16.2 Community Health Concepts
Community Health Nursing
Community health nurses work in diverse settings, including public health agencies, schools, and faith-based organizations. Their roles vary but share a common goal: promoting health and addressing the needs of populations within their communities.
Public health nurses work across various settings in the community such as government agencies, community-based centers, shelters, and vaccine distribution sites. They provide disease prevention and health promotion services, such as working with mothers and children to improve nutrition, operating immunization clinics, and leading public health education initiatives such as smoking cessation campaigns. Public health nurses also prepare to respond quickly to public health emergencies such as natural disasters or epidemics.[1],[2] Emergency preparedness is further discussed in the “Environmental Health and Emergency Preparedness” chapter. See Figure 16.2[3] for an image of a community health nurse providing health screenings in a maternal and child health clinic.

School nurses provide a specialized practice of nursing that protects and promotes student health, facilitates
optimal development, and advances academic success. School nurses, grounded in ethical and evidence-based practice, are the leaders who bridge health care and education, provide care coordination, advocate for quality student-centered care, and collaborate to design systems that allow individuals and communities to develop their full potentials. School nurses provide direct health care, administer medications and treatments, develop health care plans and emergency action plans, provide health screenings, collaborate with parents and medical providers, promote student health and safety, and so much more. For example, school nurses may help develop disaster plans that coordinate activities in the school with the larger neighborhood.[4],[5]
Parish nurses, also known as faith community nurses, integrate professional nursing with spiritual care to promote holistic health within faith-based communities. Serving in both paid and volunteer roles, they work primarily within churches, addressing the physical, emotional, and spiritual needs of their congregations. Their responsibilities encompass administering vaccinations, assisting with end-of-life care discussions, coordinating among health care providers, and leading support groups. Additionally, they visit congregation members in homes or hospitals, offering spiritual support during health challenges. By acting as liaisons between health care systems and congregations, parish nurses advocate for quality, client-centered care while honoring individuals’ spiritual beliefs.
Beyond church settings, parish nurses contribute to community health by working in hospitals, long-term care facilities, medical clinics, and social service agencies. In hospitals and long-term care environments, they often collaborate with chaplains to provide comprehensive spiritual care. Their unique role emphasizes integrating faith and health, transforming faith communities into sources of healing and support.[6]
Barriers for Community Health Nurses
Community health nurses play a crucial role in identifying the health needs of a community and planning and implementing preventative health initiatives. However, they often face specific challenges when providing care to individuals, families, and community members. Three key barriers are gaining entry, role negotiation, and confidentiality:
- Gaining Entry: Community health nurses may be considered “outsiders” as representatives of the established health care system and may not necessarily be trusted by community members. It is vital for community health nurses to build trust and supportive relationships. When working with individuals and families, nurses should assess specific community issues affecting that individual’s health or their access to health care and then address those issues in their nursing care plan. Nurses can also investigate if there are community resources available to refer the client and/or their family members for additional services. See Figure 16.3[7] for an image of Red Cross volunteers working with caregivers of clients receiving palliative care.

- Role Negotiation and Confidentiality: Community health nurses must separate their roles as data collectors, health professionals, and neighbors. These roles can be difficult to differentiate when the nurse is assessing community health needs and providing nursing interventions for a population of individuals within their own home community. These individuals may include family members, friends, neighbors, or peers. Trust must be established and confidentiality assured according to legal and ethical parameters of nursing practice. Nurses should also establish a sense of partnership and encourage clients to participate in planning preventative health strategies for themselves and their families.
Other barriers that community health nurses may experience include limited resources and funding, workforce shortages, staff burnout, and feelings of isolation from the healthcare community.[8]
Community Health
Community health nursing is grounded in key principles: promoting healthy living, preventing illness, facilitating rehabilitation, evaluating community resources, and advocating for overall health improvement.[9],[10] In this manner, community health nurses pursue health equity. Health equity means that everyone has a fair and just opportunity to be as healthy as possible. This requires removing potential obstacles to obtaining and maintaining optimal health such as lack of access to health care services, good jobs with fair pay, quality education and housing, and safe environments.[11] Community health nurses address these conditions that are also known as social determinants of health.
Social determinants of health (SDOH) are the conditions in which people are born, grow, work, live, and age. Research shows that the SDOH can be more important than health care or lifestyle choices in influencing health and account for 30-55% of health outcomes.[12] See an illustration of SDOH in Figure 16.4.[13] SDOH can contribute to health inequities, defined as avoidable differences in health status seen within and between communities. In countries at all levels of income, health and illness follow a social gradient: the lower the socioeconomic position, the worse the health. According to the World Health Organization, SDOH can influence health equity in positive and negative ways[14]:
- Income and social protection
- Education
- Unemployment and job insecurity
- Working life conditions
- Food insecurity
- Housing, basic amenities, and the environment
- Early childhood development
- Social inclusion and nondiscrimination
- Structural conflict
- Access to affordable health services of decent quality

Health disparities are health differences that are linked with social, economic, and/or environmental disadvantages. Health disparities adversely affect groups of people who often experience greater obstacles to health based on individual characteristics such as socioeconomic status, age, gender, culture, religion, mental illness, disability, sexual orientation, or gender identity.[15] These groups are often referred to as “vulnerable groups,” and their care is further discussed in the “Vulnerable Populations” chapter.
Community health nurses aim to promote health equity by addressing social determinants of health (SDOH), health disparities, and inequities in the communities they serve. They begin by assessing the community context, as it influences how members respond to public health initiatives. Key community context factors are as follow:
- Physical aspects: Consider the geographic and man-made features present in the community. How do these features influence residents’ access to health care and essential services, as well as the community health nurse’s ability to reach those residents?
- Example: Is the community rural, requiring residents to travel long distances for medical care?
- Infrastructure: Assess the condition of local roads, bridges, and public transit options, as well as the availability of utilities like Internet, electricity, and cellular service.
- Example: Are buses or rideshare services available for residents to reach health care facilities?”
- Patterns of settlement, commerce, and industry: Examine how residential and commercial areas are distributed. Are there neighborhoods located near heavy industry or areas with higher crime rates or defined by economic status?
- Example: Is there a residential area adjacent to a factory that may contribute to air pollution?”
- Demographics: Evaluate key population characteristics such as age, gender, race, ethnicity, language, and household composition.
- Example: Does the community feature multi-generational households?
- History: Reflect on the historical events and traditions that shape community identity.
- Example: Are there monuments or parks that honor local historical events or figures?
- Community leaders, both informal and formal: Understand the shared norms, traditions, and values that guide behavior in the community.
- Example: Is there an annual celebration or parade that reinforces community identity?
- Community culture, both informal and formal: What are the spoken and unspoken rules and traditions of the community?
- For example, does the community have a tradition of celebrating Memorial Day with a parade and public tributes at a local cemetery?
- Existing groups and organizations: Consider the presence of local clubs, community centers, and organizations that can facilitate collaboration and support.
- Example: Is there a YMCA or similar organization promoting physical activity?
- Existing institutions: Identify essential institutions—such as hospitals, clinics, schools, libraries, and religious centers—and assess their accessibility and leadership.
- Example: Is there an urgent care clinic easily accessible by public transit?
- Economics: Review the community’s economic base, including predominant industries and employment patterns, as well as wealth distribution.
- Example: Is the area predominantly working class, with most residents employed in local factories?
- Government/Politics: Consider the influence and engagement of political leaders and the nature of governance in the community.
- Example: How does the mayor communicate with residents?
- Social structure: Analyze how community members interact on a daily basis, including conflict resolution and symbols of respect.
- Example: Does the town board meet regularly to discuss local issues and make decisions collaboratively?
- Attitudes and values: Investigate what the community prioritizes and any prevailing assumptions or biases regarding behavior and interaction.
- Example: Is it commonly expected that neighbors will help each other during community challenges, such as after a storm?
According to the CDC, a healthy community is one in where local groups work together to prevent disease and promote healthy living. This approach benefits the largest number of people and helps reduce health disparities caused by differences in income, education, race, location, and other factors.[16]
Community Health Needs Assessment
Community health needs assessment is a systematic process to identify and analyze community health needs and assets in order to prioritize these needs, plan, and act upon significant unmet community health needs.[17] A community health assessment gives nurses and community organizations comprehensive information about the community’s current health status, needs, and issues. This information can be used to develop a community health improvement plan by justifying how and where resources should be allocated to best meet community needs.[18] Community health needs assessments are performed and reported at national, state, county, and local levels.
National Health Needs Assessments
Healthy People 2030 addresses the most current national public health priorities. It is published by the United States Department of Health and Human Services Office of Disease Prevention and Promotion. See Figure 16.5[19] for an illustration related to using Healthy People 2030 objectives and leading health indicators to assess community needs data, plan, and evaluate community health interventions.

A set of evidence-based Healthy People objectives are published every ten years based on current national data. Objectives are classified by categories[20]:
- Health Conditions
- Health Behaviors
- Populations
- Settings and Systems
- Social Determinants of Health
Examples of Healthy People 2030 community objectives include the following[21]:
- Increase the number of community organizations that provide preventative services
- Increase the rate of bystander CPR and AED use for nontraumatic cardiac arrests in public places
- Increase the proportion of adult stroke survivors who participate in rehabilitation services
Leading Health Indicators (LHIs) are a subset of high-priority Healthy People 2030 objectives to drive action toward improving health and well-being. Most LHIs address important factors that impact major causes of death and disease in the United States. They help organizations, communities, and community health nurses focus their resources and efforts to improve the health and well-being of all people. There are 23 LHIs that cover the life span from infants, children, adolescents, adults, and older adults. See a list of LHIs in Table 16.2.
Table 16.2. Leading Health Indicators Across the Life Span
| Life Stage | Leading Health Indicator |
|---|---|
| Infant |
|
| Children and Adolescents |
|
| Adults and Older Adults |
|
| All Ages |
|
Healthy People 2030 Resources
View Healthy People 2030 Objectives, Community Objectives, and Leading Health Indicators.
State Needs Assessments
States perform health needs assessments to develop state funding and program priorities for community health. For example, the Wisconsin Department of Health Services (DHS) performs a mental health and substance abuse needs assessment every other year. Data in this report includes the following:
- Prevalence of Needs: The prevalence of disorders, conditions, and associated problems for the entire population and subpopulations
- Access to Services: Determination of which and how many services are received by individuals and exploration of barriers to access
- Service Workforce and Capacity: Examination of the mental health and substance use services workforce, including the number of providers of these services and the geographic dispersion of the workforce across the state
Another example of a state needs assessment related to mental health is the Behavioral Health Gaps Study funded by the Wisconsin DHS to assess gaps and needs in the behavioral health service system for individuals with mental health and substance use disorders. Key gaps documented in this study included shortages in child and geriatric psychiatrists; shortages in mental health inpatient beds and residential facilities for treating substance use; inadequacies of the medical transportation system; a need for improving crisis stabilization services in the community that focus on reducing contact with police officers; shortages in medication-assisted treatment providers and clinics; long waitlists across the service array; shortages in competent translation services; and the need to provide wraparound services, particularly for consumers with families.[22]
Explore your state’s health needs assessments. Examples of health needs assessments in the state of Wisconsin are as follows:
Department of Health Service’s Mental Health and Substance Abuse Needs Assessment PDF
The Behavioral Health Gaps Report for the State of Wisconsin PDF completed by University of Wisconsin-Madison Population Health Institute
County Health Rankings
County health rankings are created annually by the University of Wisconsin Population Health Institute for counties across the country.[23] These rankings provide a snapshot of a community’s health and can be used as a starting point for implementing change to promote health equity in communities. See the following box to explore the health ranking for your community.
Visit the Explore Health Rankings web page from the University of Wisconsin Population Health Institute to view the health ranking of your community.
Local Needs Assessments
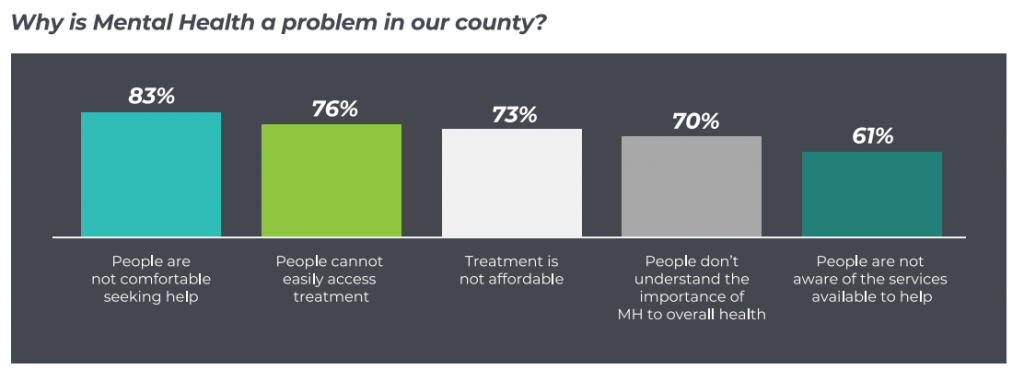
Local communities perform health needs assessments and develop specific health initiatives for their community members. For example, the Eau Claire County Health Department Needs Assessment was used to create a county health plan. In 2021 the top health priorities were documented as drug use, mental health, alcohol misuse, obesity, and healthy nutrition. See Figure 16.6[24] with an image related to data from a county mental health needs assessment.
Explore your community’s health initiatives. View the example of Eau Claire City-County Health Department Needs Assessment.
Hospitals’ Community Health Needs Assessments
Tax-exempt hospitals are required to conduct community health needs assessments according to the Patient Protection and Affordable Care Act (i.e., the Affordable Care Act). Hospitals are required to adopt implementation strategies to meet the community health needs identified through their needs assessment. This collaboration among hospitals and community partners expands the community’s capacity to address health needs through a shared vision and creates a foundation for coordinated efforts to improve community health.[25]
- Greenwood, B. (n.d.). What are the primary roles of the community nurse? CHRON. https://work.chron.com/primary-roles-community-nurse-15144.html ↵
- National Academy of Medicine. (2021). The future of nursing 2020-2030: Charting a path to achieve health equity [PDF Report]. https://www.phnurse.org/assets/docs/FON%20Valuing%20Community%20and%20Public%20Health%20Nursing.pdf ↵
- “PIXNIO-45563-3000x2000” by USAID on Pixnio is licensed under CC0 ↵
- Greenwood, B. (n.d). What are the primary roles of the community nurse? CHRON. https://work.chron.com/primary-roles-community-nurse-15144.html ↵
- National Academy of Medicine. (2021). The future of nursing 2020-2030: Charting a path to achieve health equity [PDF Report]. https://www.phnurse.org/assets/docs/FON%20Valuing%20Community%20and%20Public%20Health%20Nursing.pdf ↵
- Greenwood, B. (n.d.). What are the primary roles of the community nurse? CHRON. https://work.chron.com/primary-roles-community-nurse-15144.html ↵
- “10716898813_74292ef548_k” by Department of Foreign Affairs and Trade is licensed under CC BY 2.0 ↵
- Seyedfatemi, N., Peyrovi, H., Goharinezhad, S., & Oghli, S. H. (2024). Barriers and facilitators of community-based nursing development: A scoping review. Journal of Education and Health Promotion, 3, 488. doi: 10.4103/jehp.jehp_1329_23. ↵
- Greenwood, B. (n.d.). What are the primary roles of the community nurse? CHRON. https://work.chron.com/primary-roles-community-nurse-15144.html ↵
- National Academy of Medicine. (2021). The future of nursing 2020-2030: Charting a path to achieve health equity [PDF Report]. https://www.phnurse.org/assets/docs/FON%20Valuing%20Community%20and%20Public%20Health%20Nursing.pdf ↵
- Braveman, P., Arkin, E., Orleans, T., Proctor, D., & Plough, A. (2017). What is health equity? Robert Wood Johnson Foundation. https://www.rwjf.org/en/library/research/2017/05/what-is-health-equity-.html ↵
- World Health Organization. (n.d.). Social determinants of health. https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1 ↵
- “Healthy People 2030 SDOH Graphic.png” by U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion is in the Public Domain. Access for free at https://health.gov/healthypeople/objectives-and-data/social-determinants-health ↵
- World Health Organization. (n.d.). Social determinants of health. https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1 ↵
- HealthyPeople.gov. (2022). Disparities. Office of Disease Prevention and Health Promotion, U.S. Department of Health and Human Services. https://odphp.health.gov/healthypeople ↵
- Centers for Disease Control and Prevention. (2015). A healthy community is a prepared community. [Blog]. https://blogs.cdc.gov/publichealthmatters/2015/09/a-healthy-community-is-a-prepared-community/ ↵
- Vigna, A. J. (2020). The 2019 behavioral health gaps report for the state of Wisconsin. University of Wisconsin Population Health Institute. https://uwphi.pophealth.wisc.edu/publications-2/evaluation-reports-2/. ↵
- VHA Inc., & Healthy Communities Institute. (2013). Assessing & addressing community health needs. Catholic Heart Association of the United States. https://www.chausa.org/docs/default-source/general-files/cb_assessingaddressing-pdf.pdf?sfvrsn=4 ↵
- “HP2030_HowtoUse_Screen1_2020-03-24.png” by unknown author for U.S. Department of Health and Human Services is in the Public Domain. Access for free at https://health.gov/our-work/national-health-initiatives/healthy-people/healthy-people-2030/promoting-healthy-people-2030. ↵
- Office of Disease Prevention and Health Promotion. (2024). Healthy People 2030: Building a healthier future for all. U.S. Department of Health and Human Services. https://health.gov/healthypeople ↵
- Office of Disease Prevention and Health Promotion. (2024). Healthy People 2030: Building a healthier future for all. U.S. Department of Health and Human Services. https://health.gov/healthypeople ↵
- Vigna, A. J. (2020). The 2019 behavioral health gaps report for the state of Wisconsin. University of Wisconsin Population Health Institute. https://uwphi.pophealth.wisc.edu/publications-2/evaluation-reports-2/. ↵
- Vigna, A. J. (2020). The 2019 behavioral health gaps report for the state of Wisconsin. University of Wisconsin Population Health Institute. https://uwphi.pophealth.wisc.edu/publications-2/evaluation-reports-2/. ↵
- This image is derived from 2021 Eau Claire County Community Health Assessment by Community Health Assessment Planning Partnership Committee and is in the Public Domain. ↵
- VHA Inc., & Healthy Communities Institute. (2013). Assessing & addressing community health needs. Catholic Heart Association of the United States. https://www.chausa.org/docs/default-source/general-files/cb_assessingaddressing-pdf.pdf?sfvrsn=4 ↵
Nurses who work across various settings in the community such as government agencies, community-based centers, shelters, and vaccine distribution sites.
Provide a specialized practice of nursing which protects and promotes student health, facilitates optimal development, and advances academic success.
Nurses who integrate professional nursing with spiritual care to promote holistic health within faith-based communities; also known as faith community nurses.
Everyone has a fair and just opportunity to be as healthy as possible.
Conditions in which people are born, grow, work, live, and age.
Avoidable differences in health status seen within and between communities.
Health differences that are linked with social, economic, and/or environmental disadvantages.
Local groups from all parts of the community work together to prevent disease and make healthy living options accessible.
Systematic process to identify and analyze community health needs and assets in order to prioritize these needs, plan, and act upon significant unmet community health needs.

