edition by Dr. William Ju and is licensed under CC BY 4.0. ↵
- Mayo Clinic Staff. (2018, June 30). Parkinson’s disease. https://www.mayoclinic.org/diseases-conditions/parkinsons-disease/symptoms-causes/syc-20376055 ↵
- "Paralysis agitans (1907, after St. Leger).png" by William Richard Gowers is licensed under CC0 ↵
- This work is a derivative of Anatomy and Physiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
A state of repeated or continuous seizures.
Usually tremor at rest; When person sits, arm shakes; tremor stops when person attempts to grab something (pill rolling tremor).
Slowness in initiation and execution of voluntary movements.
Increase muscle tone and increase resistance to movement (Arms and Legs Stiff) – as severity increases cogwheel rigidity.
Abnormal fixation of posture (stoop when standing), problems with equilibrium, and righting reflex.
An abnormal way of walking, such as shuffling feet.
Inappropriate and continuous muscle contraction.
Weakness in eye muscles.

