15.4 Abuse and Neglect
Child Neglect and Abuse
All 50 states and the District of Columbia have child abuse and neglect reporting laws that mandate certain professionals and institutions refer suspected maltreatment to a Child Protective Services (CPS) agency. Each state has its own definitions of child abuse and neglect that are based on standards set by federal law. Federal legislation defines child abuse and neglect as, “Any recent act or failure to act on the part of a parent or caretaker which results in death, serious physical or emotional harm, sexual abuse or exploitation, or an act or failure to act, which presents an imminent risk of serious harm.”[1] In 2019 there were 656,000 victims of child abuse and neglect, with a victim rate calculated as 9 victims per 1,000 children across the United States. In addition, 74.9 percent of victims were neglected, 17.5 percent were physically abused, and 9.3 percent were sexually abused. Child fatalities are the most tragic consequence of maltreatment. In 2019 it was estimated that 1,840 children died from abuse and neglect in the United States. The youngest children are the most vulnerable to maltreatment, with 45.4 percent of child fatalities younger than 1 year old. A perpetrator is the person who is responsible for the abuse or neglect of a child. Furthermore, 77.5% of perpetrators are a parent of the victim.[2]
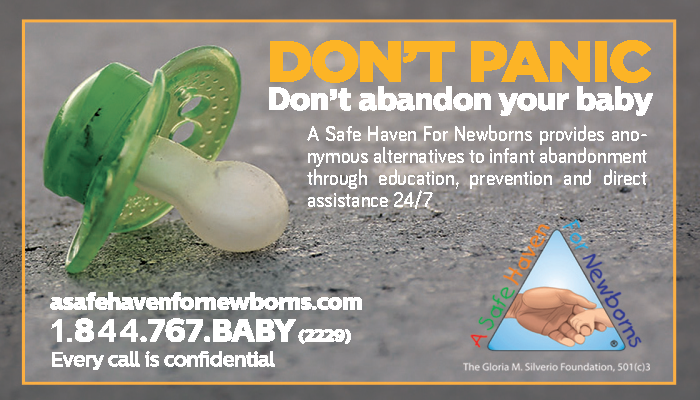
An organization called A Safe Haven for Newborns is dedicated to preventing infant abuse and abandonment through education, prevention, and direct assistance (see Figure 15.4[3]).
Call the Safe Haven Helpline at 1-877-440-2229 or visit the A Safe Haven for Newborns website to find local resources.
Assessment
Signs of Neglect and Abuse
Neglect
Neglect is a situation in which a parent or caretaker fails, refuses, or is unable, for reasons other than poverty, to provide the necessary care, food, clothing, or medical or dental care, which seriously endangers the physical, mental, or emotional health of the child. Signs of child neglect include the following[4]:
- Exhibits poor hygiene or body odor
- Is inappropriately dressed for weather
- Demonstrates needed medical or dental care
- Is left alone unsupervised for long periods of time
- Appears malnourished
- Is constantly hungry or begs for or steals food
- Demonstrates exhibits extreme willingness to please
- Is frequently absent from school
- Arrives early and stays late at school, play areas, or other people’s home
Physical Abuse
Physical abuse is defined as injury inflicted on a child by other than accidental means. Physical injury includes, but is not limited to, lacerations, fractured bones, burns, internal injuries, severe or frequent bruising, or great bodily harm. Signs of physical abuse in children are as follows[5]:
- Bruises and/or welts on face, neck, chest, back, or soft muscle areas less prone to bruising by natural play or accidents (e.g., abdomen, breasts, under arm, inner thigh)
- Injuries in the shape of object (e.g., belt or cord)
- Unexplained burns on palms, soles of feet, or back; a line of demarcation from submerging in hot liquids (e.g., ankles, buttocks, wrists); burns in the shape of object (e.g., fork, cigarette)
- Fractures that do not fit the story of how an injury occurred
- Delay in seeking medical help
- Extremes in behavior (e.g., very aggressive or withdrawn and shy)
- Afraid to go home
- Frightened of parents
- Fearful of other adults
- Failure to thrive
However, some injuries are not visible to observation, such as shaken baby syndrome, a serious brain injury resulting from forcefully shaking an infant or toddler.
Sexual Abuse
Sexual abuse is defined as sexual intercourse or sexual touching of a child; sexual exploitation; human trafficking of a child; forced viewing of sexual activity; or permitting, allowing, or encouraging a child to engage in prostitution. Here are signs of sexual abuse in children[6]:
- Pain, swelling, or itching in genital area
- Bruises, bleeding, discharge in genital area
- Difficulty walking or sitting, frequent urination, or pain
- Stained or bloody underclothing
- Sexually transmitted diseases
- Refusal to take part in gym or other exercises
- Poor peer relationships
- Unusual interest in sex for age
- Drastic change in school achievement
- Runaway or delinquent behavior
- Regressive to behaviors expected for a younger child
Read additional information about human trafficking in the “Vulnerable Populations” chapter.
Emotional Abuse
Emotional abuse is defined as harm to a child’s psychological or intellectual functioning, which is exhibited by severe anxiety, depression, withdrawal, or aggression. Emotional damage may be demonstrated by substantial and observable changes in behavior, emotional response, or learning that are incompatible with the child’s age or stage of development. Signs of emotional abuse in children include the following[7]:
- Low self-esteem
- Self-denigration
- Severe depression
- Unusual level of aggression
- Severe anxiety
- Extreme withdrawal
- Failure to learn
Interventions
Effective interventions are essential to ensure child safety, stop the abuse, support recovery, and prevent future harm. Interventions typically begin with immediate protective actions and extend into medical, psychological, legal, and family-centered care.
When abuse is suspected, professionals such as nurses, educators, and social workers (who are often mandated reporters) must report their concerns to local Child Protective Services (CPS). CPS agencies provide services to children and their families, both in their homes and in foster care. Services are provided to prevent future instances of child maltreatment and remedy conditions that brought the children and their family to the attention of the agency.[8] Once a report is made, CPS investigates the claim, assesses the level of risk, and determines the need for protective measures. In cases of immediate danger, children may be removed from their homes and placed in temporary foster or kinship care. Forensic interviews are often conducted in child advocacy centers by trained professionals using trauma-informed techniques to gather accurate and sensitive information without re-traumatizing the child.
Following the initial response, children may require medical attention to treat injuries or address physical health concerns. Pediatric health care providers, especially those trained in child maltreatment, play a crucial role in identifying signs of abuse and initiating appropriate referrals. Mental health interventions are also essential. Trauma-focused cognitive behavioral therapy (TF-CBT) is widely recognized as an evidence-based treatment that helps children process trauma, develop coping skills, and reduce symptoms of anxiety, depression, or post-traumatic stress.[9] Family therapy may be introduced if reunification with parents or guardians is a possibility, promoting healing and restoring healthy family relationships.
Ongoing support often includes case management and access to family-centered services. Parenting programs and home visiting initiatives, such as the Nurse-Family Partnership, aim to improve caregiver skills, reduce stress, and create safer home environments. These supports are especially beneficial in preventing recurrence of abuse. Social workers and case managers work closely with families to coordinate services, monitor progress, and ensure adherence to safety plans.
Legal involvement is another critical element. Family courts make determinations about custody, visitation, and parental rights, while criminal courts address charges against abusers. Guardians ad litem (GALs) or court-appointed special advocates (CASAs) may be assigned to represent the child’s best interests in these proceedings. The legal process can be daunting for families and children, which is why coordination between legal and mental health professionals is vital to minimize additional trauma.
A multidisciplinary team (MDT) approach enhances the effectiveness of child abuse interventions. This collaborative model brings together health care providers, mental health specialists, law enforcement, educators, and child welfare workers to share information, streamline care, and ensure the child receives comprehensive, holistic support. MDTs often meet at child advocacy centers or through coordinated local systems to address cases in a child-centered and trauma-informed manner.
Importantly, interventions must be tailored to the child’s age, developmental stage, and cultural background. Cultural humility and developmental sensitivity help build trust with families and ensure that services are both respectful and effective. Interventions that are culturally responsive and developmentally appropriate have been shown to reduce disparities in care and promote engagement with services.
Neglect and Abuse of Older Adults and Adults at Risk
Elder abuse is a common problem in the United States. Abuse, including neglect and exploitation, is experienced by about 1 in 10 people aged 60 and older who live at home. From 2002 to 2016, more than 643,000 older adults were treated in the emergency department for nonfatal assaults, and over 19,000 homicides occurred. This information is considered an underestimate of the problem because it is limited to those individuals treated in emergency departments and doesn’t include those who do not seek treatment. Victims must decide whether to tell someone they are being hurt or continue being abused by someone they depend upon or care for deeply.[10]
Elder abuse is defined as an intentional act or failure to act that causes or creates a risk of harm to an older adult. An older adult is defined as someone age 60 or older.[11] Adults at risk are also considered vulnerable adults at risk for abuse. Adults at risk are defined as adults who have a physical or mental condition that impairs their ability to care for their own needs.[12] Older adults and adults at risk are potentially susceptible for abuse, neglect, or financial exploitation by caregivers or a person they trust.[13] A caregiver is a person who has taken responsibility for all or part of an individual’s care. Risk factors for elder abuse include cognitive impairment, functional dependency, poor physical health, low income, social isolation, and a history of past trauma or abuse. Perpetrator-related risk factors include caregiver burden, psychiatric illness, and substance abuse. Environmental factors such as living in high-crime areas and low social support also contribute to the risk.[14]
The following are types of elder abuse[[15]:
- Physical abuse: Physical abuse refers to illness, pain, injury, functional impairment, distress, or death as a result of the intentional use of physical force and includes acts such as hitting, kicking, pushing, slapping, and burning. See Figure 15.5[16] for an infographic describing physical signs of elder abuse.
- Sexual abuse: Sexual abuse refers to forced or unwanted sexual interaction of any kind. This may include unwanted sexual contact or penetration or non-contact acts such as sexual harassment.
- Emotional abuse: Emotional abuse refers to verbal or nonverbal behaviors that inflict anguish, mental pain, fear, or distress, such as humiliation or disrespect, verbal and nonverbal threats, harassment, and geographic or interpersonal isolation.
- Neglect: Neglect is the failure to meet the person’s basic needs, including food, water, shelter, clothing, hygiene, and essential medical care.
- Financial abuse: Financial abuse is the illegal, unauthorized, or improper use of money, benefits, belongings, property, or assets for the benefit of someone other than the individual.
- Treatment without consent: Treatment without consent refers to the administration of medication or the performance of psychosurgery, electroconvulsive therapy, or experimental research on an individual who has not provided informed consent.
- Unreasonable confinement or restraint: Unreasonable confinement or restraint refers to the intentional and unnecessary confinement of an individual in a locked room, involuntary separation from their living area, use of physical restraints, or the provision of unnecessary or excessive medication. (This does not include the use of these methods or devices if they conform with state and federal standards governing restraint or seclusion. Review ANA guidelines on using restraints in the “Client Rights” section of the “Legal and Ethical Considerations in Mental Health Care” chapter.)
Assessment
Elder abuse can be challenging to detect, as symptoms may be subtle or mistaken for age-related conditions. A comprehensive assessment involves careful observation, open-ended questioning, and consideration of both physical and psychosocial indicators. Clinicians should maintain a high index of suspicion, especially when inconsistencies arise between reported histories and observed findings.
Physical indicators may include unexplained injuries such as bruises, lacerations, burns, or fractures. Particular attention should be paid to injury patterns that are inconsistent with normal aging or accidental trauma. For instance, bruising on the maxillofacial area, upper extremities (especially the inner arms), or torso may suggest defensive injuries or restraint use. Recurrent injuries at various stages of healing are also red flags. In cases of sexual abuse, assess for genital trauma, sexually transmitted infections, or sudden behavioral changes.[17],[18]
Behavioral and psychological signs can include withdrawal, increased anxiety, depression, agitation, or fear of specific individuals—especially caregivers. A once-outgoing elder who becomes socially isolated or unusually quiet during interactions may be experiencing emotional or psychological abuse.[19],[20]
Neglect-related signs are equally important and may present as poor hygiene, untreated medical conditions, malnutrition, dehydration, pressure injuries, or inappropriate clothing for the weather. Weight loss without a medical cause or a dirty, unsafe living environment may also be indicative of neglect.[21],[22]
Health care utilization patterns may offer additional clues. Frequent emergency department visits, inconsistent follow-up care, or evidence of “doctor shopping” by caregivers may signal underlying abuse or caregiver manipulation.
During assessment, it’s crucial to do the following:
- Interview the elder alone, if possible, to ensure their safety and candor.
- Use validated screening tools, such as the Elder Abuse Suspicion Index (EASI) or Hwalek-Sengstock Elder Abuse Screening Test (H-S/EAST).[23]
- Document findings thoroughly and objectively, including direct quotes, photos (as per policy), and detailed descriptions of injuries or environmental conditions.
Lastly, consider cultural and cognitive factors that may affect an elder’s willingness or ability to disclose abuse. Older adults with dementia or language barriers may require additional support or modified communication strategies.

Interventions
Effective interventions for elder abuse require a coordinated, multidisciplinary response that prioritizes the safety, dignity, and autonomy of the older adult. Once abuse is suspected or confirmed, a key resource is Adult Protective Services (APS). APS agencies are state-run programs that investigate reports of elder and vulnerable adult abuse, neglect, and exploitation. Their role is to protect adults—particularly those with developmental disabilities, degenerative brain disorders, serious mental illness, or other incapacities—who are unable to protect themselves from harm.
APS interventions are tailored to the individual’s needs and may include outreach; crisis counseling; and coordination of medical, legal, and social services. Caseworkers assess the level of risk and collaborate with health care providers, legal authorities, and family members to ensure safety while respecting the adult’s right to self-determination when possible. Services may also include helping arrange safe housing, facilitating access to mental health or substance use treatment, and supporting guardianship proceedings if the individual is deemed unable to make informed decisions
In cases of financial exploitation, APS may work in tandem with law enforcement and financial institutions to recover assets or pursue prosecution. When abuse involves a caregiver, interventions can also focus on caregiver support, respite care, and education to reduce stress and prevent recurrence. For institutional settings, reporting to long-term care ombudsman programs and state licensing boards may trigger regulatory reviews and corrective actions.[24]
See Figure 15.6[25] for an illustration related to reporting concerns about vulnerable adults.

Find resources in your area for reporting elder abuse at the National Adult Protective Services Association website.
Read more about protective services in your state. Here is the link to Wisconsin’s Adult Protective Services.
Find elder care resources in your community at Eldercare Locator.
Mandatory Reporting
Mandated reporters are required by law to report suspected abuse and neglect they see in the course of their professional duties. Nurses and other professionals are referred to as mandated reporters because they are required by state law to report suspected neglect or abuse of children, adults at risk, and the elderly. Nurses should be aware of the county or state agencies to whom they should report suspected abuse. For example, in Wisconsin, suspected neglect or abuse is reported to the Child Protective Services (CPS) or law enforcement. Persons required to report and who intentionally fail to report suspected child abuse or neglect may be fined up to $1,000 or imprisoned for up to six months or both.[26] See Figure 15.7[27] for an image related to reporting suspected abuse and neglect.

What to Report
Mandatory reporters who suspect neglect or abuse should contact their county social/human services department, sheriff, or local police department immediately. When making a report, explain what happened or is happening to the child, vulnerable adult, or elderly. Describe the nature of the abuse or neglect and be as specific as possible. Be prepared to give the name, date of birth, address, and telephone number of the victim, as well as the name of their parent or caregiver. If you do not know all of this information, report what you do know and explain all you know about the situation and family dynamics.[28]
When a report is filed, the receiving department will make a safety screening determination based on state statutes. If the report meets the criteria for alleged maltreatment, a social worker from the county department of social/human services will proceed with an investigation of the reported maltreatment and work with the parents or caregiver to assess the situation to determine if any support or assistance is needed to protect the child, vulnerable adult, or elderly.[29]
Find resources in your area for reporting suspected child abuse at ChildHelp National Child Abuse Hotline.
Read more about protective services in your state. Access Wisconsin’s information at Child Protective Services.
- Administration for Children & Families. (2021). Child maltreatment 2019. [Report]. U.S. Department of Health & Human Services. https://www.acf.hhs.gov/cb/report/child-maltreatment-2019 ↵
- Administration for Children & Families. (2021). Child maltreatment 2019. [Report]. U.S. Department of Health & Human Services. https://www.acf.hhs.gov/cb/report/child-maltreatment-2019 ↵
- “bc-english-ashfnb” by A Safe Haven for Newborns is used under Fair Use. Access for free at https://asafehavenfornewborns.com/international-safe-haven/ ↵
- Wisconsin Department of Children and Families. (n.d.). Signs of child abuse and neglect. https://dcf.wisconsin.gov/cps/signs ↵
- Wisconsin Department of Children and Families. (n.d.). Signs of child abuse and neglect. https://dcf.wisconsin.gov/cps/signs ↵
- Wisconsin Department of Children and Families. (n.d.). Signs of child abuse and neglect. https://dcf.wisconsin.gov/cps/signs ↵
- Wisconsin Department of Children and Families. (n.d.). Signs of child abuse and neglect. https://dcf.wisconsin.gov/cps/signs ↵
- Administration for Children & Families. (2021). Child maltreatment 2019. [Report]. U.S. Department of Health & Human Services. https://www.acf.hhs.gov/cb/report/child-maltreatment-2019 ↵
- Medical University of South Carolina. (n.d.). TF-CBT Web: Trauma-focused cognitive behavioral therapy training. https://www.tfcbt.org ↵
- Centers for Disease Control and Prevention. (2024). About abuse of older persons. https://www.cdc.gov/elder-abuse/about/index.html ↵
- Centers for Disease Control and Prevention. (2024). About abuse of older persons. https://www.cdc.gov/elder-abuse/about/index.html ↵
- Wisconsin Department of Health Services. (2018). Adult protective services: Definitions. https://www.dhs.wisconsin.gov/aps/definitions.htm#Abuse ↵
- Centers for Disease Control and Prevention. (2024). About abuse of older persons. https://www.cdc.gov/elder-abuse/about/index.html ↵
- Johannesen, M., & LoGiudice, D. (2013). Elder abuse: a systematic review of risk factors in community-dwelling elders. Age Ageing, 42(3), 292-8. doi: 10.1093/ageing/afs195. ↵
- Centers for Disease Control and Prevention. (2024). About abuse of older persons. https://www.cdc.gov/elder-abuse/about/index.html ↵
- “Signs of Elder Abuse - Physical” by National Council on Aging is used under Fair Use. Access for free at https://www.ncoa.org/article/get-the-facts-on-elder-abuse ↵
- National Center on Elder Abuse (NCEA). (2020). Types and signs of abuse. U.S. Department of Health & Human Services. https://ncea.acl.gov ↵
- Lachs, M. S., & Pillemer, K. A. (2015). Elder abuse. The New England Journal of Medicine, 373(20), 1947–1956. https://doi.org/10.1056/NEJMra1404688 ↵
- National Center on Elder Abuse (NCEA). (2020). Types and signs of abuse. U.S. Department of Health & Human Services. https://ncea.acl.gov ↵
- Lachs, M. S., & Pillemer, K. A. (2015). Elder abuse. The New England Journal of Medicine, 373(20), 1947–1956. https://doi.org/10.1056/NEJMra1404688 ↵
- National Center on Elder Abuse (NCEA). (2020). Types and signs of abuse. U.S. Department of Health & Human Services. https://ncea.acl.gov ↵
- Lachs, M. S., & Pillemer, K. A. (2015). Elder abuse. The New England Journal of Medicine, 373(20), 1947–1956. https://doi.org/10.1056/NEJMra1404688 ↵
- Yaffe, M. J., Wolfson, C., Lithwick, M., & Weiss, D. (2008). Development and validation of a tool to improve physician identification of elder abuse: The Elder Abuse Suspicion Index (EASI). Journal of Elder Abuse & Neglect, 20(3), 276–300. https://doi.org/10.1080/08946560801973168 ↵
- National Adult Protective Services Association. (n.d.). Adult Protective Services (APS). https://www.napsa-now.org/get-informed/what-is-adult-protective-services/ ↵
- “APS_header_3.jpg” by unknown author for Washington State Department of Social and Health Services is used under Fair Use. ↵
- Wisconsin Department of Children and Families. (2019). It shouldn’t hurt to be a child… but sometimes it does. [PDF Brochure]. https://dcf.wisconsin.gov/files/publications/pdf/0101.pdf ↵
- “stop-child-abuse-see-the-signs-make-the-call-1536x748.jpg” by unknown author for Delaware Department of Services for Children, Youth & Their Families is used under Fair Use. ↵
- Wisconsin Department of Children and Families. (2019). It shouldn’t hurt to be a child… but sometimes it does. [PDF Brochure]. https://dcf.wisconsin.gov/files/publications/pdf/0101.pdf ↵
- Wisconsin Department of Children and Families. (2019). It shouldn’t hurt to be a child… but sometimes it does. [PDF Brochure]. https://dcf.wisconsin.gov/files/publications/pdf/0101.pdf ↵
When a parent or caretaker fails, refuses, or is unable, for reasons other than poverty, to provide the necessary care, food, clothing, or medical or dental care, which seriously endangers the physical health of the child.
Defined as injury inflicted on a child by other than accidental means.
Sexual intercourse or sexual touching of a child; sexual exploitation; sex trafficking of a child; forced viewing of sexual activity; or permitting, allowing, or encouraging a child to engage in prostitution.
Harm to a child’s psychological or intellectual functioning, which is exhibited by severe anxiety, depression, withdrawal, or aggression.
An evidence-based treatment that helps children process trauma, develop coping skills, and reduce symptoms of anxiety, depression, or post-traumatic stress.
An intentional act or failure to act that causes or creates a risk of harm to an older adult.
Adults who have a physical or mental condition that impairs their ability to care for their own needs.
A person who has taken responsibility for all or part of an individual's care.
State-run programs that investigate reports of elder and vulnerable adult abuse, neglect, and exploitation.
Individuals required by state law to report suspected neglect or abuse of children, adults at risk, and the elderly.

