3.6 Cephalosporins
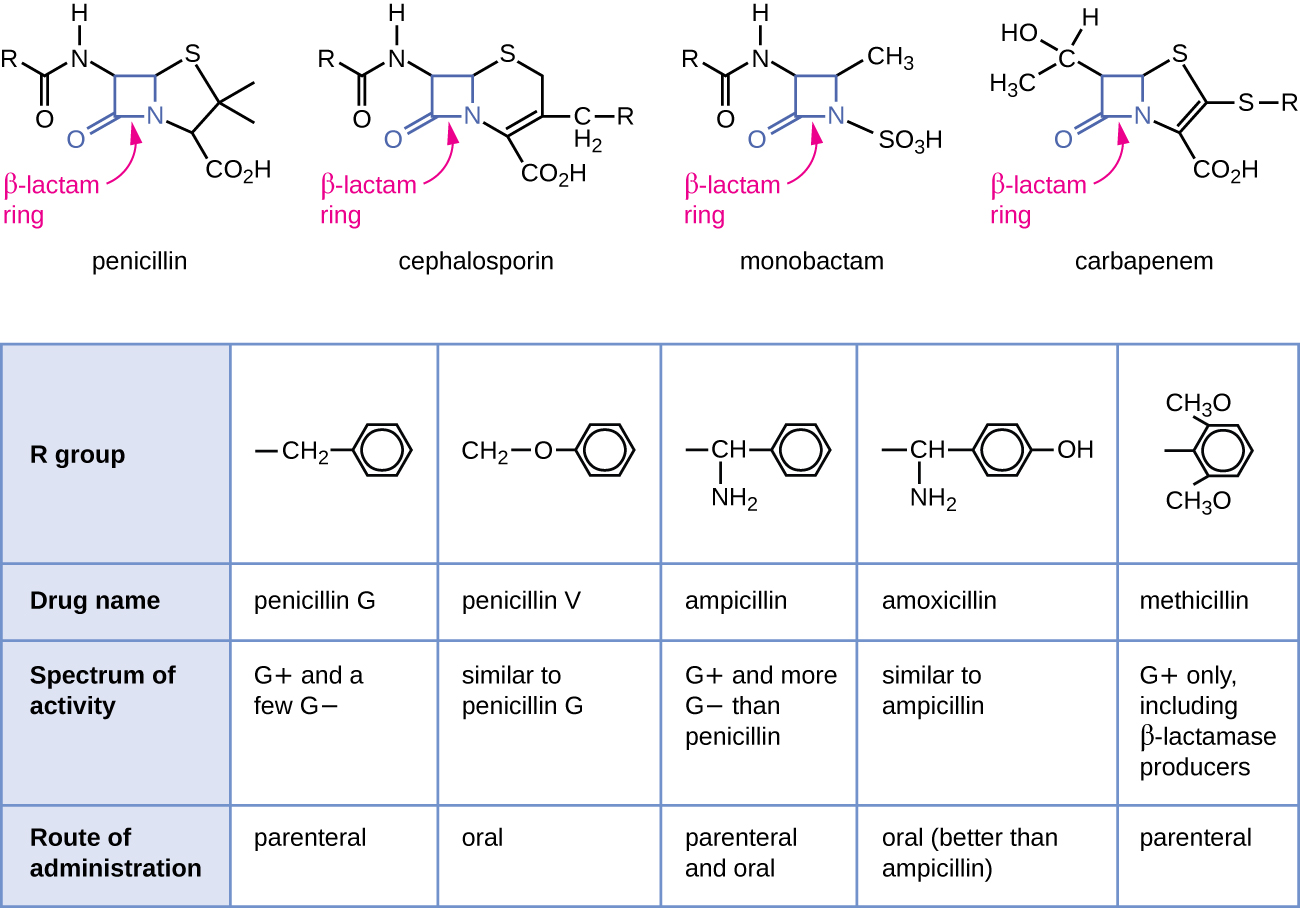
Cephalosporins are a slightly modified chemical “twin” to penicillins due to their beta-lactam chemical structure. See Figure 3.6[1] for a comparison of the beta-lactam ring structure, spectrum of activity, and route of administration across different classes of medications. Because of these similarities in chemical structure, some clients who have severe allergies to penicillins may experience cross-sensitivity to cephalosporins. Nurses should review the type and severity of a client’s previous reaction to penicillin to determine if administering cephalosporin is appropriate.
Mechanism of Action: Cephalosporins are typically bactericidal and are similar to penicillin in their action within the cell wall. Cephalosporins are sometimes grouped into “generations” by their antimicrobial properties. The 1st-generation drugs are effective mainly against gram-positive organisms. Higher generations generally have expanded spectra against aerobic gram-negative bacilli. The 5th-generation cephalosporins are active against methicillin-resistant Staphylococcus aureus (MRSA) or other complicated infections.[2]
Indications: Cephalosporins are used to treat skin and skin-structure infections, bone infections, genitourinary infections, otitis media, and community-acquired respiratory tract infections.
Nursing Considerations: Clients who are allergic to pencillins may also be allergic to cephalosporins. Clients who consume cephalosporins while drinking alcoholic beverages may experience disulfiram-like reactions, including severe headache, flushing, nausea, vomiting, etc.[3] Additionally, like penicillins, cephalosporins may interfere with coagulability and increase a client’s risk of bleeding. Cephalosporin dosing may require adjustment for clients experiencing renal impairment. Blood urea nitrogen (BUN) and creatinine should be monitored carefully to identify signs of nephrotoxicity.
Side Effects/Adverse Effects: Common side effects of cephalosporin medications include gastrointestinal upset including nausea, vomiting, and diarrhea. Additionally, nurses should monitor for rash, C-diff, and nephrotoxicity. Cephalosporins may also elevate a client’s INR and increase bleeding risk. Nurses should also monitor for low blood cell counts and hemolytic anemia.
Health Teaching & Health Promotion: Clients who are prescribed cephalosporins should be specifically cautioned about a disulfiram reaction, which can occur when alcohol is ingested while taking the medication. Additionally, individuals should be instructed to monitor for rash and signs of superinfection (such as vaginal itching or discharge indicating a yeast infection or loose or foul-smelling stool indicating C-diff) and report these symptoms to the prescribing provider.
It is also important to note that cephalosporin can enter breastmilk and may alter bowel flora of the infant. Thus, use during breastfeeding is often discouraged.[4]
Now let’s take a closer look at the cephalosporin medication grid in Table 3.6.[5]
Table 3.6 Cephalosporin Medication Grid
Class/Subclass |
Prototype/Generic |
Nursing Considerations |
Therapeutic Effects |
Side/Adverse Effects |
|---|---|---|---|---|
| Cephalosporins | 1st-generation:
2nd-generation: 3rd-generation: 4th-generation: 5th-generation: |
Check for allergies, including if allergic to penicillin
Dosage adjustment if renal impairment Use with caution with seizure disorder PO: Administer without regard to food; if GI distress, give with food IV: Reconstitute drug with sterile water or normal saline per manufacturer instructions; shake well until dissolved. Inject into large vein or free-flowing IV solution over 3-5 minutes Drug interaction: Anticoagulants |
Monitor for systemic signs of infection:
-WBCs -Fever Monitor actual site of infection Monitor culture results, if obtained |
Common side effects:
-Nausea -Vomiting -GI upset -Diarrhea Monitor for: -Rash -Yeast infection -C-diff Nephrotoxicity if preexisting renal disease Elevated INR and bleeding risk Development of hemolytic anemia |
Critical Thinking Activity 3.6
Using the above grid information, consider the following clinical scenario question:
An 89-year-old client is admitted to the medical-surgical floor for treatment of a skin infection. The admitting provider prescribes Cefazolin 1 gram every 8 hours IV.
The client’s laboratory tests including renal studies include:
Creatinine: 1.3 mg/dL (Normal range: 1.2 mg/dL)[6]
Blood urea nitrogen (BUN): 25 mg/dL (Normal: 8-20 mg/dL)
Glomerular Filtration Rate: 55 mL/min (Normal: 90-120 mL/min)[7]
On Day 3, the renal laboratory studies are repeated. The results are:
Creatinine: 1.6 mg/dL
Blood urea nitrogen (BUN): 57 mg/dL
Glomerular Filtration Rate: 20 mL/min
Are Day 3 findings expected or not? What course of action should the nurse take?
Note: Answers to the Critical Thinking activities can be found in the “Answer Key” section at the end of the book.
- “OSC Microbio 14 02 BetaLactam.jpg” by CNX Openstax is licensed under CC BY 4.0 Access for free at https://openstax.org/books/microbiology/pages/14-3-mechanisms-“of-antibacterial-drugs ↵
- Werth, B. J. (2018, August). Cephalosporins. Merck Manual Professional Version. https://www.merckmanuals.com/professional/infectious-diseases/bacteria-and-antibacterial-drugs/cephalosporins ↵
- Ren, S., Cao, Y., Zhang, X., Jiao, S., Qian, S., & Liu, P. (2014). Cephalosporin induced disulfiram-like reaction: A retrospective review of 78 cases. International Surgery, 99(2), 142–146. https://www.internationalsurgery.org/doi/full/10.9738/INTSURG-D-13-00086.1 ↵
- uCentral from Unbound Medicine. https://www.unboundmedicine.com/ucentral ↵
- This work is a derivative of DailyMed by U.S. National Library of Medicine in the Public Domain. ↵
- U.S. National Library of Medicine, Medline Plus. (2020, February 13). Basic metabolic panel. https://medlineplus.gov/ency/article/003462.htm ↵
- U.S. National Library of Medicine, Medline Plus. (2020, February 13). Glomerular filtration rate. https://medlineplus.gov/ency/article/007305.htm ↵

