7.4 ECG Patterns and Dysrhythmias
Abnormal ECG waveforms indicate dysrhythmias (also referred to as arrhythmias). Some dysrhythmias can significantly affect the client’s clinical status and require rapid nurse response. Early and accurate identification of ECG patterns, assessment of the client’s clinical presentation, and knowledge of the agency’s policies and procedures regarding treatment will ensure clients receive optimal care.
Recall that the electrical conduction system stimulates the mechanical pumping action of the heart. If the ventricles become unable to effectively pump blood to the rest of the body due to altered electrical signals, signs and symptoms of decreased cardiac output occur, such as decreased blood pressure and pulses, prolonged capillary refill, chest pain, shortness of breath, dizziness, confusion, or loss of consciousness. When an ECG demonstrates new abnormal findings, the nurse must immediately assess the client for signs of decreased cardiac output and respond appropriately.
Some dysrhythmias can quickly lead to cardiac arrest, such as ventricular tachycardia, ventricular fibrillation, and third-degree heart block. The nurse must be aware of which rhythms require emergency assistance.
Medical treatments for symptomatic dysrhythmias can include antidysrhythmic medications, cardioversion, defibrillation, and/or implantation of medical devices such as pacemakers and implantable cardioverter defibrillators (ICDs). Cardioversion and defibrillation are further discussed in the “Cardioversion and Defibrillation” section of this chapter.
ECG patterns are generally classified into three categories depending on whether the signal originates from the SA node (i.e, sinus rhythms), the atria (i.e., atrial rhythms), or the ventricles (i.e., ventricular rhythms). Additionally, heart blocks refer to blocks in the normal pathway of electrical conduction through the heart and can be categorized as sinus node, atrioventricular (AV) node, or bundle branch blocks. The characteristics of each of these types of rhythms and blocks are further discussed in the following sections. A table summarizing the ECG images discussed in this chapter can be found in the “Appendix of Rhythm Strips.”
Sinus Rhythms
Sinus rhythm is a regular rhythm, but the rate varies depending on autonomic nervous system regulation of the sinus node. When the rhythm is regular but there is an abnormal rate, it is called “sinus arrhythmia.” Sinus arrhythmias include sinus tachycardia and sinus bradycardia. Characteristics and treatment of sinus rhythms are summarized in Table 7.4a at the end of this subsection.
Normal sinus rhythm (NSR) originates from the sinus node and describes the characteristic rhythm of a healthy human heart. All components of the ECG waveform are within normal limits. See Figure 7.16[1] for an image of normal sinus rhythm.

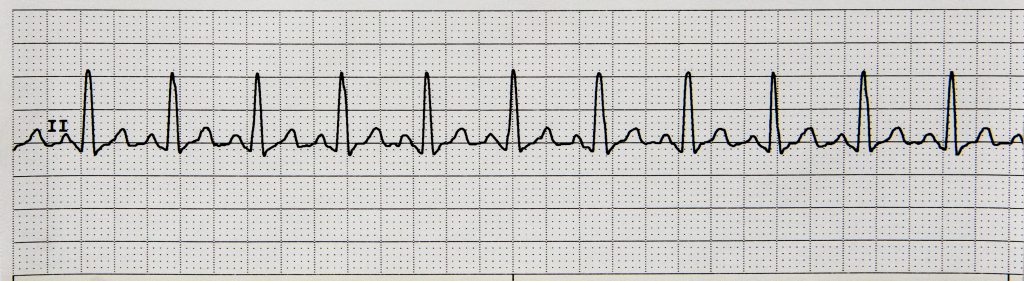
A sinus rhythm faster than a normal rate (i.e., greater than 100 in adults) is called a sinus tachycardia. Sinus tachycardia is commonly caused by stress, exercise, alcohol, caffeine, and tobacco and can be resolved by addressing these causes. However, sinus tachycardia can also be caused by conditions such as hypovolemia, anemia, fever/infection, decreased oxygenation, cardiac conditions, and some medications, requiring nursing action depending upon the cause. See Figure 7.17[2] for an image of sinus tachycardia.
A sinus rhythm with a slower rate than normal range (i.e., less than 60 in an adult) is called a sinus bradycardia. Sinus bradycardia may be asymptomatic and normally occur in athletes due to a well-conditioned heart. However, it can also be symptomatic and signify a new cardiac condition or side effect of cardiac medications, requiring nursing action. See Figure 7.18[3] for an image of sinus bradycardia.

Respiratory sinus arrhythmia is typically a normal finding in young, healthy adults where the heart rhythm correlates to the respiratory cycle. As the client breathes in, the heart rate increases and then the rate slows as they breathe out.
Table 7.4a Characteristics of Normal Sinus Rhythm and Common Sinus Dysrhythmias
| Sinus Rhythms | Patho-
physiology |
Causes | Identification | Symptoms | Nursing Interventions | Medical Treatment | Patient Education |
|---|---|---|---|---|---|---|---|
| Normal Sinus Rhythm (NSR) | Normal conduction of the heart. | N/A | All components are within normal limits. | N/A | N/A | N/A | N/A |
| Sinus Bradycardia[4] | Slowed electrical conduction in the heart. | May occur in well-conditioned athletes. Can also signify a cardiac condition or side effects of cardiac medications requiring nursing action. | All components are within normal limits except the heart rate is less than 60 beats per minute. | Many clients are asymptomatic, but if signs and symptoms occur, they are related to decreased cardiac output. | Assess for adequate cardiac output.
Withhold cardiac medications if indicated and notify the provider. |
If symptomatic, the cause is treated.
Atropine, transcutaneous pacemaker, and placement of a permanent pacemaker may be required for chronic bradycardia. |
Seek medical care for symptoms such as chest pain, shortness of breath, dizziness, confusion, or fainting. |
| Sinus Tachycardia[5] | Fast electrical conduction through the heart, causing lack of filling between each beat. | Often caused by stress, exercise, alcohol, caffeine, and tobacco.
Can also be caused by hypovolemia, anemia, fever/ infection, decreased oxygenation, cardiac conditions, and some medications. |
All components are within normal limits except the heart rate is above 100 beats per minute. | Some clients are asymptomatic. Other clients have palpitations or symptoms of decreased cardiac output. | Assess for adequate cardiac output and notify the provider if indicated.
Educate about lifestyle changes that could cause the rhythm. |
If symptomatic, the underlying cause is treated. Beta-blockers, calcium channel blockers, or sinus ablation may be used to slow the rate. | Eliminate the cause of the rhythm.
Seek medical treatment for symptoms of chest pain, shortness of breath, dizziness, confusion, or loss of consciousness. |
| Respiratory Sinus Arrhythmia[6] | Rhythm correlates to the respiratory cycle; the rate increases when the client breathes in and slows when they breathe out. | Very common in young healthy adults. | All components are within normal limits except the rhythm is irregular and corresponds to the respiratory cycle.
If the client holds their breath, the rhythm reverts to NSR. |
Rare. | Notify the provider if symptomatic. | Typically, no treatment is needed. | This is a sign of a normal functioning heart. |
Atrial Rhythms
Atrial rhythms originate in the atria rather than in the SA node. The P wave is positive, but its shape can be different from a normal sinus rhythm because the electrical impulse follows a different path to the AV (atrioventricular) node. Common atrial arrhythmias include premature atrial contractions, atrial fibrillation, and atrial flutter. Characteristics and treatment of common atrial dysrhythmias are summarized in Table 7.4b at the end of this subsection.
Premature atrial contractions (PAC) are common in older adults and are caused by ectopic beats that originate in the atria. They are not typically treated unless the client becomes symptomatic.
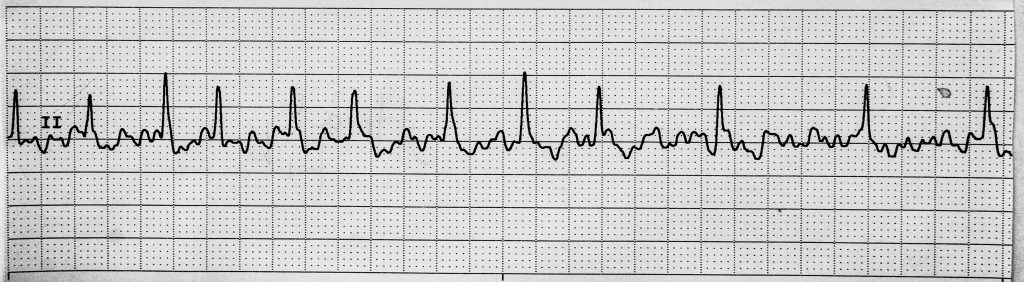
Atrial fibrillation (A-fib) is categorized as an “irregularly irregular rhythm.” It is characterized by atrial quivering, resulting in a lack of P waves. Clients may develop signs and symptoms of decreased cardiac output because the ventricles are not able to fill and pump the appropriate amount of blood with each beat. Nurses should assess for signs of decreased cardiac output, including fatigue, dizziness, syncope, chest pain, and shortness of breath, as well as for new signs of stroke. Clients with A-fib are at risk of stroke due to blood pooling in the atria. See Figure 7.19[7] for an image of atrial fibrillation.
Atrial flutter (A flutter) displays the atrial beats as sawtooth beats, and the PR interval is not measurable. Atrial impulses are fast and regular, with rates between 250-300, and the ventricular rate is not the same as the atrial rate. As a result, the client’s cardiac output decreases because the heart is not able to fill and pump the appropriate amount of blood with each beat. Clients with atrial flutter are also at risk for stroke. See Figure 7.20[8] for an image of atrial flutter.
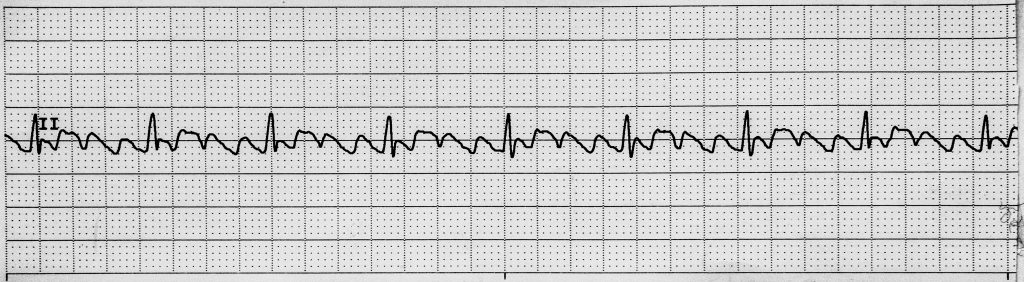
Table 7.4b Characteristics of Common Atrial Dysrhythmias
| Atrial Rhythms | Pathophysiology | Causes | Identification | Symptoms | Nursing Interventions | Treatment | Patient Education |
|---|---|---|---|---|---|---|---|
| Premature Atrial Contractions (PAC)[9] | An ectopic beat that originates in the atria. | Common in older adults; often caused by caffeine, tobacco, anxiety, and electrolyte imbalances. | Early P waves that may be closer than normal to the previous T wave. | Feelings of a skipped beat or palpitations. | Encourage lifestyle changes, such as decreased caffeine, tobacco, and alcohol intake, as well as improved stress management. | If symptomatic, then treatments are prescribed to eliminate the cause. | Seek medical treatment for symptoms of chest pain, shortness of breath, dizziness, confusion, or fainting. |
| Atrial Fibrillation (A-fib)[10] | An irregular heart rhythm originating in the atria characterized by atrial quivering. This rhythm is categorized as an “irregularly irregular rhythm.”
Clients are at increased risk for a stroke due to blood pooling in the atria. |
Coronary artery disease, heart failure, high blood pressure, and cardiac irritability due to ischemia or electrolyte imbalances. | Irregular heart rate with lack of clear P waves and a wavy baseline because they are quivering.
PR interval is not measurable. |
Irregular heartbeat and possible palpitations.
May have signs and symptoms of decreased cardiac output, including fatigue, dizziness, syncope, chest pain, and shortness of breath. |
Be aware that atrial and ventricular rates are different and may affect the accuracy of blood pressure readings on automatic monitors.
Immediately report signs of decreased cardiac output or signs of stroke. |
Medications for stable A-fib include those to control rate and/or rhythm, as well as anticoagulation to prevent strokes.
Treatments of unstable A-fib include cardioversion and/or ablation. A pacemaker may be implanted if bradycardia is present. |
Seek medical care for symptoms of a stroke, such as one-sided weakness or paralysis, slurred speech, or facial drooping.
Seek medical treatment for chest pain, shortness of breath, dizziness, confusion, or fainting. |
| Atrial Flutter (A flutter)[11] | Fast, regular atrial impulses with rates between 250-300. As a result, the heart is not able to fill and pump the appropriate amount of blood with each beat. Clients are at increased risk for stroke. | Coronary artery disease, hypertension, obesity, and heart failure. | Atrial beats appear as sawtooth beats.
PR interval is not measurable. QRS may be regular or irregular. |
Shortness of breath, syncope, palpitations, and dizziness. | Be aware atrial and ventricular rates will be different.
Monitor for signs of decreased cardiac output and stroke. |
If stable, medications are prescribed for rate and/or rhythm control, as well as for anticoagulation to prevent strokes.
If unstable, cardioversion, ablation, and/or a pacemaker may be performed. |
Seek medical care for symptoms of a stroke, such as one-sided weakness or paralysis, slurred speech, or facial drooping.
Seek medical treatment for chest pain, shortness of breath, dizziness, confusion, or fainting. |
Ventricular Rhythms
Ventricular rhythms originate in the ventricles (rather than the SA node) and typically cause the heart to beat faster (i.e., ventricular tachycardia) or quiver (i.e., ventricular fibrillation). There are several different types of ventricular dysrhythmias. Many ventricular dysrhythmias are life-threatening and require immediate emergency response. Common ventricular dysrhythmias include premature ventricular tachycardia (PVC), supraventricular tachycardia, torsades de pointes, ventricular tachycardia (V-tach), and ventricular fibrillation (V-fib). Characteristics and treatment of common ventricular dysrhythmias are summarized in Table 7.4c at the end of this subsection.
Some ventricular dysrhythmias may be unifocal or multifocal. Unifocal dysrhythmias causes the waveforms to look the same because the signal is originating from the same area in the heart, whereas multifocal dysrhythmias cause the waveforms to look different because the impulse is originating from different areas of the heart. Multifocal rhythms are harder to treat and are more dangerous because the impulse is not predictable and multiple areas of the heart are involved.
Premature ventricular contractions (PVC) are caused by ectopic beats that originate in the ventricle, resulting in the appearance of wide, bizarre QRS complexes within an otherwise normal sinus rhythm. Although occasional PVCs are common in healthy adults with no symptoms other than occasional palpitations, increased frequency of PVCs per minute can signal a more serious condition. Bigeminy is a PVC every other beat. Trigeminy is a PVC every third beat. Couplets refer to PVCs occurring in pairs. See Figure 7.21[12] for an image of unifocal PVCs in an otherwise normal sinus rhythm. See Figure 7.22[13] for an image of PVCs occurring in couplets.
R on T phenomenon occurs when a PVC occurs on a T wave and can trigger ventricular tachycardia. Medications or diseases that cause prolonged QT interval can result in R on T phenomenon.
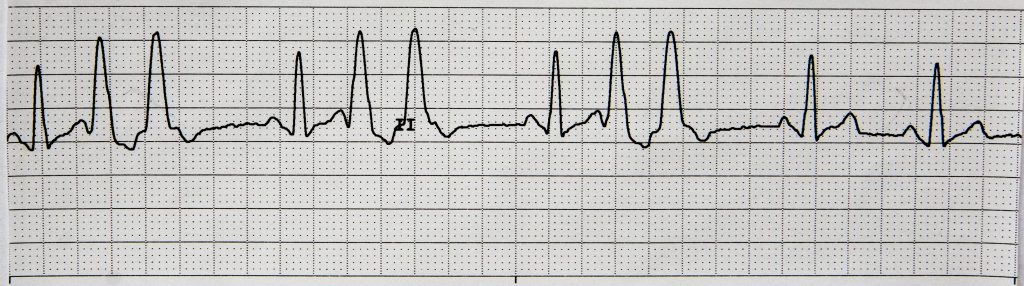
Supraventricular tachycardia (SVT) is characterized by a narrow QRS interval of 0.1 second or less and rapid heart rates over 160 beats per minute. P waves often cannot be identified due to fast rate, and cardiac output may decrease due to the inability of the ventricles to fill and pump blood. See Figure 7.23[14] for an image of supraventricular tachycardia.
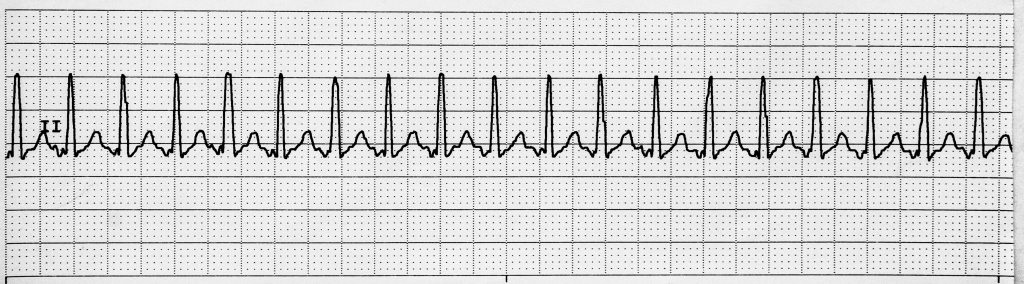
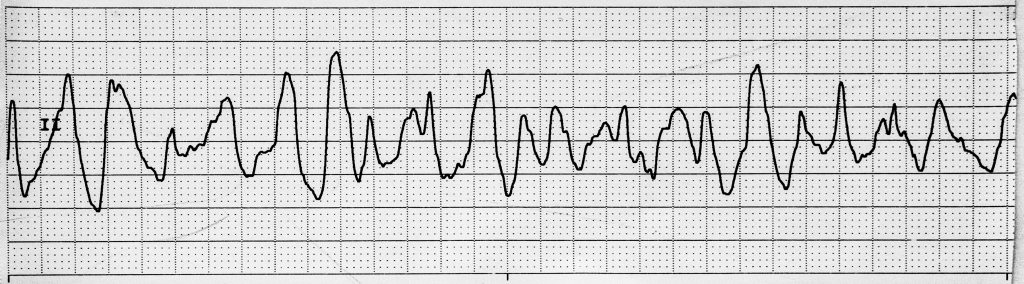
Ventricular tachycardia (V-tach) is characterized by wide QRS complexes without visible P and T waves. The ventricular rate is often over 120 beats per minute, resulting in rapidly worsening cardiac output. The client is only able to tolerate this rapid ventricular rhythm for a short period of time before losing consciousness. V-tach requires emergency response. If the client has a pulse, synchronized cardioversion and/or intravenous antidysrhythmic medications are administered. If the client does not have a pulse, defibrillation is administered. Read details about synchronized cardioversion and defibrillation in the “Cardioversion and Defibrillation” section of this chapter. Read more information about antidysrhythmic medications in the “Antiarrhythmics” section of the “Cardiac and Renal” chapter of Open RN Nursing Pharmacology. See Figure 7.24[15] for an image of ventricular tachycardia.
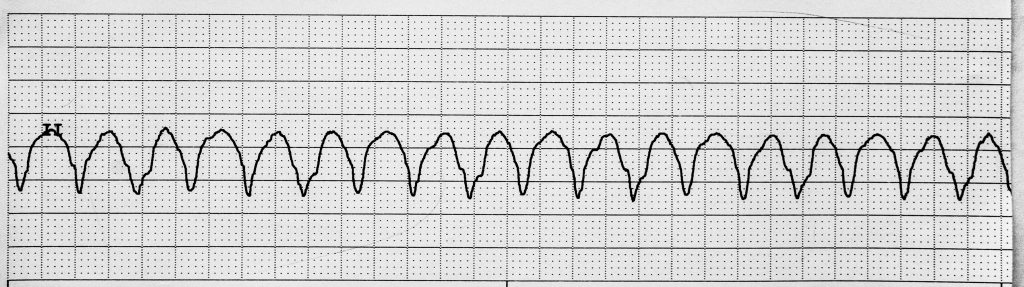
Torsades de pointes is a type of V-tach that occurs when there is a long QT interval, and a beat occurs during the QT interval. It resembles ventricular tachycardia but has a pattern of twisting points or peaks. This rhythm can rapidly develop into ventricular fibrillation and requires emergency response. See Figure 7.25[16] for an image of torsades de pointes.
Ventricular fibrillation is characterized by quivering ventricles with no patterns to the waveforms, so nothing can be measured on the ECG. As a result, there are no effective contractions and no cardiac output. This is the most dangerous arrhythmia because of lack of cardiac output and requires immediate initiation of CPR and emergency response. Defibrillation is administered, along with IV antidysrhythmic medications. Read details about defibrillation in the “Cardioversion and Defibrillation” section of this chapter. Read more information about antidysrhythmic medications in the “Antiarrhythmics” section of the “Cardiac and Renal” chapter of Open RN Nursing Pharmacology 2e. See Figure 7.26[17] for an image of ventricular fibrillation.
Some dysrhythmias, such as asystole and pulseless electrical activity, have no electrical conduction through the ventricles, resulting in no contractions and no pulse.
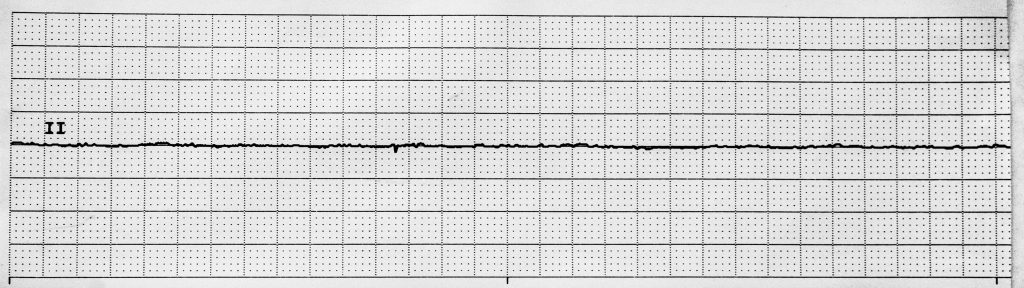
In asystole there are no electrical impulses, and a flat line appears on the ECG. CPR and emergency treatment are instituted, but asystole is not a shockable rhythm because there are no existing electrical impulses. See Figure 7.27[18] for an image of asystole.
Pulseless electrical activity (PEA) is similar to asystole because although electrical activity appears on the ECG, it is not strong enough to stimulate a ventricular contraction or a pulse. CPR and emergency treatment are initiated, but PEA is not a shockable rhythm.
Table 7.4c Characteristics of Common Ventricular Dysrhythmias, Asystole, and PEA
| Ventricular Rhythms | Pathophysiology | Causes | Identification | Symptoms | Nursing Interventions | Treatment | Patient Education |
|---|---|---|---|---|---|---|---|
| Premature Ventricular Contraction (PVC)[19] | Ectopic beats that originate in the ventricle. Common in healthy adults with no symptoms other than occasional palpitation. | Heart failure, high blood pressure, electrolyte imbalance, stress, alcohol, and excessive caffeine or energy drink consumption. | Wide bizarre QRS complexes within a normal underlying rhythm.
May be single or multiple PVCs. |
Palpitations and signs of decreased cardiac output depending on how frequent they are occurring. | Monitor for signs of decreased cardiac output. | If PVCs are infrequent or asymptomatic, no treatment is needed.
Treatment for symptomatic PVCs include correcting the underlying cause and may include ablation and antiarrhythmic medication. |
Educate about potential causes and lifestyle changes such as decreased caffeine and alcohol and improved stress management.
Seek medical care for signs of decreased cardiac output. |
| Supraventricular Tachycardia (SVT)[20] | The impulse to the ventricle is fast with ventricular rates often over 160 beats per minute. | Stress, caffeine, alcohol, infection, or sepsis. | Narrow-complex tachycardias with a QRS interval of 0.1 second or less. P waves cannot be identified due to the fast ventricular rate. | Chest pain, fast heartbeat, palpitations, shortness of breath, and syncope. | Prepare to administer medications to slow the heart rate. | Valsalva maneuvers and medications are used to slow the heart rate. | Seek medical care when the heart feels like it is racing or for symptoms of chest pain, shortness of breath, dizziness, confusion, or fainting. |
| Ventricular Tachycardia (V-tach[21] | Ventricular rate over 120 beats per minute, causing rapidly worsening cardiac output. | Coronary artery disease, heart failure, myocarditis, heart surgery, previous damage to the heart, recreational drugs, alcohol, medications, and electrolyte imbalances. | Wide QRS complexes are the only components that are measurable.
P and T waves are not visible. |
Chest pain, shortness of breath, syncope, palpitations, and cardiac arrest. Client can only tolerate this rhythm for a short period of time before losing consciousness. | Notify the provider and obtain emergency assistance.
Prepare to administer IV antidysrhythmic medications, cardioversion, or defibrillation. |
Reversible causes are treated.
If the client is stable, synchronized cardioversion and IV antidysrhythmic medications are administered. If the client is unstable, defibrillation and CPR are administered, along with IV antidysrhythmic medications. |
Call 911 for chest pain, shortness of breath, or fainting. |
| Torsades de Pointes[22] | A type of V-tach. | Long QT interval syndrome, certain congenital syndromes, and medications that can prolong the QT interval. | Resembles ventricular tachycardia but looks like twisting points or peaks.
Review the first beat to determine if it started in the QT interval. |
Chest pain, shortness of breath, syncope, palpitations, and cardiac arrest. Client can only tolerate this rhythm for a short period of time before losing consciousness. | Notify the provider and obtain emergency assistance. Be aware if the client is taking medications that prolong the QT interval.
Prepare to administer IV antidysrhythmic medications, cardioversion, or defibrillation.
|
Reversible causes are treated.
Synchronized cardioversion, IV magnesium, and/or IV antiarrhythmic medications are administered. An implantable cardiac defibrillator may be required. |
Seek medical care for feelings of the heart racing or palpitations. |
| Ventricular Fibrillation
(V-fib)[23] |
The ventricles are quivering with no effective contractions and no cardiac output.
This is the most dangerous arrhythmia. |
Heart disease, heart attack, heart surgery, untreated arrhythmias, electrolyte imbalances, and electrical shock. | Nothing can be measured because there is just a fibrillatory line.
Can be coarse or fine fibrillatory waves. Coarse waves are taller than fine. Fine V-fib is harder to treat and convert to a sustaining rhythm. |
Pulselessness and loss of consciousness. | Obtain emergency assistance and initiate CPR.
Prepare to administer IV antidysrhythmic medications and defibrillation. |
Reversible causes are treated. Defibrillation and IV antiarrhythmic medications administered according to ACLS algorithm. | Not applicable because the client is unconscious. |
| Asystole[24] | There are no electrical impulses occurring in the heart. | Shock, heart attack, untreated arrhythmia, trauma, and toxins. | A flat line appears on the ECG.
There is no impulse occurring, so nothing is measurable. |
Client is unconscious and does not have a pulse. | Initiate CPR and obtain emergency assistance.
Be aware systole is not a shockable rhythm. |
CPR and IV epinephrine are administered, and the underlying cause is treated. | Not applicable because the client is unconscious. |
| Pulseless Electrical Activity (PEA)[25] | There is electrical activity, but it is not strong enough to cause a contraction or a pulse. | Cardiac arrest, shock, untreated dysrhythmias, hypothermia, and trauma. | ECG components may be present, but the client does not have a pulse. | Client is unconscious and does not have a pulse. | Initiate CPR and obtain emergency assistance.
Be aware PEA is not a shockable rhythm. |
PEA is not a shockable rhythm. CPR and IV epinephrine are administered, and the underlying cause is treated. | Not applicable because the client is unconscious. |
Heart Block
A heart block is an obstruction in the normal pathway of electrical conduction through the heart that can occur in many anatomical locations. The anatomical location of a heart block can be categorized as in the sinus node, atrioventricular (A/V) node, or bundle branches.[26]
Sinus node blocks (also referred to as sinoatrial exit blocks) occur due to failed conduction of the impulses beyond the SA node, resulting in prolonger PR intervals or dropped P waves on the ECG. Common causes of sinus node blocks include sick sinus syndrome, increased vagal tone, inferior wall MI, vagal stimulation, myocarditis, and drugs (including digoxin and beta-blockers).[27]
Atrioventricular (AV) blocks are conduction blocks that can occur anywhere between the SA node and Purkinje fibers. There are three variants of AV blocks: first-degree, second-degree, and third-degree. Diagnosing AV blocks requires careful measuring of the PR interval and examining the relationship of the P waves to QRS complexes.[28] Certain medications, such as beta-blockers, can contribute to or worsen AV blocks and may need adjustments per the health care provider. First-degree, second-degree, third-degree, and bundle branch blocks are further described in the following subsections. Characteristics and treatments of common heart blocks are summarized in Table 7.4d at the end of this section.
First-Degree Heart Block
First-degree AV block is defined as a prolonged PR interval more than 0.2 seconds. A single P wave precedes every QRS complex by a consistent length. It may be a normal finding in some individuals. Conversely, it can be an early sign of degenerative disease of the conduction system or a transient manifestation of myocarditis, drug toxicity, hypokalemia, and acute rheumatic fever. It usually does not require any treatment.[29] See Figure 7.28[30] for an image of first-degree heart block.
Second-Degree Heart Block
There are two types of second-degree heart blocks: Type I and Type II.
Type I
Second-degree Type 1 AV block is also known as Wenckebach block. The block across the AV node or bundle of His is variable and increases with each ensuing impulse, ultimately resulting in a drop of the impulse. On an ECG, it shows a progressive prolongation of the PR interval, and then suddenly, a P wave is not followed by the QRS complex. This sequence regularly repeats itself. Most clients with Mobitz Type I second-degree AV block are asymptomatic. Mobitz Type I AV block may occur in the setting of acute myocardial ischemia or myocarditis. It may also result in clinical deterioration if the resulting ventricular rate is inadequate to maintain cardiac output. Most clients with Mobitz Type I second-degree AV block are asymptomatic and do not require specific intervention. Occasionally, clients with Mobitz Type I block are symptomatic, demonstrate hemodynamic instability, and require treatment with either atropine or cardiac pacing.[31]
Type II
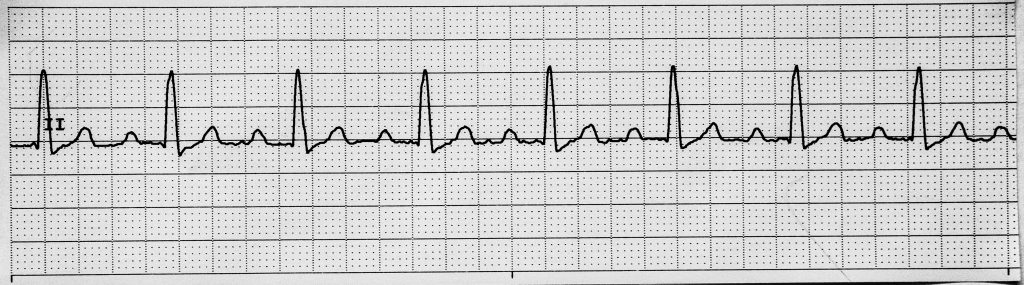
Second-degree Type 2 AV block has a consistent PR interval and the duration may be normal, but there are dropped ventricular beats, or QRS complexes, periodically. There can be one or more dropped QRS complexes, which can result in several P waves in a row without QRS complexes following them. This is significant because when ventricular beats are dropped, there is no ventricular output, meaning there is no cardiac output for the preceding P waves. It usually occurs below the AV node at the level of the bundle of His. It clinically signifies a severe underlying heart disease that can progress to third-degree heart block. When diagnosed, it usually requires prompt treatment with a permanent pacemaker.[32] See Figure 7.29[33] for an image of second-degree heart block, Type II.

Third-Degree Heart Block
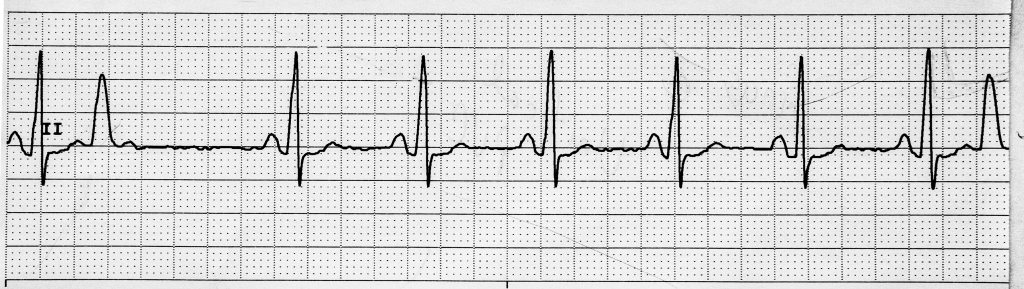
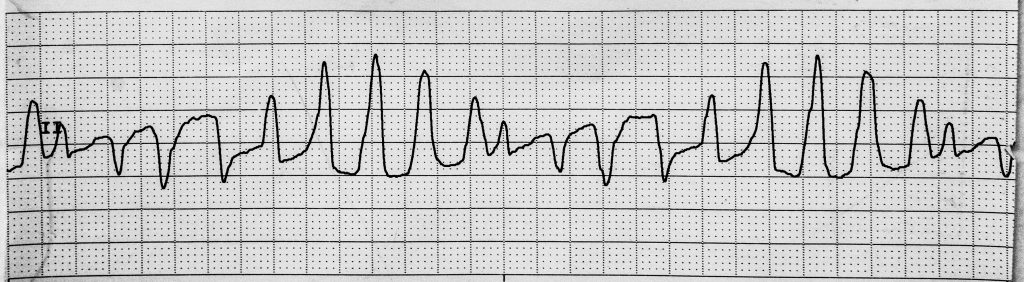
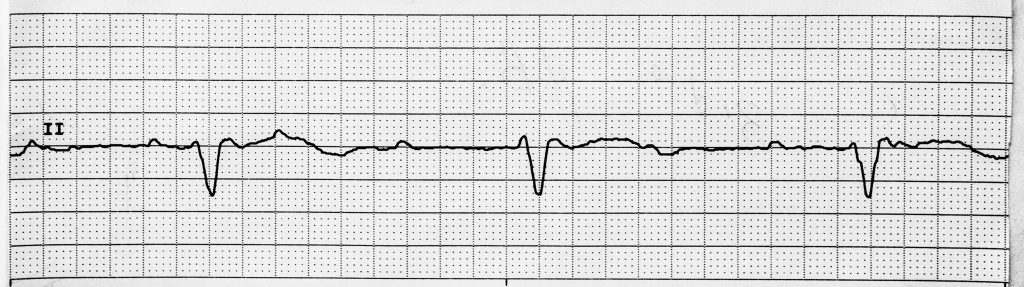
Third-degree AV block, also called complete heart block, is characterized by a complete electrical dissociation between the atria and ventricles, resulting in the atria and the ventricles beating at their intrinsic rates irrespective of how the other is beating. Degenerative disease of the conduction system is the leading cause of third-degree heart block. A complete heart block may present in acute myocardial infarction. Complete heart block may be reversible with prompt revascularization, especially in inferior myocardial infarction. Elevated magnesium levels can also cause third-degree heart block. Lyme disease may be associated with a complete heart block and is potentially reversible with antibiotic therapy. In the case of irreversible or permanent complete heart block, a permanent pacemaker remains the standard treatment.[34] See Figure 7.30[35] for an image of third-degree heart block.
Bundle Branch Blocks
Bundle branch blocks (i.e., intraventricular conduction delays) result from the conduction block of either left or right bundle branches and occur within the ventricles. They are diagnosed by examining the width and configuration of the QRS complexes.[36] A generic bundle branch block is characterized by a widened QRS complex greater than 0.12 mm. To determine if it is a right or left bundle branch block, additional 12-lead EKG interpretation is necessary and is beyond the scope of this text.
Table 7.4d Characteristics of Common AV Blocks
| AV Blocks | Pathophysiology | Causes | Identification | Symptoms | Nursing Interventions | Treatment | Patient Education |
|---|---|---|---|---|---|---|---|
| 1st-Degree AV Block | There is a slowed impulse from the AV node to the ventricles. | Heart attack, heart muscle disease, heart surgery, medications, toxins, and genetics. | The PR interval is greater than 0.20 seconds and consistent. There is one P wave for each QRS. | Typically, no symptoms. | Typically, none because asymptomatic. | Reverse underlying causes. | This is the least dangerous form of a heart block, but there is a chance it could progress to worse types of heart blocks. |
| 2nd-Degree Type 1 AV Block | The impulse from the AV node to the ventricles gets slower and slower with each beat until there is a dropped beat. The pattern then repeats itself. | Same as 1st-degree block. | The PR interval will become more prolonged with each beat until there is a missing beat. | Syncope, chest pain, shortness of breath, palpitations, shortness of breath, and nausea. | Treat the cause of the block if it is reversible.
Monitor for signs of worsening decreased cardiac output. |
Reverse underlying causes. If symptomatic, medications prescribed to improve cardiac output until a permanent pacemaker can be placed. | Be aware this type of block can progress to worsening blocks.
Seek medical treatment for chest pain, shortness of breath, dizziness, confusion, or fainting. |
| 2nd-Degree Type 2 AV Block | The impulse from the AV node to the ventricles is variable. Some beats will be normal, and other beats will be dropped. | Same as 1st-degree block. | PR interval is consistent. It may be normal or prolonged until the QRS is dropped, resulting in only P waves for those heartbeats. | Syncope, chest pain, shortness of breath, palpitations, shortness of breath, and nausea. | Treat the cause of the block if it is reversible.
Monitor for signs of worsening decreased cardiac output. |
Reverse underlying causes.
Symptomatic: Medications are prescribed to improve cardiac output until a permanent pacemaker can be placed. |
Be aware this type of block can progress to worsening blocks.
Seek medical treatment for chest pain, shortness of breath, dizziness, confusion, or fainting. |
| 3rd-Degree AV Block | The impulse from the AV node to the ventricles is blocked. The atria and ventricles beat independently of each other. | Same as 1st-degree block. | There is no correlation between the P and the QRS complex, but the P waves march out consistently and the QRS march out consistently.
The QRS complex is the only thing that is able to be measured. |
Syncope, chest pain, fatigue, and shortness of breath. | Client may have reduced cardiac output due to poor ventricular filling and slow heart rate.
Prepare the client for a pacemaker (temporary or permanent). |
Reverse underlying causes.
A temporary pacemaker may be initiated until a permanent pacemaker can be placed. |
Client will need a pacemaker. Be aware of pre-surgical treatment. |
Paced Rhythms
Clients with pacemakers have a set heart rate with unique characteristics on their ECGs referred to as paced rhythms. If their heart is atrial paced (A paced), a pacer spike appears before the P wave. If their heart is ventricular paced (V paced), a pacer spike appears before the QRS complex, and the QRS complex will be wide. If their heart is atrial-ventricular (AV) paced, there will be pacer spikes before the P wave and the QRS complex, and the QRS complex will be wide. See Figure 7.31[37] for an image of a ventricular-paced rhythm with pacer spikes appearing before the QRS complex. Characteristics of paced rhythms are summarized in Table 7.4e.

Table 7.4e Characteristics of Paced Rhythms
| Other Rhythms | Pathophysiology | Causes | Identification | Symptoms | Nursing Interventions | Treatment | Patient Education |
|---|---|---|---|---|---|---|---|
| Paced Rhythms[38] | A client who has a pacemaker will have a set rate. | Permanent pacemakers are placed for symptomatic bradycardia, heart blocks, or other dysrhythmias. | If it is atrial paced (A paced), there is a pacer spike before the P wave.
If it is ventricular paced (V paced), there is a pacer spike before the QRS complex. The QRS complex will be wide. If it is AV paced, there will be a pacer spike before the P wave and the QRS complex. The QRS complex will be wide. |
No symptoms as long as the pacemaker is working appropriately. | Interpret rhythm strip; report inappropriate pacing and pacing abnormalities to the provider. | None. | Take medications as prescribed; call the provider for symptoms such as unexplained edema, shortness of breath, dizziness, hiccups or muscle twitching, or signs of infection around the insertion site. Complete pacer checks as prescribed. |
ST Segment Abnormality
ST segment abnormality (elevation or depression) indicates myocardial ischemia or myocardial infarction and requires rapid emergency response. Discussion of medical treatment is beyond the scope of this text, but nurses should recognize ST abnormalities on ECGs and seek immediate emergency assistance. See Figure 7.32[39] for an image of ST elevation.
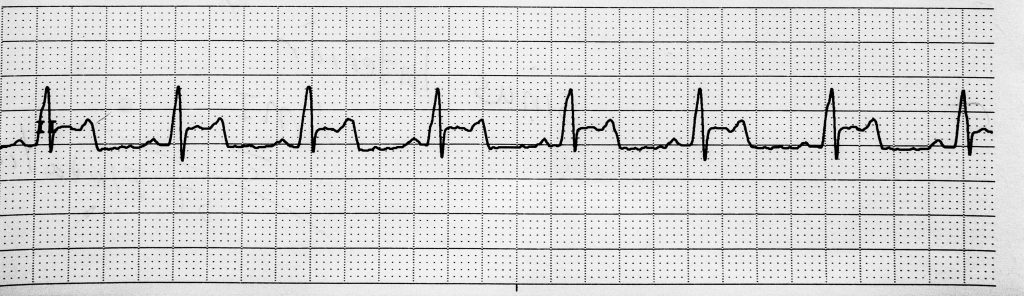
- “Normal Sinus Rhythm” by Deanna Hoyord is licensed under CC BY 4.0 ↵
- “Sinus Tachycardia.jpg” by Deanna Hoyord is licensed under CC BY 4.0 ↵
- “Sinus Bradycardia” by Deanna Hoyord is licensed under CC BY 4.0 ↵
- Cleveland Clinic. (2022, March 7). Sinus bradycardia. https://my.clevelandclinic.org/health/diseases/22473-sinus-bradycardia ↵
- Cleveland Clinic. (2022, October 3). Tachycardia. https://my.clevelandclinic.org/health/diseases/22108-tachycardia ↵
- Cleveland Clinic. (2022, March 21). Sinus arrhythmia. http://my.clevelandclinic.org/health/diseases/21666-sinus-arrhythmia ↵
- “Atrial Fibrillation” by Deanna Hoyord is licensed under CC BY 4.0 ↵
- “Atrial Flutter” by Deanna Hoyord is licensed under CC BY 4.0 ↵
- Cleveland Clinic. (2021, July 27). Premature atrial contractions. https://my.clevelandclinic.org/health/diseases/21700-premature-atrial-contractions ↵
- Cleveland Clinic. (2022, May 1). Atrial fibrillation (Afib). https://my.clevelandclinic.org/health/diseases/16765-atrial-fibrillation-afib ↵
- Cleveland Clinic. (2022, September 21). Atrial flutter. https://my.clevelandclinic.org/health/diseases/22885-atrial-flutter ↵
- “Sinus Rhythm with Unifocal PVCs” by Deanna Hoyord is licensed under CC BY 4.0 ↵
- “Bigeminy PVCs” by Deanna Hoyord is licensed under CC BY 4.0 ↵
- “Supraventricular Tachycardia” by Deanna Hoyord is licensed under CC BY 4.0 ↵
- “Ventricular Tachycardia” by Deanna Hoyord is licensed under CC BY 4.0 ↵
- “Torsades de Pointes” by Deanna Hoyord is licensed under CC BY 4.0 ↵
- “Ventricular Fibrillation” by Deanna Hoyord is licensed under CC BY 4.0 ↵
- “Asystole” by Deanna Hoyord is licensed under CC BY 4.0 ↵
- Cleveland Clinic. (2022, July 29). Premature ventricular contractions. https://my.clevelandclinic.org/health/diseases/17381-premature-ventricular-contractions ↵
- Cleveland Clinic. (2021, December 1). SVT (supraventricular tachycardia). https://my.clevelandclinic.org/health/diseases/22152-svt-supraventricular-tachycardia ↵
- Cleveland Clinic. (2022, June 12). Ventricular tachycardia. https://my.clevelandclinic.org/health/diseases/17616-ventricular-tachycardia ↵
- Cleveland Clinic. (2021, August 13). Torsades de pointes. https://my.clevelandclinic.org/health/diseases/21915-torsades-de-pointes ↵
- Cleveland Clinic. (2021, September 20). Ventricular fibrillation. https://my.clevelandclinic.org/health/diseases/21878-ventricular-fibrillation ↵
- Cleveland Clinic. (2022, May 3). Asystole. https://my.clevelandclinic.org/health/symptoms/22920-asystole ↵
- Cleveland Clinic. (2022, June 3). Pulseless electrical activity. https://my.clevelandclinic.org/health/symptoms/23213-pulseless-electrical-activity ↵
- This work is a derivative of StatPearls by Sattar and Chhabra and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Sattar and Chhabra and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Sattar and Chhabra and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Sattar and Chhabra and is licensed under CC BY 4.0 ↵
- “1st Degree Heart Block” by Deanna Hoyord is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Sattar and Chhabra and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Sattar and Chhabra and is licensed under CC BY 4.0 ↵
- “2nd Degree Type II AV Block.jpg” by Deanna Hoyord is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Sattar and Chhabra and is licensed under CC BY 4.0 ↵
- “Third Degree Heart Block.jpg” by Deanna Hoyord is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Sattar and Chhabra and is licensed under CC BY 4.0 ↵
- “Ventricular Paced Rhythm” by Deanna Hoyord is licensed under CC BY 4.0 ↵
- Cleveland Clinic. (2022, February 28). Permanent pacemaker. https://my.clevelandclinic.org/health/symptoms/23213-pulseless-electrical-activity ↵
- “Sinus Inferior AMI with ST Elevation.jpg” by Deanna Hoyord is licensed under CC BY 4.0 ↵
Decreased blood pressure and pulses, prolonged capillary refill, chest pain, shortness of breath, dizziness, confusion, or loss of consciousness.
Rhythms that originate from the sinus node and describe the characteristic rhythm of the healthy human heart.
Sinus rhythm faster than the normal range (i.e., greater than 100).
A sinus rhythm that is a slower rate than normal (i.e., less than 60).
Rhythm correlates to the respiratory cycle; the rate increases when the client breathes in and slows when they breathe out.
Rhythms that originate in the atria rather than in the SA node.
An ectopic beat that originates in the atria.
An irregular heart rhythm originating in the heart's upper chambers (atria) characterized by atrial quivering. This rhythm is often referred to as an “irregularly irregular rhythm.”
Fast, regular atrial impulses with rates between 250-300. As a result, the heart is not able to fill and pump the appropriate amount of blood with each beat. Clients are at increased risk for stroke.
Rhythms that originate in the ventricles (rather than the SA node) and cause the heart to beat faster.
Waveforms that look the same because the signal is originating from the same area in the heart.
Waveforms that look different because the impulse is originating from different areas of the heart.
Ectopic beats that originate in the ventricle.
A PVC every other beat.
A PVC that occurs every third beat.
PVCs occurring in pairs.
When a PVC occurs on the T wave.
The impulse to the ventricle is fast, and the impulse in the ventricle tries to keep up.
The ventricles are beating at a rate over 120 beats per minute, causing rapidly worsening cardiac output.
Occurs when there is a long QT interval, and the beat occurs during the QT interval.
The ventricles are quivering with no effective contractions and no cardiac output.
There are no electrical impulses occurring in the heart.
There is electrical activity, but it is not strong enough to cause contractions or a pulse.
An obstruction in the normal pathway of electrical conduction through the heart that can occur in many anatomical locations.
Failed conduction of the impulses beyond the SA node, resulting in prolonger PR intervals or dropped P waves on the ECG.
Conduction blocks that can occur anywhere between the SA node and Purkinje fibers.
There is a slowed impulse from the AV node to the ventricles.
The impulse from the AV node to the ventricles gets slower and slower with each beat until there is a dropped beat. The pattern then repeats itself.
The impulse from the AV node to the ventricles is variable. Some beats will be normal, and other beats will be dropped.
The impulse from the AV node to the ventricles is blocked. The atriums and ventricles beat independently of each other.
Conduction block of either left or right bundle branches and occur within the ventricles.
A client who has a pacemaker will have a set rate.

