11.3 Schizophrenia
There is a spectrum of psychotic disorders, and schizophrenia is one of the disorders on the spectrum. Schizophrenia is a serious mental illness that affects how a person thinks, feels, and behaves. It also affects the person’s ability to recognize their symptoms as problematic, referred to as a “lack of insight.” Continuous signs of the disturbance must be present for at least six months in order for schizophrenia to be diagnosed, and potential medical conditions that could be causing delirium must be ruled out.[1],[2]
Schizophrenia is typically diagnosed in the late teen years to the early thirties and tends to emerge earlier in males than females. A diagnosis of schizophrenia often follows the first episode of psychosis when individuals first display symptoms of schizophrenia. Gradual changes in thinking, mood, and social functioning often begin before the first episode of psychosis, usually starting in mid-adolescence. (See “Early Signs of Psychosis” in the previous section.) Schizophrenia can occur in younger children, but it is rare for it to occur before late adolescence.[3]
Symptoms of Schizophrenia
Symptoms of schizophrenia are classified by three categories: positive, negative, and cognitive:[4]
- Positive symptoms: Positive symptoms reflect behaviors or experiences that are added to a person’s mental functioning. They represent a distortion or excess of normal functions. Positive symptoms include hallucinations, delusions, thought disorders, disorganized speech, and alterations in behaviors. Read more about delusions and hallucinations in the “Thoughts and Perceptions” subsection of the “Assessment” section of the “Application of the Nursing Process in Mental Health Care” chapter. The most common types of delusions experienced by individuals with schizophrenia are paranoia, persecutory, grandiose, or religious ideas. For example, an individual with persecutory delusions may feel the nursing staff is trying to poison them when they administer medications. People with psychotic symptoms lose a shared sense of reality and experience the world in a distorted way.
- Negative symptoms: Negative symptoms refer to the absence or decrease of normal behaviors and emotional responses. They include a loss of motivation, disinterest or lack of enjoyment in daily activities, social withdrawal, difficulty showing emotions, and difficulty functioning normally. Individuals typically experience the following negative symptoms:
- Reduced motivation and difficulty planning, beginning, and sustaining activities (i.e., avolition)
- Diminished feelings of pleasure in everyday life (i.e., anhedonia)
- Flat affect (i.e., reduced expression of emotions via facial expression or voice tone)
- Reduced speaking
- Cognitive symptoms: Cognitive symptoms refer to problems in attention, concentration, and memory. For some individuals, the cognitive symptoms of schizophrenia are subtle, but for others, they are more prominent and interfere with activities like following conversations, learning new things, or remembering appointments. Individuals typically experience symptoms such as these:
- Difficulty processing information to make decisions
- Problems using information immediately after learning it
- Trouble focusing or paying attention
The Positive and Negative Syndrome Scale (PANSS) is a widely used tool for measuring the severity of symptoms in clients with schizophrenia. It consists of 30 items, each rated on a scale from 1 (absent) to 7 (extreme), with higher scores indicating more severe symptoms. The scale is divided into three subscales: positive symptoms (7 items), negative symptoms (7 items), and general psychopathology (16 items).
See the following box for signs and symptoms for the diagnosis of schizophrenia according to the DSM-5-TR.
Symptoms of Schizophrenia[5]
Schizophrenia is diagnosed when two (or more) of the following characteristics are present for a significant portion of time during a one-month period (or less if successfully treated). At least one symptom is delusions, hallucinations, or disorganized speech:
- Delusions
- Hallucinations
- Disorganized speech (i.e., frequent derailment or incoherence)
- Grossly disorganized or catatonic behavior. (Catatonia is a state of unresponsiveness.)
- Negative symptoms (i.e., diminished emotional expression or avolition.)
Additionally, for a significant portion of time, the client’s level of functioning in one or more areas, such as work, interpersonal relations, or self-care, is significantly below their prior level of functioning. Continuous signs of schizophrenia persist for at least six months (or less if it is successfully treated). Depressive or bipolar disorders with psychotic features must have been previously ruled out, and the disturbance is not attributable to the physiological effects of a substance or other medical condition. The provider may specify if this is the first episode or multiple episodes and if it is an acute episode, in partial remission, or in full remission.[6]
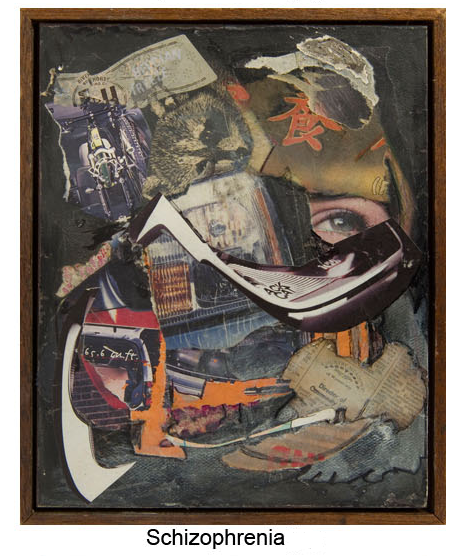
See Figure 11.2[7] for an artwork depiction of the thought disorders associated with schizophrenia.
Risk Factors for Schizophrenia
It is believed that several factors contribute to the risk of developing schizophrenia, including genetics, environment, and brain structure and function.[8]
Genetics
Schizophrenia tends to run in families. Genetic studies strongly suggest that many different genes increase the risk of developing schizophrenia, but that no single gene causes the disorder by itself. It is not yet possible to use genetic information to predict who will develop schizophrenia.[9]
Environment
Scientists think that interactions between genetic risk and aspects of an individual’s environment play a role in the development of schizophrenia. Environmental factors that may be involved include adverse childhood experiences (ACE) or exposure to viruses or nutritional problems before birth.[10] Other environmental risk factors include urban upbringing, migration, and early life adversities.[11] A systematic review found that cannabis (marijuana) worsens symptoms of psychosis in genetically predisposed individuals and causes more relapses and hospitalizations.[12]
Brain Structure and Function
Scientists think that differences in brain structure, function, and interactions among neurotransmitters may contribute to the development of schizophrenia. For example, differences in the volumes of specific components of the brain; the manner in which regions of the brain are connected and work together; and neurotransmitters, such as dopamine, are found in people with schizophrenia. Differences in brain connections and brain circuits seen in people with schizophrenia may begin developing before birth. Changes to the brain that occur during puberty may trigger psychotic episodes in people who are already vulnerable due to genetics, environmental exposures, or the types of brain differences mentioned previously.[13]
View the following YouTube video on an individual’s experience with psychosis[14]: What is Psychosis?
Treatment
Early treatment of psychosis increases the chance of a successful remission.[15] Treatments focus on managing symptoms and solving problems related to day-to-day functioning and include antipsychotic medications, psychosocial treatments, family education and support, coordinated specialty care, and assertive community treatment.[16]
Antipsychotic Medications
Antipsychotic medications reduce the intensity and frequency of psychotic symptoms by inhibiting dopamine receptors. Certain symptoms of psychosis, such as feeling agitated and having hallucinations, resolve within days of starting an antipsychotic medication. Symptoms like delusions usually resolve within a few weeks, but the full effects of the medication may not be seen for up to six weeks.[17]
First-generation antipsychotics (also called “typical antipsychotics”) treat positive symptoms of schizophrenia and have several potential adverse effects due to their tight binding to dopamine receptors. Medication is prescribed based on the client’s ability to tolerate the adverse effects. Second-generation antipsychotics (also referred to as “atypical antipsychotics”) treat both positive and negative symptoms of schizophrenia. They have fewer adverse effects because they block selective dopamine D2 receptors, as well as serotonin, so they are generally better tolerated than first-generation antipsychotics. Clients respond differently to antipsychotic medications, so it may take several trials of different medications to find the one that works best for their symptoms.[18]
See Table 11.3 for a list of common antipsychotic medications. They are usually taken daily in pill or liquid form. Some antipsychotic medications can also be administered as injections twice a month, monthly, every three months, or every six months, which can be more convenient and improve medication adherence.
Review information on neuroreceptors affected by antipsychotic medications in the “Antipsychotics” section of the “Psychotropic Medications” chapter.
Table 11.3. Common Antipsychotic Medications[19],[20],[21]
| Medication Class | Mechanism of Action | Adverse Effects |
|---|---|---|
| First-Generation (Typical)
Examples: Chlorpromazine Haloperidol Perphenazine Fluphenazine |
Postsynaptic blockade of dopamine receptors in the brain |
|
| Second-Generation (Atypical)
Examples: Risperidone Olanzapine Quetiapine Ziprasidone Aripiprazole Paliperidone Lurasidone Clozapine |
Postsynaptic blockade of dopamine receptors in the brain |
|
Clozapine
Clients with treatment-resistant schizophrenia may be prescribed clozapine, a specific type of atypical antipsychotic medication. However, people treated with clozapine must undergo routine blood testing to detect a potentially dangerous side effect called agranulocytosis (extremely low white blood cell count). Clozapine also has strong anticholinergic, sedative, cardiac, and hypotensive properties and frequent drug-drug interactions.[22]
Boxed Warning
A Boxed Warning states that elderly clients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death.[23]
Adverse Effects
Common side effects of both first- and second-generation antipsychotics include the following[24]:
- Anticholinergic symptoms: dry mouth, constipation, blurred vision, or urinary retention[25]
- Drowsiness
- Dizziness
- Restlessness
- Weight gain
- Nausea or vomiting
- Low blood pressure
First-generation antipsychotics, also known as neuroleptics or typical antipsychotics, have significant potential to cause extrapyramidal side effects and tardive dyskinesia due to their tight binding to dopamine receptors. The risk for developing these movement disorders is the primary difference between first-generation antipsychotics and second-generation antipsychotics (also known as atypical antipsychotics). In other respects, the two classes of medication have similar side effects and mechanisms of action.[26]
Extrapyramidal (EPS) side effects refer to akathisia (psychomotor restlessness), rigidity, bradykinesia (slowed movement), tremor, and dystonia (involuntary contractions of muscles of the extremities, face, neck, abdomen, pelvis, or larynx in either sustained or intermittent patterns that lead to abnormal movements or postures). See Figure 11.3[27] for an image of dystonia.
Acute dystonic reactions affecting the larynx can be a medical emergency requiring intubation and mechanical ventilation. EPS symptoms usually resolve dramatically within 10 to 30 minutes of administration of parenteral anticholinergics such as diphenhydramine and benztropine.[28]
Tardive dyskinesia (TD) is a syndrome of movement disorders that can occur in clients taking first-generation antipsychotics. Hallmark symptoms are smacking and puckering lips, eye blinking, grimacing, and twitching. TD persists for at least one month and can last up to several years despite discontinuation of the medications. Primary treatment of TD includes discontinuation of first-generation antipsychotics and may include the addition of another medication. Second-generation VMAT2 inhibitors such as deutetrabenazine and valbenazine are considered first-line treatment for TD. Clonazepam and ginkgo biloba have also shown good effectiveness for improving symptoms of TD.[29],[30]

View a supplementary YouTube video on tardive dyskinesia[31]: Understanding Tardive Dyskinesia.
Neuroleptic malignant syndrome (NMS) is a rare but fatal adverse effect that can occur at any time during treatment with antipsychotics. It typically develops over a period of days to weeks and resolves in approximately nine days with treatment. Signs include increased temperature, severe muscular rigidity, confusion, agitation, hyperreflexia, elevation in white blood cell count, elevated creatinine phosphokinase, elevated liver enzymes, myoglobinuria, and acute renal failure. The antipsychotic should be immediately discontinued when signs occur. Dantrolene and bromocriptine are typically prescribed for treatment. Nursing interventions include adequate hydration, cooling, and close monitoring of vital signs and serum electrolytes.[32]
View a supplementary YouTube video[33] on NMS: Neuroleptic Malignant Syndrome in 3 Minutes.
Second-generation antipsychotics have a significantly decreased risk of extrapyramidal side effects but are associated with weight gain and the development of metabolic syndrome.[34] Metabolic syndrome is a cluster of conditions that occur together, increasing the risk of heart disease, stroke, and type 2 diabetes. Symptoms include increased blood pressure; high blood sugar; excess body fat around the waist (also referred to as having an “apple waistline”); and abnormal cholesterol, triglyceride levels, and high-density lipoprotein (HDL) levels. Weight, glucose levels, and lipid levels should be monitored before treatment is initiated then annually.
View a supplementary YouTube video[35] on metabolic syndrome: What is Metabolic Syndrome?
View this PDF comparison: Adverse Effects of Antipsychotic Medications.
Client Education
Clients should be advised to contact their provider if and side effects occur. This includes the development of any involuntary or uncontrollable movements. They should be warned to not suddenly stop taking the medication because abrupt withdrawal can cause dizziness; nausea and vomiting; and uncontrolled movements of the mouth, tongue, or jaw. Clients should be warned to not consume alcohol or other CNS depressants because their ability to operate machinery or drive may be impaired.
Relapse
Some people may experience relapse, meaning their psychosis symptoms come back or get worse. Relapses typically occur when people stop taking their prescribed antipsychotic medication or when they take it sporadically. Some people stop taking prescribed medications because they feel better or they feel that they don’t need it anymore, but medication should never be stopped suddenly. After talking with a prescriber, clients can gradually taper their medications in some situations. However, most people with schizophrenia must stay on an antipsychotic continuously for months, years, or indefinitely for mental wellness.[36]
Psychosocial Treatments
Cognitive behavioral therapy, behavioral skills training, supported employment, and cognitive remediation interventions are types of psychosocial treatments that can help address the negative and cognitive symptoms of schizophrenia. A combination of these therapies and antipsychotic medication is a common treatment approach for schizophrenia. Psychosocial treatments can help improve an individual’s coping skills with the everyday challenges of schizophrenia. Therapies can also help people pursue their life goals, such as attending school, working, or forming relationships. Individuals who participate in regular psychosocial treatments are less likely to relapse or be hospitalized.[37]
Family Education and Support
Psychosis and schizophrenia can take a heavy toll on a client’s family members, significant others, and friends. Educational programs offer instruction about schizophrenia symptoms, treatments, and strategies for assisting their loved one experiencing psychosis and schizophrenia. Increasing their understanding of psychotic symptoms, treatment options, and the course of recovery can lessen their distress, bolster their own coping strategies, and empower them to offer effective assistance to their loved one. Family-based services may be provided on an individual basis or through multi-family workshops and support groups.
For more information about family-based services in your area, visit the family education and support groups page on the National Alliance on Mental Illness website.[38]
Coordinated Specialty Care
Coordinated specialty care (CSC) is a general term used to describe recovery-oriented treatment programs for people with first-episode psychosis, an early stage of schizophrenia. A team of health professionals and specialists deliver CSC that includes psychotherapy, medication management, case management, employment and education support, and family education and support. The person with early psychosis and the team work together in a client-centered and family-centered approach to make treatment decisions. Compared to typical care for early psychosis, CSC is more effective at reducing symptoms, improving quality of life, and increasing involvement in work or school.[39]
The goal is to link the individual with a CSC team as soon as possible after psychotic symptoms begin. There are many different programs that are considered CSC in the United States, including (but are not limited to) Comprehensive Community Support (CCS), Community Support Programs (CSP), NAVIGATE, Connection Program, OnTrackNY, Specialized Treatment Early in Psychosis (STEP) program, and Early Assessment and Support Alliance (EASA). Supported Employment/Education (SEE) is an important part of CSC that helps individuals return to work or school because it addresses the client’s personal goals. A SEE specialist helps clients develop the skills they need to achieve school and work goals. In addition, the specialist can be a bridge between clients and educators or employers.[40]
Research from the RAISE project (Recovery After an Initial Schizophrenia Episode) has shown that treatments for psychosis work better when they are delivered closer to the time when psychotic symptoms first appear. The goal of the RAISE project is to help decrease the likelihood of future episodes of psychosis, reduce long-term disability, and help people to get their lives back on track so they can pursue their goals.[41]
Read more about the RAISE project at RAISE Questions and Answers web page.
With early diagnosis and appropriate treatment, it is possible to recover from psychosis. Many people who receive early treatment never have another psychotic episode. For other people, recovery means the ability to live a fulfilling and productive life, even if psychotic symptoms return at times. However, if untreated, psychotic symptoms can cause disruptions in school and work, strained family relations, and separation from friends. The longer the symptoms go untreated, the greater the risk for developing additional problems. These problems can include abusing substances, having legal trouble, or becoming homeless.[42]
Assertive Community Treatment
Assertive Community Treatment (ACT) is designed for individuals with schizophrenia who are at risk for repeated hospitalizations or homelessness. Research has demonstrated a prevalence of psychosis as high as 21% among homeless people living on the street.[43] See Figure 11.4[44] for an image of a homeless man. ACT is based on a multidisciplinary team approach, including a medication prescriber, a shared caseload among team members, direct service provision by team members, high frequency of client contact, low client to staff ratios, and outreach to clients in the community. ACT has been shown to reduce hospitalizations and homelessness among individuals with schizophrenia.[45]

Read more information about ACT programs on the Substance Abuse and Mental Health Services Administration (SAMHSA) website.
- National Institute of Mental Health. (2024). Schizophrenia. U.S. Department of Health and Human Services. https://www.nimh.nih.gov/health/topics/schizophrenia ↵
- American Psychiatric Association. (2022). Desk reference to the diagnostic criteria from DSM-5-TR (5th ed.). American Psychiatric Association Publishing. ↵
- National Institute of Mental Health. (2024). Schizophrenia. U.S. Department of Health and Human Services. https://www.nimh.nih.gov/health/topics/schizophrenia ↵
- National Institute of Mental Health. (2024). Schizophrenia. U.S. Department of Health and Human Services. https://www.nimh.nih.gov/health/topics/schizophrenia ↵
- American Psychiatric Association. (2022). Desk reference to the diagnostic criteria from DSM-5-TR (5th ed.). American Psychiatric Association Publishing. ↵
- American Psychiatric Association. (2022). Desk reference to the diagnostic criteria from DSM-5-TR (5th ed.). American Psychiatric Association Publishing. ↵
- “Schizophrenia.png” by William A. Ursprung is in the Public Domain. ↵
- National Institute of Mental Health. (2024). Schizophrenia. U.S. Department of Health and Human Services. https://www.nimh.nih.gov/health/topics/schizophrenia ↵
- National Institute of Mental Health. (2024). Schizophrenia. U.S. Department of Health and Human Services. https://www.nimh.nih.gov/health/topics/schizophrenia ↵
- National Institute of Mental Health. (2024). Schizophrenia. U.S. Department of Health and Human Services. https://www.nimh.nih.gov/health/topics/schizophrenia ↵
- Tandon, R., Nasrallah, H., Akbarian, S., Carpenter, W. T., DeLisi, L. E., Gaebel, W., Green, M. F., Gur, R. E., Heckers, S., Kane, J. M., Malaspina, D., Meyer-Lindenberg, A., Murray, R., Owen, M., Smoller, J. W., Yassin, W., & Keshavan, M. (2024). The schizophrenia syndrome, circa 2024: What we know and how that informs its nature. Schizophrenia Research. 264, 1-28. doi: 10.1016/j.schres.2023.11.015. ↵
- Patel, S., Khan, M. S., & Hamid, P. (2020). The association between cannabis use and schizophrenia: Causative or curative? A systematic review. Cureus, 12(7), e9309. https://doi.org/10.7759/cureus.9309 ↵
- National Institute of Mental Health. (2024). Schizophrenia. U.S. Department of Health and Human Services. https://www.nimh.nih.gov/health/topics/schizophrenia ↵
- Living Well With Schizophrenia. (2019, July 17). What is psychosis? [Video]. YouTube. All rights reserved. https://youtu.be/Pgsujx2UQl8 ↵
- National Institute of Mental Health. (2024). Schizophrenia. U.S. Department of Health and Human Services. https://www.nimh.nih.gov/health/topics/schizophrenia ↵
- National Institute of Mental Health. (2020). Schizophrenia. U.S. Department of Health and Human Services. https://www.nimh.nih.gov/health/topics/schizophrenia ↵
- National Institute of Mental Health. (2023). Mental health medications. U.S. Department of Health and Human Services. https://www.nimh.nih.gov/health/topics/mental-health-medications#part_2362 ↵
- National Institute of Mental Health. (2023). Mental health medications. U.S. Department of Health and Human Services. https://www.nimh.nih.gov/health/topics/mental-health-medications#part_2362 ↵
- National Institute of Mental Health. (2023). Mental health medications. U.S. Department of Health and Human Services. https://www.nimh.nih.gov/health/topics/mental-health-medications#part_2362 ↵
- Vasan, S., & Padhy, R. K. (2023). Tardive dyskinesia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK448207/ ↵
- Jibson, M. D. (2021). Second-generation antipsychotic medications: Pharmacology, administration, and side effects. UpToDate. www.uptodate.com ↵
- Jibson, M. D. (2021). Second-generation antipsychotic medications: Pharmacology, administration, and side effects. UpToDate. www.uptodate.com ↵
- United States. Department of Health and Human Services. Office of Inspector General. (2021). CMS could improve the data it uses to monitor antipsychotic drugs in nursing homes. https://collections.nlm.nih.gov/catalog/nlm:nlmuid-9918384885506676-pdf ↵
- National Institute of Mental Health. (2023). Mental health medications. U.S. Department of Health and Human Services. https://www.nimh.nih.gov/health/topics/mental-health-medications#part_2362 ↵
- Jibson, M. D. (2021). Second-generation antipsychotic medications: Pharmacology, administration, and side effects. UpToDate. www.uptodate.com ↵
- Jibson, M. D. (2021). Second-generation antipsychotic medications: Pharmacology, administration, and side effects. UpToDate. www.uptodate.com ↵
- “Dystonia2010.JPG” by James Heilman, MD is licensed under CC BY-SA 3.0 ↵
- Lewis, K., & O'Day, C. S. (2023). Dystonic reactions. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK531466/ ↵
- Vasan, S., & Padhy, R. K. (2023). Tardive dyskinesia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK448207/ ↵
- Pontone, G. (2020). Treating tardive dyskinesia: A clinical conundrum and new approaches. Drug Induced Disorders: The Clinical Essentials. Psychopharmacology Institute. https://psychopharmacologyinstitute.com/section/treating-tardive-dyskinesia-a-clinical-conundrum-and-new-approaches-2557-4810#:~:text=Clonazepam%20probably%20improves%20tardiv ↵
- Alliance for Patient Access. (2019, October 14). Understanding tardive dyskinesia [Video]. YouTube. All rights reserved. https://youtu.be/gBCiWt-4Cm4 ↵
- Chokhawala, K., & Stevens, L. (2023). Antipsychotic medications. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK519503/ ↵
- TownsendTeaching. 2022, August 28). Neuroleptic malignant syndrome in 3 minutes [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=s73S6o4wlE0 ↵
- Chokhawala, K., & Stevens, L. (2023). Antipsychotic medications. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK519503/ ↵
- Health Link. (2019, December 31). What is metabolic syndrome? [Video]. YouTube. All rights reserved. https://youtu.be/fVMvY_Lsqzw ↵
- National Institute of Mental Health. (2023). Mental health medications. U.S. Department of Health and Human Services. https://www.nimh.nih.gov/health/topics/mental-health-medications#part_2362 ↵
- National Institute of Mental Health. (2024). Schizophrenia. U.S. Department of Health and Human Services. https://www.nimh.nih.gov/health/topics/schizophrenia ↵
- National Institute of Mental Health. (2020, May). Schizophrenia. U.S. Department of Health and Human Services. https://www.nimh.nih.gov/health/topics/schizophrenia ↵
- National Institute of Mental Health. (2024). Schizophrenia. U.S. Department of Health and Human Services. https://www.nimh.nih.gov/health/topics/schizophrenia ↵
- National Institute of Mental Health. (n.d.). What is psychosis? U.S. Department of Health and Human Services. https://www.nimh.nih.gov/health/topics/schizophrenia/raise/what-is-psychosis ↵
- National Institute of Mental Health. (n.d.). Raise researchers. U.S. Department of Health and Human Services. ↵
- National Institute of Mental Health. (n.d.). What is psychosis? U.S. Department of Health and Human Services. https://www.nimh.nih.gov/health/topics/schizophrenia/raise/what-is-psychosis ↵
- Ayano, G., Tesfaw, G., & Shumet, S. (2019). The prevalence of schizophrenia and other psychotic disorders among homeless people: A systematic review and meta-analysis. BMC Psychiatry, 19(370). https://doi.org/10.1186/s12888-019-2361-7 ↵
- “HomelessParis_7032101.jpg” by Eric Pouhier is licensed under CC BY-SA 2.5 ↵
- National Institute of Mental Health. (2024). Schizophrenia. U.S. Department of Health and Human Services. https://www.nimh.nih.gov/health/topics/schizophrenia ↵
Mental illness characterized by periods of psychosis for at least six months.
Include hallucinations, delusions, thought disorders, disorganized speech, and alterations in behaviors.
Refers to loss of motivation, disinterest or lack of enjoyment in daily activities, social withdrawal, difficulty showing emotions, and difficulty functioning normally.
Refers to problems in attention, concentration, and memory.
A state of unresponsiveness due to a person’s mental state.
Treat positive symptoms of schizophrenia and have several potential adverse effects due to their tight binding to dopamine receptors.
Treat both positive and negative symptoms of schizophrenia.
Extremely low white blood cell count.
Refer to akathisia (agitation, distress, and restlessness), rigidity, bradykinesia (slowed movement), tremor, and dystonia (involuntary contractions of muscles of the extremities, face, neck, abdomen, pelvis, or larynx in either sustained or intermittent patterns that lead to abnormal movements or postures).
Motor restlessness.
Slowed movement.
Involuntary contractions of muscles of the extremities, face, neck, abdomen, pelvis, or larynx in either sustained or intermittent patterns that lead to abnormal movements or postures.
A syndrome of movement disorders that can occur in clients taking first-generation antipsychotics.
A rare but fatal adverse effect that can occur at any time during treatment with antipsychotics. Signs include increased temperature, severe muscular rigidity, confusion, agitation, hyperreflexia, elevation in white blood cell count, elevate creatinine phosphokinase, elevated liver enzymes, myoglobinuria, and acute renal failure.
A cluster of conditions that occur together, increasing the risk of heart disease, stroke, and type 2 diabetes.
Recovery-oriented treatment programs for people with first-episode psychosis, an early stage of schizophrenia.

