7.9 Spotlight Application
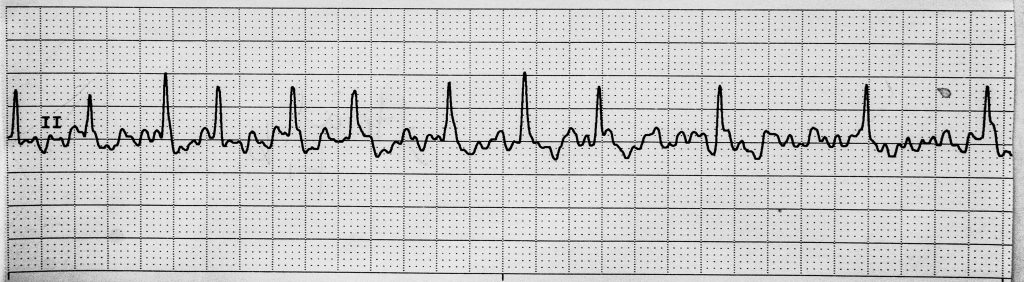
A 65-year-old male client with no past cardiac medical history comes into the Emergency Department complaining of palpitations and shortness of breath. He tells the triage nurse it started about two hours ago. He states he has felt these palpitations before, but they always went away after about ten minutes. The nurse attaches the ECG leads and connects the monitor. The rhythm in Figure 7.36[1] appears on the monitor.
Reflection Questions:
- Interpret this cardiac rhythm.
- Does this rhythm require emergency assistance?
- Is this client a candidate for defibrillation or synchronized cardioversion?
Answers:
Here are the steps the nurse took to interpret this rhythm:
- The nurse calculates the ventricular rate of 120 beats per minute by counting 12 R waves in the 6-second strip (i.e., over 30 large boxes) and multiplies this by 10 to reach 120. The atrial rate cannot be calculated because there are no discernible P waves.
- The nurse classifies this rhythm as an irregularly irregular rhythm because the R waves are not equal distances apart.
- The nurse assesses the P waves. There are no P waves present, so these heartbeats are not originating in the SA node.
- The PR interval cannot be calculated because there are no P waves.
- The QRS duration ranges between 0.04 to 0.12 seconds (1 – 3 small boxes).
- The T waves cannot be evaluated in this lead because the quivering atria (i.e., P waves) obscure them.
- The ST segment cannot be evaluated in this lead because of the lack of discernible T waves.
- The QT interval cannot be evaluated in this lead because of the lack of discernible T waves.
- The quivering waves on the ECG strip between the R waves indicate the atria are quivering, which is a characteristic of atrial fibrillation.
- The nurse assesses the client for signs and symptoms of decreased cardiac output such as decreased blood pressure, decreased peripheral pulses, prolonged capillary refill, dizziness, chest pain, confusion, and loss of consciousness. The client is stable without signs of decreased cardiac output at this time.
The client is diagnosed by the provider with new onset, stable atrial fibrillation. Because the client presented to the hospital within 48 hours of onset, he is a candidate for a synchronized cardioversion. The nurse anticipates an order for administration of anticoagulant medication and to set up for a cardioversion procedure by the cardiologist.
The Rest of the Story:
Cardioversion is completed, and the client successfully returns to a normal sinus rhythm. He is discharged the next day with a follow-up outpatient appointment with cardiology services to ensure he remains in normal sinus rhythm with prescribed medications.
- “Rhythm.jpg” by Deanna Hoyord is licensed under CC BY 4.0 ↵

