3.2 Stress
Everyone experiences stress during their lives. High levels of stress can cause symptoms like headaches, back pain, and gastrointestinal symptoms. Chronic stress contributes to the development of chronic illnesses, as well as acute physical illnesses due to decreased effectiveness of the immune system. It is important for nurses to recognize signs and symptoms of stress in themselves and others, as well as encourage effective stress management strategies. We will begin this section by reviewing the stress response and signs and symptoms of stress and then discuss stress management techniques.
Stress Response
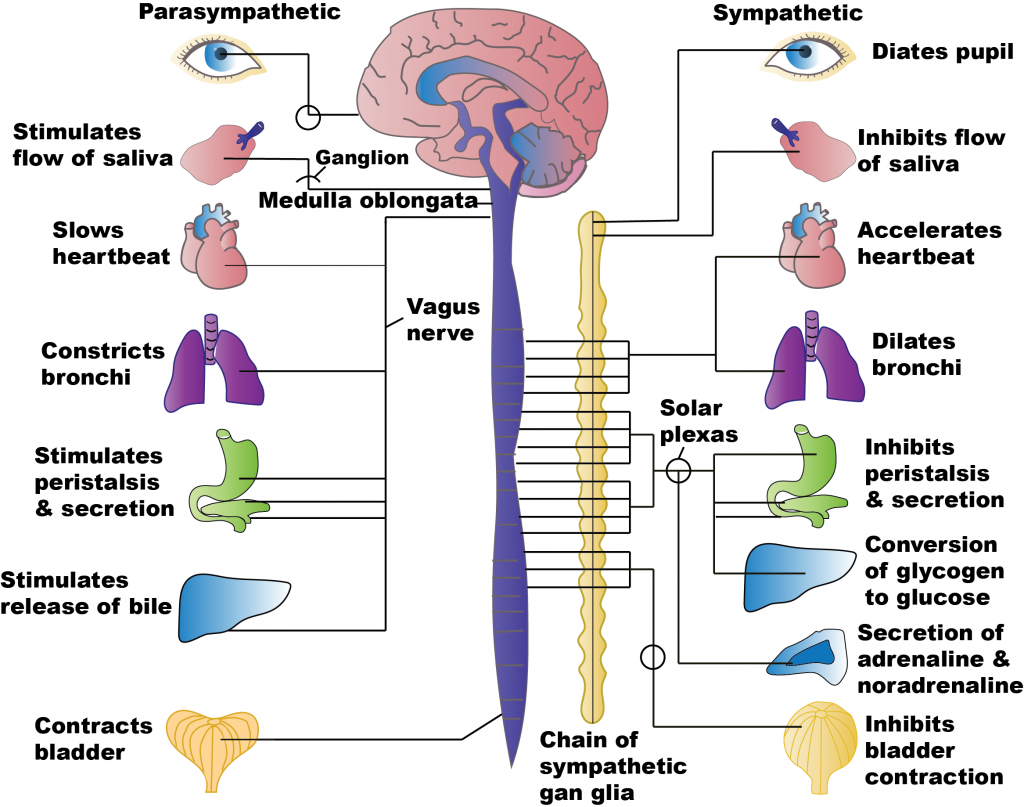
Stressors are any internal or external event, force, or condition that results in physical or emotional stress.[1] The body’s sympathetic nervous system (SNS) responds to actual or perceived stressors with the “fight, flight, or freeze” stress response. Several reactions occur during the stress response that help the individual to achieve the purpose of either fighting or running. The respiratory, cardiovascular, and musculoskeletal systems are activated to breathe rapidly, stimulate the heart to pump more blood, dilate the blood vessels, and increase blood pressure to deliver more oxygenated blood to the muscles. The liver creates more glucose for energy for the muscles to use to fight or run. Pupils dilate to see the threat (or the escape route) more clearly. Sweating prevents the body from overheating from excess muscle contraction. Because the digestive system is not needed during this time of threat, the body shunts oxygen-rich blood to the skeletal muscles. To coordinate all these targeted responses, hormones, including epinephrine, norepinephrine, and glucocorticoids (including cortisol, often referred to as the “stress hormone”), are released by the endocrine system via the hypothalamic-pituitary-adrenal axis (HPA) and dispersed to the many SNS neuroreceptors on target organs simultaneously.[2] After the response to the stressful stimuli has resolved, the body returns to the pre-emergency state facilitated by the parasympathetic nervous system (PNS) that has opposing effects to the SNS. See Figure 3.1[3] for an image comparing the effects of stimulating the SNS and PNS.
Effects of Chronic Stress
The “fight or flight or freeze” stress response equips our bodies to quickly respond to life-threatening stressors. However, exposure to long-term stress can cause serious effects on the cardiovascular, musculoskeletal, endocrine, gastrointestinal, and reproductive systems.[4] Consistent and ongoing increases in heart rate and blood pressure and elevated levels of stress hormones contribute to inflammation in arteries and can increase the risk for hypertension, heart attack, or stroke.[5]
During sudden onset stress, muscles contract and then relax when the stress passes. However, during chronic stress, muscles in the body are often in a constant state of vigilance that may trigger other reactions of the body and even promote stress-related disorders. For example, tension-type headaches and migraine headaches are associated with chronic muscle tension in the area of the shoulders, neck, and head. Musculoskeletal pain in the lower back and upper extremities has also been linked to job stress.[6]
Relaxation techniques and other stress-relieving activities have been shown to effectively reduce muscle tension, decrease the incidence of stress-related disorders, and increase a sense of well-being. For individuals with chronic pain conditions, stress-relieving activities have been shown to improve mood and daily function.[7]
During an acute stressful event, an increase in cortisol can provide the energy required to deal with prolonged or extreme challenges. However, chronic stress can result in an impaired immune system that has been linked to the development of numerous physical and mental health conditions, including chronic fatigue, metabolic disorders (e.g., diabetes, obesity), depression, and immune disorders.[8]
When chronically stressed, individuals may eat much more or much less than usual. Increased food, alcohol, or tobacco can result in acid reflux. Stress can induce muscle spasms in the bowel and can affect how quickly food moves through the gastrointestinal system, causing either diarrhea or constipation. Stress especially affects people with chronic bowel disorders, such as inflammatory bowel disease or irritable bowel syndrome. This may be due to the nerves in the gut being more sensitive, changes in gut microbiota, changes in how quickly food moves through the gut, and/or changes in gut immune responses.[9]
Excess amounts of cortisol can affect the normal biochemical functioning of the male reproductive system. Chronic stress can affect testosterone production, resulting in a decline in sex drive or libido, erectile dysfunction, or impotence. It can negatively impact sperm production and maturation, causing difficulties in couples who are trying to conceive. Researchers have found that men who experienced two or more stressful life events in the past year had a lower percentage of sperm motility and a lower percentage of sperm of normal morphology (size and shape) compared with men who did not experience any stressful life events.[10]
In the female reproductive system, stress affects menstruation and may be associated with absent or irregular menstrual cycles, more painful periods, and changes in the length of cycles. It may make premenstrual symptoms worse or more difficult to cope with, such as cramping, fluid retention, bloating, negative mood, and mood swings. Chronic stress may also reduce sexual desire. Stress can negatively impact a woman’s ability to conceive, the health of her pregnancy, and her postpartum adjustment. Maternal stress can negatively impact fetal development, disrupt bonding with the baby following delivery, and increase the risk of postpartum depression.[11]
Adverse Childhood Experiences
Adults with adverse childhood experiences or exposure to adverse life events often experience ongoing chronic stress with an array of physical, mental, and social health problems throughout adulthood. Some of the most common health risks include physical and mental illness, substance use disorder, and a high level of engagement in risky sexual behavior.[12]
As previously discussed in Chapter 1, adverse childhood experiences (ACEs) include sexual abuse, physical abuse, emotional abuse, physical neglect, emotional neglect, parental loss, or parental separation before the child is 18 years old. Individuals who have experienced four or more ACEs are at a significantly higher risk of developing mental, physical, and social problems in adulthood. Research has established that early life stress is a predictor of smoking, alcohol consumption, and drug dependence. Adults who experienced ACEs related to maladaptive family functioning (parental mental illness, substance use disorder, criminality, family violence, physical and sexual abuse, and neglect) are at higher risk for developing mood, substance abuse, and anxiety disorders. ACEs are also associated with an increased risk of the development of malignancy, cardiovascular disease, metabolic syndrome, and other chronic debilitating conditions.[13]
Signs and Symptoms of Stress
Nurses are often the first to notice signs and symptoms of stress and can help make their clients aware of these symptoms. Common signs and symptoms of chronic stress are as follows[14],[15]:
- Irritability
- Fatigue
- Headaches
- Difficulty concentrating
- Rapid, disorganized thoughts
- Difficulty sleeping
- Digestive problems
- Changes in appetite
- Feeling helpless
- A perceived loss of control
- Low self-esteem
- Loss of sexual desire
- Nervousness
- Frequent infections or illnesses
- Vocalized suicidal thoughts
Stress Management
Recognizing signs and symptoms of stress allows individuals to implement stress management strategies. Nurses can educate clients about effective strategies for reducing the stress response. Effective strategies include the following[16],[17]:
- Set personal and professional boundaries
- Maintain a healthy social support network
- Select healthy food choices
- Engage in regular physical exercise
- Get an adequate amount of sleep each night
- Set realistic and fair expectations
Setting limits is essential for effectively managing stress. Individuals should list all of the projects and commitments making them feel overwhelmed, identify essential tasks, and cut back on nonessential tasks. For work-related projects, responsibilities can be discussed with supervisors to obtain input on priorities. Encourage individuals to refrain from accepting any more commitments until they feel their stress is under control.[18]
Maintaining a healthy social support network with friends and family can provide emotional support.[19] Caring relationships and healthy social connections are essential for achieving resilience.
Physical activity increases the body’s production of endorphins that boost the mood and reduce stress. Nurses can educate clients that a brisk walk or other aerobic activity can increase energy and concentration levels and lessen feelings of anxiety.[20]
People who are chronically stressed often suffer from lack of adequate sleep and, in some cases, stress-induced insomnia. Nurses can educate individuals how to take steps to increase the quality of sleep. Experts recommend going to bed at a regular time each night, striving for at least 7-8 hours of sleep, and, if possible, eliminating distractions, such as television, cell phones, and computers from the bedroom. Begin winding down an hour or two before bedtime and engage in calming activities such as listening to relaxing music, reading an enjoyable book, taking a soothing bath, or practicing relaxation techniques like meditation. Avoid eating a heavy meal or engaging in intense exercise immediately before bedtime. If a person tends to lie in bed worrying, encourage them to write down their concerns and work on quieting their thoughts.[21]
Nurses can encourage clients to set realistic expectations, look at situations more positively, see problems as opportunities, and refute negative thoughts to stay positive and minimize stress. Setting realistic expectations and positively reframing the way one looks at stressful situations can make life seem more manageable. Clients should be encouraged to keep challenges in perspective and do what they can reasonably do to move forward.[22]
Mindfulness is a form of meditation that uses breathing and thought techniques to create an awareness of one’s body and surroundings. Research suggests that mindfulness can have a positive impact on stress, anxiety, and depression.[23] Additionally, guided imagery may be helpful for enhancing relaxation. The use of guided imagery provides a narration that the mind can focus in on during the activity. For example, as the nurse encourages a client to use mindfulness and relaxation breathing, they may say, “As you breathe in, imagine waves rolling gently in. As you breathe out, imagine the waves rolling gently back out to sea.”
WHO Stress Management Guide
In addition to the stress management techniques discussed in the previous section, the World Health Organization (WHO) shares additional techniques in a guide titled Doing What Matters in Times of Stress. This guide is comprised of five categories. Each category includes techniques and skills that, based on evidence and field testing, can reduce overall stress levels even if only used for a few minutes each day. These categories include 1) Grounding, 2) Unhooking, 3) Acting on our values, 4) Being kind, and 5) Making room.[24]
Nurses can educate clients that powerful thoughts and feelings are a natural part of stress, but problems can occur if we get “hooked” by them. For example, one minute you might be enjoying a meal with family, and the next moment you get “hooked” by angry thoughts and feelings. Stress can make someone feel as if they are being pulled away from the values of the person they want to be, such as being calm, caring, attentive, committed, persistent, and courageous.[25]
There are many kinds of difficult thoughts and feelings that can “hook us,” such as, “This is too hard,” “I give up,” “I am never going to get this,” “They shouldn’t have done that,” or memories about difficult events that have occurred in our lives. When we get “hooked,” our behavior changes. We may do things that make our lives worse, like getting into more disagreements, withdrawing from others, or spending too much time lying in bed. These are called “away moves” because they move us away from our values. Sometimes emotions become so strong they feel like emotional storms. However, we can “unhook” ourselves by focusing and engaging in what we are doing, referred to as “grounding.”[26]
Grounding
“Grounding” is a helpful tool when feeling distracted or having trouble focusing on a task and/or the present moment. The first step of grounding is to notice how you are feeling and what you are thinking. Next, slow down and connect with your body by focusing on your breathing. Exhale completely and wait three seconds, and then inhale as slowly as possible. Slowly stretch your arms and legs and push your feet against the floor. The next step is to focus on the world around you. Notice where you are and what you are doing. Use your five senses. What are five things you can see? What are four things you can hear? What can you smell? Tap your leg or squeeze your thumb and count to ten. Touch your knees or another object within reach. What does it feel like? Grounding helps us engage in life, refocus on the present moment, and realign with our values.[27]
Unhooking
At times we may have unwanted, intrusive, negative thoughts that negatively affect us. “Unhooking” is a tool to manage and decrease the impact of these unwanted thoughts. First, NOTICE that a thought or feeling has hooked you, and then NAME it. Naming it begins by silently saying, “Here is a thought,” or “Here is a feeling.” By adding “I notice,” it unhooks us even more. For example, “I notice there is a knot in my stomach.” The next step is to REFOCUS on what you are doing, fully engage in that activity, and pay full attention to whoever is with you and whatever you are doing. For example, if you are having dinner with family and notice feelings of anger, note “I am having feelings of anger,” but choose to refocus and engage with family.[28]
Acting on Our Values
The third category of skills is called “Acting on Our Values.” This means, despite challenges and struggles we are experiencing, we will act in line with what is important to us and our beliefs. Even when facing difficult situations, we can still make the conscious choice to act in line with our values. The more we focus on our own actions, the more we can influence our immediate world and the people and situations we encounter every day. We must continually ask ourselves, “Are my actions moving me toward or away from my values?” Remember that even the smallest actions have impact, just as a giant tree grows from a small seed. Even in the most stressful of times, we can take small actions to live by our values and maintain or create a more satisfying and fulfilling life. These values should also include self-compassion and care. By caring for oneself, we ultimately have more energy and motivation to then help others.[29]
Being Kind
“Being Kind” is a fourth tool for reducing stress. Kindness can make a significant difference to our mental health by being kind to others, as well as to ourselves.
Making Room
“Making Room” is a fifth tool for reducing stress. Sometimes trying to push away painful thoughts and feelings does not work very well. In these situations, it is helpful to notice and name the feeling, and then “make room” for it. “Making room” means allowing the painful feeling or thought to come and go like the weather. Nurses can educate clients that as they breathe, they should imagine their breath flowing into and around their pain and making room for it. Instead of fighting with the thought or feeling, they should allow it to move through them, just like the weather moves through the sky. If clients are not fighting with the painful thought or feeling, they will have more time and energy to engage with the world around them and do things that are important to them.[30]
Read Doing What Matters in Times of Stress by the World Health Organization (WHO).
View the following YouTube video on the WHO Stress Management Guide[31]:
Stress Related to the COVID-19 Pandemic and World Events
The COVID-19 pandemic had a major effect on many people’s lives. Many health care professionals faced challenges that were stressful, overwhelming, and caused strong emotions.[32] See Figure 3.2[33] for a message from the World Health Organization regarding stress and health care workers.
Learning to cope with stress in a healthy way can increase feelings of resiliency for health care professionals. Here are ways to help manage stress resulting from world events[34]:
- Take breaks from watching, reading, or listening to news stories and social media. It’s good to be informed but consider limiting news to just a couple times a day and disconnecting from phones, TVs, and computer screens for a while.
- It can be important to do a self check-in before reading any news. “Do I have the emotional energy to handle a difficult headline if I see one?”
- Take care of your body.
- Take deep breaths, stretch, or meditate
- Try to eat healthy, well-balanced meals
- Exercise regularly
- Get plenty of sleep
- Avoid excessive alcohol, tobacco, and substance use
- Continue routine preventive measures (such as vaccinations, cancer screenings, etc.) as recommended by your health care provider
- Make time to unwind. Plan activities you enjoy.
- Purposefully connect with others. It is especially important to stay connected with your friends and family. Helping others cope through phone calls or video chats can help you and your loved ones feel less lonely or isolated. Connect with your community or faith-based organizations.
- Use the techniques described in the WHO stress management guide.[35]
Strategies for Self-Care
By becoming self-aware regarding signs of stress, you can implement self-care strategies to prevent compassion fatigue and burnout. Use the following “A’s” to assist in building resilience, connection, and compassion[36]:
- Attention: Become aware of your physical, psychological, social, and spiritual health. What are you grateful for? What are your areas of improvement? This protects you from drifting through life on autopilot.
- Acknowledgement: Honestly look at all you have witnessed as a health care professional. What insight have you experienced? Acknowledging the pain of loss you have witnessed protects you from invalidating the experiences.
- Affection: Choose to look at yourself with kindness and warmth. Affection and self-compassion prevent you from becoming bitter and “being too hard” on yourself.
- Acceptance: Choose to be at peace and welcome all aspects of yourself. By accepting both your talents and imperfections, you can protect yourself from impatience, victim mentality, and blame.
Many individuals have had to cope with grief and loss during the COVID pandemic. Read more about coping with grief and loss during COVID at the CDC’s Mental Health Grief and Loss webpage.
- American Psychological Association. (n.d.). Stressor. APA Dictionary of Psychology. https://dictionary.apa.org ↵
- This work is a derivative of Anatomy and Physiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- Untitled image by Meredith Pomietlo for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- Shaw, W., Labott-Smith, S., Burg, M. M., Hostinar, C., Alen, N., van Tilburg, M. A. L., Berntson, G. G., Tovian, S. M., & Spirito, M. (2018, November 1). Stress effects on the body. American Psychological Association. https://www.apa.org/topics/stress/body ↵
- Shaw, W., Labott-Smith, S., Burg, M. M., Hostinar, C., Alen, N., van Tilburg, M. A. L., Berntson, G. G., Tovian, S. M., & Spirito, M. (2018, November 1). Stress effects on the body. American Psychological Association. https://www.apa.org/topics/stress/body ↵
- Shaw, W., Labott-Smith, S., Burg, M. M., Hostinar, C., Alen, N., van Tilburg, M. A. L., Berntson, G. G., Tovian, S. M., & Spirito, M. (2018, November 1). Stress effects on the body. American Psychological Association. https://www.apa.org/topics/stress/body ↵
- Shaw, W., Labott-Smith, S., Burg, M. M., Hostinar, C., Alen, N., van Tilburg, M. A. L., Berntson, G. G., Tovian, S. M., & Spirito, M. (2018, November 1). Stress effects on the body. American Psychological Association. https://www.apa.org/topics/stress/body ↵
- Shaw, W., Labott-Smith, S., Burg, M. M., Hostinar, C., Alen, N., van Tilburg, M. A. L., Berntson, G. G., Tovian, S. M., & Spirito, M. (2018, November 1). Stress effects on the body. American Psychological Association. https://www.apa.org/topics/stress/body ↵
- Shaw, W., Labott-Smith, S., Burg, M. M., Hostinar, C., Alen, N., van Tilburg, M. A. L., Berntson, G. G., Tovian, S. M., & Spirito, M. (2018, November 1). Stress effects on the body. American Psychological Association. https://www.apa.org/topics/stress/body ↵
- Shaw, W., Labott-Smith, S., Burg, M. M., Hostinar, C., Alen, N., van Tilburg, M. A. L., Berntson, G. G., Tovian, S. M., & Spirito, M. (2018, November 1). Stress effects on the body. American Psychological Association. https://www.apa.org/topics/stress/body ↵
- Shaw, W., Labott-Smith, S., Burg, M. M., Hostinar, C., Alen, N., van Tilburg, M. A. L., Berntson, G. G., Tovian, S. M., & Spirito, M. (2018, November 1). Stress effects on the body. American Psychological Association. https://www.apa.org/topics/stress/body ↵
- Amnie, A. G. (2018). Emerging themes in coping with lifetime stress and implication for stress management education. SAGE Open Medicine, 6. https://doi.org/10.1177%2F2050312118782545 ↵
- Amnie, A. G. (2018). Emerging themes in coping with lifetime stress and implication for stress management education. SAGE Open Medicine, 6. https://doi.org/10.1177%2F2050312118782545 ↵
- Shaw, W., Labott-Smith, S., Burg, M. M., Hostinar, C., Alen, N., van Tilburg, M. A. L., Berntson, G. G., Tovian, S. M., & Spirito, M. (2018, November 1). Stress effects on the body. American Psychological Association. https://www.apa.org/topics/stress/body ↵
- Kelly, J. F., & Coons, H. L. (2019, October 25). Stress won’t go away? Maybe you are suffering from chronic stress. American Psychological Association. https://www.apa.org/topics/stress/chronic ↵
- Shaw, W., Labott-Smith, S., Burg, M. M., Hostinar, C., Alen, N., van Tilburg, M. A. L., Berntson, G. G., Tovian, S. M., & Spirito, M. (2018, November 1). Stress effects on the body. American Psychological Association. https://www.apa.org/topics/stress/body ↵
- Kelly, J. F., & Coons, H. L. (2019, October 25). Stress won’t go away? Maybe you are suffering from chronic stress. American Psychological Association. https://www.apa.org/topics/stress/chronic ↵
- Kelly, J. F., & Coons, H. L. (2019, October 25). Stress won’t go away? Maybe you are suffering from chronic stress. American Psychological Association. https://www.apa.org/topics/stress/chronic ↵
- Kelly, J. F., & Coons, H. L. (2019, October 25). Stress won’t go away? Maybe you are suffering from chronic stress. American Psychological Association. https://www.apa.org/topics/stress/chronic ↵
- Kelly, J. F., & Coons, H. L. (2019, October 25). Stress won’t go away? Maybe you are suffering from chronic stress. American Psychological Association. https://www.apa.org/topics/stress/chronic ↵
- Kelly, J. F., & Coons, H. L. (2019, October 25). Stress won’t go away? Maybe you are suffering from chronic stress. American Psychological Association. https://www.apa.org/topics/stress/chronic ↵
- Kelly, J. F., & Coons, H. L. (2019, October 25). Stress won’t go away? Maybe you are suffering from chronic stress. American Psychological Association. https://www.apa.org/topics/stress/chronic ↵
- Kandola, A. (2018, October 12). What are the health effects of chronic stress? MedicalNewsToday. https://www.medicalnewstoday.com/articles/323324#treatment ↵
- This work is a derivative of Doing What Matters in Times of Stress: An Illustrated Guide by World Health Organization and is licensed under CC BY-NC-SA 3.0 IGO ↵
- This work is a derivative of Doing What Matters in Times of Stress: An Illustrated Guide by World Health Organization and is licensed under CC BY-NC-SA 3.0 IGO ↵
- This work is a derivative of Doing What Matters in Times of Stress: An Illustrated Guide by World Health Organization and is licensed under CC BY-NC-SA 3.0 IGO ↵
- This work is a derivative of Doing What Matters in Times of Stress: An Illustrated Guide by World Health Organization and is licensed under CC BY-NC-SA 3.0 IGO ↵
- This work is a derivative of Doing What Matters in Times of Stress: An Illustrated Guide by World Health Organization and is licensed under CC BY-NC-SA 3.0 IGO ↵
- This work is a derivative of Doing What Matters in Times of Stress: An Illustrated Guide by World Health Organization and is licensed under CC BY-NC-SA 3.0 IGO ↵
- This work is a derivative of Doing What Matters in Times of Stress: An Illustrated Guide by World Health Organization and is licensed under CC BY-NC-SA 3.0 IGO ↵
- World Health Organization (WHO). (2020, November 4). Doing what matters in times of stress: An illustrated guide [Video]. YouTube. Licensed in the Public Domain. https://youtu.be/E3Cts45FNrk ↵
- Centers for Disease Control and Prevention. (2021, December 2). Healthcare personnel and first responders: How to cope with stress and build resilience during the COVID-19 pandemic. https://www.cdc.gov/coronavirus/2019-ncov/hcp/mental-health-healthcare.html ↵
- “89118597-2933268333403014-548082632068431872-n.jpg” by unknown author for World Health Organization (WHO) is licensed in the Public Domain. Access for free at https://www.who.int/campaigns/connecting-the-world-to-combat-coronavirus/healthyathome/healthyathome---mental-health?gclid=Cj0KCQiA0MD_BRCTARIsADXoopa7YZldaIqCtKlGrxDV8YcUBtpVSD2HaOtT9NsdT8ajyCXbnPot-bsaAvlQEALw_wcB. ↵
- Centers for Disease Control and Prevention. (2021, December 2). Healthcare personnel and first responders: How to cope with stress and build resilience during the COVID-19 pandemic. https://www.cdc.gov/coronavirus/2019-ncov/hcp/mental-health-healthcare.html ↵
- This work is a derivative of Doing What Matters in Times of Stress: An Illustrated Guide by World Health Organization and is licensed under CC BY-NC-SA 3.0 IGO ↵
- This work is a derivative of Nursing Care at the End of Life by Lowey and is licensed under CC BY-NC-SA 4.0 ↵
Any internal or external event, force, or condition that results in physical or emotional stress.
The body’s physiological response to a real or perceived stressor.
Traumatic circumstances experienced during childhood such as abuse, neglect, or growing up in a household with violence, mental illness, substance use, incarceration, or divorce.

