7.4 Treatments for Depression
Depression is one of the most treatable mental disorders. Between 80% and 90% percent of people with depression eventually respond well to treatment. Almost all patients gain some relief from their symptoms with effective treatment. Before a diagnosis is made or treatment planned, a mental health care provider should conduct a thorough diagnostic evaluation, including an interview, mental status examination, psychosocial assessment, and a physical examination performed by a primary care provider. In some cases, a blood test might be done to make sure the depression is not due to a medical condition like a thyroid problem or a vitamin deficiency. The evaluation also explores medical and family histories, cultural beliefs, and environmental factors as part of the psychosocial assessment with the goal of arriving at a diagnosis and planning a course of action. Treatments for depression include medications, psychotherapy, electroconvulsive therapy, transcranial magnetic stimulation, and encouraging self-care and effective coping strategies. Nurses should keep patient-centered care and client preferences in mind when implementing a client’s treatment plan. For example, the client should be educated about the possible adverse effects associated with antidepressant medication, and their ability to pay for and obtain transportation to treatments like psychotherapy should be considered.[1]
Antidepressant Medications
Brain chemistry may contribute to an individual’s depression and may factor into their treatment. Read more about the causes of depression in the “Causes of Depression” section of this chapter. For this reason, providers may prescribe antidepressants to help modify an individual’s brain chemistry.
Antidepressants are used to regulate and increase neurotransmitters in the brain to improve mood. There are several classes of antidepressants with different mechanisms of action and potential adverse side effects. Classes of antidepressants, their mechanism of action, and common side effects are outlined in Table 7.4.[2] Common side effects are listed in this table by frequency of their occurrence. Some medications can cause QTc prolongation, which refers to delayed cardiac electrical conduction that can lead to dysrhythmias. Tricyclic antidepressants (TCAs) and monoamine oxidase inhibitors (MAOIs) often cause anticholingeric side effects (e.g., tachycardia, urinary retention, constipation, dry mouth, blurred vision, confusion, psychomotor slowing, sedation, and delirium). A specific medication class is typically initiated by the provider based on the individual’s symptoms, potential side effects, cost, and family history of success with certain medications.
Review neurotransmitter actions and related central nervous system physiology in the “Psychotropics Medications” chapter.
Table 7.4. Antidepressants
| Medication Class | Mechanism of Action | Common Side Effects
(*Indicates medical emergency) |
|---|---|---|
| Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs)
Common examples: Venlafaxine Duloxetine |
Block the uptake of both serotonin and norepinephrine from the cell synapse. Similar to SSRIs but with two neurotransmitters. |
|
| Selective Serotonin Reuptake Inhibitors (SSRIs)
Common examples: Fluoxetine Sertraline Citalopram |
Impact the receptors of the cell synapse to inhibit or prevent the uptake of serotonin, making the neurotransmitter serotonin stay in the synapse longer. |
*Serotonin syndrome |
| Tricyclic Antidepressants (TCAs)
Common examples: Amitriptyline Nortriptyline |
Block the presynaptic receptor for norepinephrine and partially serotonin. This makes the neurotransmitter norepinephrine level increase in the synapse. |
|
| Monoamine Oxidase Inhibitors (MAOIs)
Common examples: Phenelzine Tranylcypromine |
Block the enzyme that breaks down monoamine, which causes an increase in the level of neurotransmitters serotonin and norepinephrine. |
*Hypertensive crisis |
| Norepinephrine and Dopamine Reuptake Inhibitor (NDRI)
Example: Bupropion |
Blocks the uptake of both norepinephrine and dopamine from the cell synapse. |
|
Antidepressants may produce some improvement within the first week or two, but full benefits may not be seen for two to three months. If a patient feels little or no improvement after several weeks, the mental health care provider can alter the dose of the medication, add another medication, or substitute another antidepressant. In a similar manner, if a client develops ongoing bothersome side effects, the provider can switch them to a different medication. Nurses should encourage clients to contact their mental health care prescriber if a medication is not working within the expected time frame or if they are experiencing ongoing bothersome side effects. It is typically recommended that clients continue to take medication(s) for six or more months after the symptoms have improved. Long-term maintenance therapy may be suggested to decrease the risk of future episodes for people at high risk for recurrence.[3]
Boxed Warning
A Boxed Warning is a significant warning from the Food and Drug Administration (FDA) that alerts the public and health care providers to serious side effects, such as injury or death. Boxed Warnings are in place for all classes of antidepressants used with children, adolescents, and young adults due to a higher risk of suicide. All clients receiving antidepressants should be monitored for signs of worsening depression or changing behavior, especially when the medication is started or dosages changed.
Adverse/Side Effects
Nurses must monitor clients receiving antidepressants for side effects and report concerns to the prescribing provider. Clients should be instructed to immediately call their provider if they have any of the following symptoms, especially if they are new or worsening[4]:
- Thoughts about suicide or dying
- Attempts to commit suicide
- Worsening depression
- Anxiety
- Agitation or restlessness
- Panic attacks
- Trouble sleeping (insomnia)
- Irritability
- Aggression, anger, or violence
- Dangerous impulses
- Increased activity and talking (i.e., signs of mania)
- Other unusual changes in behavior or mood
Serotonin Syndrome
High doses of antidepressants or a combination of medications that affect serotonin, such as antidepressants or triptans (used to treat migraine headaches), can cause a medical emergency called serotonin syndrome. The presentation of serotonin syndrome is extremely variable, ranging from mild symptoms to a life-threatening syndrome. It typically develops within 24 hours from the increased dosage or combination of medications and can be fatal.
Symptoms of serotonin syndrome can be classified into three categories[5],[6],[7]:
- Mental status changes: Agitation, restlessness, or delirium
- Autonomic hyperactivity: Tachycardia, hypertension, hyperthermia, diaphoresis, shivering, vomiting, or diarrhea
- Neuromuscular hyperactivity: Tremor, muscle hypertonia or rigidity, myoclonus, hyperreflexia, or clonus (including rapid, horizontal eye movements)
A mnemonic commonly used to remember the symptoms of serotonin syndrome is SHIVERS:
- S: Shivering: A neuromuscular symptom similar to tremors specific to serotonin syndrome
- H: Hyperreflexia (and myoclonus): Hyperactive reflexes most prominent in the lower extremities
- I: Increased Temperature
- V: Vital Sign Abnormalities: Tachycardia, tachypnea, and labile blood pressure
- E: Encephalopathy: Mental status changes such as agitation, delirium, and confusion
- R: Restlessness
- S: Sweating
People may get slowly worse and can become severely ill if not quickly treated. Untreated, serotonin syndrome can be deadly. With treatment, symptoms usually go away within 24 hours, but permanent kidney damage may result even with treatment. Uncontrolled muscle spasms can cause severe muscle breakdown called rhabdomyolysis. Myoglobin is released into the blood with muscle breakdown and clogs renal tubules, which can cause severe kidney damage if serotonin syndrome isn’t recognized promptly and treated.
Treatment of serotonin syndrome may include the following[8],[9]:
- Stopping all serotonergic medications.
- Providing supportive care to normalize vital signs such as IV fluids, cooling measures, and medications to control heart rate and blood pressure.
- Sedating with benzodiazepines, such as diazepam or lorazepam, to decrease agitation, seizure-like movements, and muscle stiffness.
- If symptoms persist, administering cyproheptadine to block serotonin production.
- For patients with severe symptoms such as hyperthermia and muscle rigidity, more aggressive measures are required. These include sedation, intubation, neuromuscular paralysis, and active cooling techniques.[10]
Clients with moderate to severe serotonin syndrome should be hospitalized for close monitoring and management. Serotonin syndrome, in its most severe form, can resemble neuroleptic malignant syndrome (NMS) caused by antipsychotic medications. However, NMS develops over a period of days to weeks. Neuroleptic malignant syndrome (NMS) will be discussed further in Chapter 11.
Hypertensive Crisis
Hypertensive crisis can occur when clients taking monoamine oxidase inhibitors (MAOIs) also take medications containing pseudoephedrine or eat foods containing tyramine (aged foods; fermented foods; cured meats; alcoholic beverages such as beer or red wine; or overripe fruits such as raisins, prunes, or bananas). MAOIs inhibit the breakdown of tyramine, causing elevated tyramine levels in the body that can lead to hypertensive crisis. Hypertensive crisis is a medical emergency defined as severe hypertension (blood pressure over 180/120 mm Hg) with acute end-organ damage such as stroke, myocardial infarction, or acute kidney damage. Symptoms may include a severe headache accompanied with confusion and blurred vision. Tachycardia or bradycardia may be present and associated with constricting chest pain. Other symptoms include neck stiffness or soreness, nausea or vomiting, sweating, dilated pupils, photophobia, shortness of breath, severe anxiety, and unresponsiveness. Seizures may occur, as well as intracranial bleeding in association with the increased blood pressure. Hypertensive crisis treatment involves discontinuation of the offending agent, administration of appropriate intravenous antihypertensive medications such as phentolamine or labetalol, and supportive care. In severe cases, treatment in the intensive care unit may be required.[11],[12]
Client Education
Clients should be instructed it may take four to six weeks for antidepressants to achieve their full effectiveness. They should not suddenly stop taking antidepressants or they may experience withdrawal symptoms. When it is time to stop the medication, the provider will slowly and safely decrease the dose. If clients stop taking the medication before the provider advises, the depression may return. They may not feel better with the first antidepressant they try, and they may need to try several different classes of medications to find one that works best for them. Education related to potential side effects and when to contact the provider, clinical worsening, avoiding alcohol, interference with cognitive or motor functioning, and potential drug interactions should also be provided.
Nurses also teach clients about coping strategies to reduce symptoms of depression. For example, regular exercise helps create positive feelings and improves mood. Getting enough quality sleep on a regular basis, eating a healthy diet, and avoiding alcohol (a depressant) can also reduce symptoms of depression.[13] Read more about coping strategies in the “Stress, Coping, and Crisis Intervention” chapter.
Psychotherapy
Psychotherapy may be used alone for treatment of mild depression or in combination with antidepressant medications for moderate to severe depression. Psychotherapy may involve only the individual, but it can include others such as family members or couples therapy to help address issues within these close relationships. Depending on the severity of the depression, significant improvement can be made in 10 to 15 sessions. Group therapy brings people with similar disorders together in a supportive environment to learn how others cope in similar situations.[14]
Cognitive Behavioral Therapy
Cognitive behavioral therapy (CBT) is a form of psychotherapy that is effective for a range of problems including depression, anxiety disorders, alcohol and drug use problems, marital conflict, eating disorders, and severe mental illness. CBT helps a person to recognize distorted/negative thinking with the goal of changing thoughts and behaviors to respond to changes in a more positive manner.[15] Numerous research studies suggest that CBT leads to significant improvement in functioning and quality of life. Studies show that CBT has been demonstrated to be as effective as, or more effective than, other forms of psychological therapy or psychiatric medications.[16]
CBT is based on these core principles[17]:
- Psychological problems are based, in part, on faulty or unhelpful ways of thinking.
- Psychological problems are based, in part, on learned patterns of unhelpful behavior.
- People suffering from psychological problems can learn better ways of coping with them, thereby relieving their symptoms and increasing quality of life.
CBT treatment involves efforts to change thinking patterns. These strategies might include the following[18]:
- Learning to recognize one’s distortions in thinking that are creating problems and then reevaluating them in light of reality.
- Gaining a better understanding of the behavior and motivation of others.
- Using problem-solving skills to cope with difficult situations.
- Learning to develop a greater sense of confidence in one’s own abilities.
CBT treatment also usually involves efforts to change behavioral patterns. These strategies might include facing one’s fears instead of avoiding them, using role-playing to prepare for potentially problematic interactions with others, and learning to calm one’s mind and relax one’s body.[19]
CBT aims to help clients develop skills to manage their feelings in healthy ways. Through in-session exercises and “homework” between sessions, clients develop coping skills, whereby they learn ways to change their own thinking and behavior, ultimately changing how they feel. CBT therapists focus on current situations, thought patterns, and behaviors rather than past events. A certain amount of information about one’s history is needed, but the focus is primarily on developing more effective ways of coping with life moving forward.[20]
Dialectical Behavior Therapy
Dialectical behavior therapy (DBT) is a type of cognitive behavioral therapy that provides clients with new skills to manage painful emotions and decrease conflict in relationships. It has been used successfully to treat people experiencing depression, bulimia, binge-eating, bipolar disorder, post-traumatic stress disorder, borderline personality disorder, and substance abuse. DBT focuses on providing therapeutic skills in four key areas[21]:
- Mindfulness focuses on improving an individual’s ability to accept and be present in the current moment.
- Distress tolerance is geared toward increasing a person’s tolerance of negative emotion, rather than trying to escape from it.
- Emotion regulation strategies are used to manage and change intense emotions that are causing problems in a person’s life.
- Interpersonal effectiveness techniques allow a person to communicate with others in a way that is assertive, maintains self-respect, and strengthens relationships.
Electroconvulsive Therapy
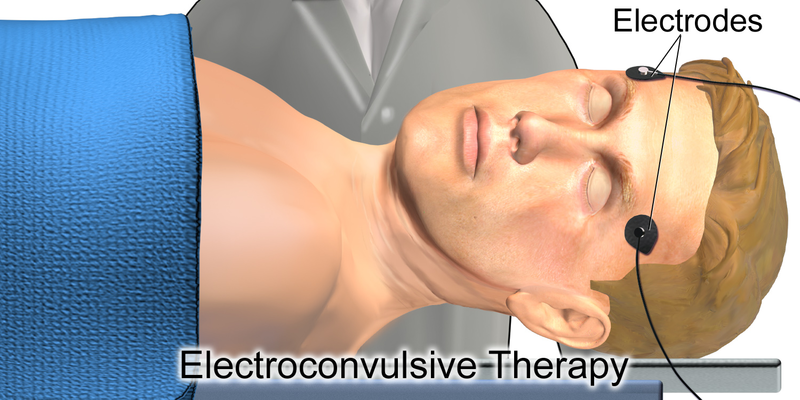
Electroconvulsive therapy (ECT) is a medical treatment reserved for clients with severe major depression who have not responded to medications, psychotherapy, or other treatments. It involves a brief electrical stimulation of the brain while the client is under anesthesia. A client typically receives ECT two to three times a week for a total of 6 to 12 treatments. It is usually managed by a team of trained medical professionals, including a psychiatrist, an anesthesiologist, and a nurse.[22] See Figure 7.8[23] for an image showing ECT electrode placement.
Nursing considerations regarding ECT include the following:
- Pre-procedure education
- Securement of informed consent
- Pre-procedure preparation
- Screening tools used pre- and post-ECT to evaluate side effects, including memory loss
- Medication administration
- Post-ECT care, such as monitoring vital signs and for changes in airway, breathing, and circulation, and implementing fall risk precautions post-anesthesia
A client must provide written informed consent before ECT is administered. In situations where a client is too ill to make decisions for themselves, the consent process is governed by state law (for example, a court-appointed guardian).[24]
Clients and their families should discuss all options for treatment with the psychiatrist before making a specific treatment decision. They should be provided with sufficient information to fully understand the procedure and the potential benefits, risks, and side effects of each treatment option before providing written consent.[25]
General anesthesia is provided during ECT, so presurgical preparation is provided with typical dietary restrictions before the procedure. Typically, this means no food or water after midnight and only a sip of water with morning medications. An intravenous line is inserted, and electrode pads are placed on the head.
A client typically receives ECT two or three times a week for a total of 6 to 12 treatments, depending on the severity of symptoms and the response to treatment. At the time of each treatment, a client is given general anesthesia and a muscle relaxant, and electrodes are attached to the scalp at precise locations. The client’s brain is stimulated with a brief controlled series of electrical pulses. This causes a seizure within the brain that lasts for approximately one minute. The patient is asleep for the procedure and awakens after 5-10 minutes, much as from minor surgery.[26]
ECT treatment has been associated with some risks such as short-term memory loss and difficulty learning. Some people have trouble remembering events that occurred in the weeks before the treatment or earlier. In most cases, memory problems improve within a couple of months. Some clients may experience longer-lasting problems, including permanent gaps in memory.[27]
View the following YouTube video of ECT therapy.[28]
Transcranial Magnetic Stimulation
Transcranial magnetic stimulation (TMS) is a noninvasive procedure that uses magnetic fields to stimulate nerve cells in the brain to improve symptoms of depression. TMS is typically used when other depression treatments haven’t been effective. It uses a magnet to activate the brain. Unlike electroconvulsive therapy (ECT), in which electrical stimulation is more generalized, TMS can be targeted to a specific site in the brain. A typical TMS session lasts 30 to 60 minutes and does not require anesthesia. During the procedure, an electromagnetic coil is held against the forehead near an area of the brain that is thought to be involved in mood regulation. Short electromagnetic pulses are administered through the coil. The magnetic pulses easily pass through the skull and cause small electrical currents that stimulate nerve cells in the targeted brain region. The magnetic field is about the same strength as that of a magnetic resonance imaging (MRI) scan. The person generally feels a slight knocking or tapping on the head as the pulses are administered. The muscles of the scalp, jaw, or face may contract or tingle during the procedure, and mild headaches or brief light-headedness may result after the procedure. It is also possible that the procedure could cause a seizure, although this adverse effect is uncommon. Because the treatment is relatively new, long-term side effects are unknown.[29]
- American Psychiatric Association. (2020). What is depression? https://www.psychiatry.org/patients-families/depression/what-is-depression ↵
- Rush, J. A. (2025). Side effects of antidepressant medication. UpToDate. https://www.uptodate.com/ ↵
- American Psychiatric Association. (2020). What is depression? https://www.psychiatry.org/patients-families/depression/what-is-depression ↵
- National Institute of Mental Health. (2016). Mental health medications. U.S. Department of Health & Human Services. https://www.nimh.nih.gov/health/topics/mental-health-medications ↵
- A.D.A.M. Medical Encyclopedia [Internet]. (2021). Serotonin syndrome. https://medlineplus.gov/ency/article/007272.htm ↵
- Boyer, E. W. (2021). Serotonin syndrome (serotonin toxicity). UpToDate. https://www.uptodate.com/ ↵
- Tanen, D. (2021). Serotonin syndrome. Merck Manual Professional Version. https://www.merckmanuals.com/professional/injuries-poisoning/heat-illness/serotonin-syndrome ↵
- Boyer, E. W. (2021). Serotonin syndrome (serotonin toxicity). UpToDate. https://www.uptodate.com/ ↵
- Tanen, D. (2021). Serotonin syndrome. Merck Manual Professional Version. https://www.merckmanuals.com/professional/injuries-poisoning/heat-illness/serotonin-syndrome ↵
- Spadaro, A., Scott, K. R., Koyfman, A., & Long, B. (2022). High risk and low prevalence diseases: Serotonin syndrome. The American Journal of Emergency Medicine, 61, 90-97. doi: 10.1016/j.ajem.2022.08.030. ↵
- U.S. National Library of Medicine. (2024). Hypertensive crisis. MedlinePlus. https://medlineplus.gov/ ↵
- Sheps, S. G. (2021). Hypertensive crisis: What are the symptoms? Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/high-blood-pressure/expert-answers/hypertensive-crisis/faq-20058491#:~:text=A%20hypertensive%20crisis%20is%20a,higher%20%E2%80%94%20can%20damage%20blood%20vessels. ↵
- American Psychiatric Association. (2020). What is depression? https://www.psychiatry.org/patients-families/depression/what-is-depression ↵
- American Psychiatric Association. (2020). What is depression? https://www.psychiatry.org/patients-families/depression/what-is-depression ↵
- American Psychiatric Association. (2020). What is depression? https://www.psychiatry.org/patients-families/depression/what-is-depression ↵
- Clinical Practice Guideline for the Treatment of Posttraumatic Stress Disorder. (2017). What is cognitive behavioral treatment? American Psychological Association. https://www.apa.org/ptsd-guideline/patients-and-families/cognitive-behavioral ↵
- Clinical Practice Guideline for the Treatment of Posttraumatic Stress Disorder. (2017). What is cognitive behavioral treatment? American Psychological Association. https://www.apa.org/ptsd-guideline/patients-and-families/cognitive-behavioral ↵
- Clinical Practice Guideline for the Treatment of Posttraumatic Stress Disorder. (2017). What is cognitive behavioral treatment? American Psychological Association. https://www.apa.org/ptsd-guideline/patients-and-families/cognitive-behavioral ↵
- Clinical Practice Guideline for the Treatment of Posttraumatic Stress Disorder. (2017). What is cognitive behavioral treatment? American Psychological Association. https://www.apa.org/ptsd-guideline/patients-and-families/cognitive-behavioral ↵
- Clinical Practice Guideline for the Treatment of Posttraumatic Stress Disorder. (2017). What is cognitive behavioral treatment? American Psychological Association. https://www.apa.org/ptsd-guideline/patients-and-families/cognitive-behavioral ↵
- Psychology Today. (n.d.). Dialectical behavior therapy. https://www.psychologytoday.com/us/therapy-types/dialectical-behavior-therapy ↵
- American Psychiatric Association. (2020). What is depression? https://www.psychiatry.org/patients-families/depression/what-is-depression ↵
- “Electroconvulsive_Therapy.png” by BruceBlaus is licensed under CC BY-SA 4.0 ↵
- American Psychiatric Association. (2019). What is electroconvulsive therapy (ECT)? https://www.psychiatry.org/patients-families/ect ↵
- American Psychiatric Association. (2019). What is electroconvulsive therapy (ECT)? https://www.psychiatry.org/patients-families/ect ↵
- American Psychiatric Association. (2019). What is electroconvulsive therapy (ECT)? https://www.psychiatry.org/patients-families/ect ↵
- American Psychiatric Association. (2019). What is electroconvulsive therapy (ECT)? https://www.psychiatry.org/patients-families/ect ↵
- Michigan Medicine. (2022). ECT: Disrupting the stigma around an essential treatment option [Video]. YouTube. https://youtu.be/qk_FjhitKDI?si=hwi32ffhJGvOGM-a ↵
- National Institute of Mental Health. (2016). Brain stimulation therapies. U.S. Department of Health and Human Services. https://www.nimh.nih.gov/health/topics/brain-stimulation-therapies/brain-stimulation-therapies ↵
A significant warning from the Food and Drug Administration (FDA) that alerts the public and health care providers to serious side effects, such as injury or death.
A medical emergency that can occur in clients taking medications that affect serotonin levels.
Severe muscle breakdown which releases myoglobin into the bloodstream and subsequently clogging renal tubules and causing kidney damage.
Acute rise and significantly elevated blood pressure, typically over 180/120 mm Hg, that causes acute end-organ damage such as stroke, myocardial infarction, or acute kidney damage.
A type of psychotherapy that brings people with similar disorders together in a supportive environment to learn how others cope in similar situations.
A type of psychotherapy that helps a person recognize distorted/negative thinking with the goal of changing thought and behaviors to respond to changes in a more positive manner.
A type of cognitive behavioral therapy that provides clients with new skills to manage painful emotions and decrease conflict in relationships.
A medical treatment reserved for patients with severe major depression who have not responded to medications, psychotherapy, or other treatments. It involves a brief electrical stimulation of the brain while the patient is under anesthesia.
A noninvasive procedure that uses magnetic fields to stimulate nerve cells in the brain to improve symptoms of depression.

