6.2 Basic Concepts
Review of Anatomy and Physiology
The lungs sit to the left and right of the heart within a space called the thoracic cavity. The cavity is protected by the rib cage. A sheet of muscle called the diaphragm sits at the bottom of the thoracic cavity and separates it from the abdominal cavity. For this reason, the thoracic cavity is a closed space with its own intrathoracic pressure.[1]
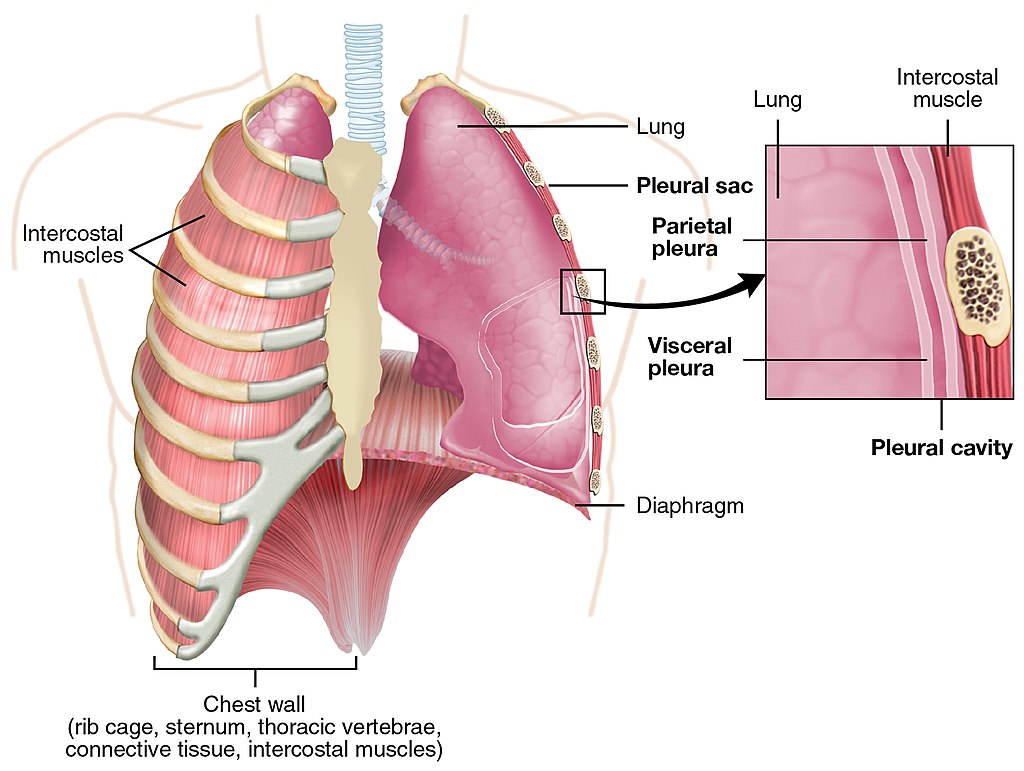
There are two membranes in the thoracic cavity. The visceral pleura membrane covers the outside of the lungs, and the parietal pleura membrane lines the interior chest wall. The space between these two membranes is called the pleural space (also referred to as the pleural cavity). The pleural space normally contains between 10 to 20 mL of pleural fluid that provides lubrication as the pleura continuously slide against each other during inspiration and expiration.[2] See Figure 6.1[3] for an illustration of the pleural cavity (i.e., pleural space).
The process of breathing, known as ventilation, is divided into two distinct phases called inspiration and expiration. During inspiration (also called inhalation), the diaphragm contracts and pulls downward while the intercostal muscles between the ribs pull upward. This movement increases the size of the thoracic cavity, thus decreasing the intrathoracic pressure. This change in pressure on inspiration is referred to as negative pressure. As a result, pressure is lower inside the thoracic cavity than atmospheric pressure, creating a vacuum effect that causes air to rush into the lungs on inspiration.[4]
During expiration (also called exhalation), the diaphragm relaxes, and the volume of the thoracic cavity decreases as the chest recoils. As a result, the intrathoracic pressure increases and becomes higher than atmospheric pressure, causing air to be forced out or the lungs.
View the following supplementary Medline Plus video[5] reviewing the physiology of breathing: Breathing
Pleural Disorders and Indications for Chest Tubes
An injury, inflammation, or infection can cause blood, fluid, or air to build up in the pleural space. The buildup of air or fluid can put pressure on the lung and cause all or part of it to collapse. Chest pain, shortness of breath, and coughing are common symptoms of pleural disorders, but the treatment for pleural disorders varies depending on the type of disorder and its seriousness. If left untreated, pleural disorders can lead to serious problems, including complete collapse of the lung, shock, or sepsis.[6]
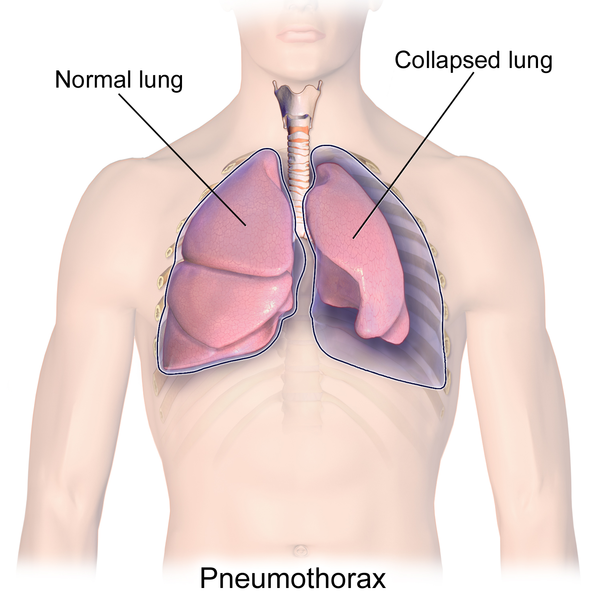
When a lung collapses due to leaked air into the pleural space, it is called a pneumothorax, and when it collapses due to blood in the pleural space, it is called a hemothorax.[7] See Figure 6.2[8] for an illustration of a pneumothorax.
There are different types of a pneumothorax: spontaneous pneumothorax, traumatic pneumothorax, and tension pneumothorax. A spontaneous pneumothorax can happen suddenly without any known cause. It can also be caused by medical conditions that affect the lungs, such as chronic obstructive pulmonary disease (COPD). A traumatic pneumothorax is caused by a chest injury, such as a bullet wound that pierces the pleural membranes, causing air to rush into the thoracic cavity.
Tension pneumothorax is a medical emergency caused by large pneumothorax that impacts cardiovascular functioning. The increasing thoracic pressure interferes with blood flow through the inferior vena cava, superior vena cava, and right chambers of the heart, causing the patient’s cardiac output and blood pressure to significantly drop. Due to increasing thoracic pressure, a tension pneumothorax causes the patient’s trachea to shift to the unaffected side.[9]
Other conditions that may require the placement of a chest tube include the following:
- Pleural effusion: Accumulation of fluid in the pleural space, often due to a medical condition such as cancer or heart, kidney, or liver failure
- Chylothorax: A collection of lymph in the pleural space
- Empyema: A pyogenic infection (pus) of the pleural space
- Hydrothorax: Accumulation of serous fluid in the pleural space
Chest tubes are indicated for these pleural disorders to remove air and/or fluid from the pleural space, reestablish negative pressure, and allow the lung to re-expand.
Chest Tube Placement Location
A chest tube is a sterile catheter that is inserted into the pleural space with small drainage holes at the proximal end of the tube to allow for drainage of air or fluid. See Figure 6.3[10] for an image of the proximal end of the chest tube that is inserted into the patient’s pleural space.

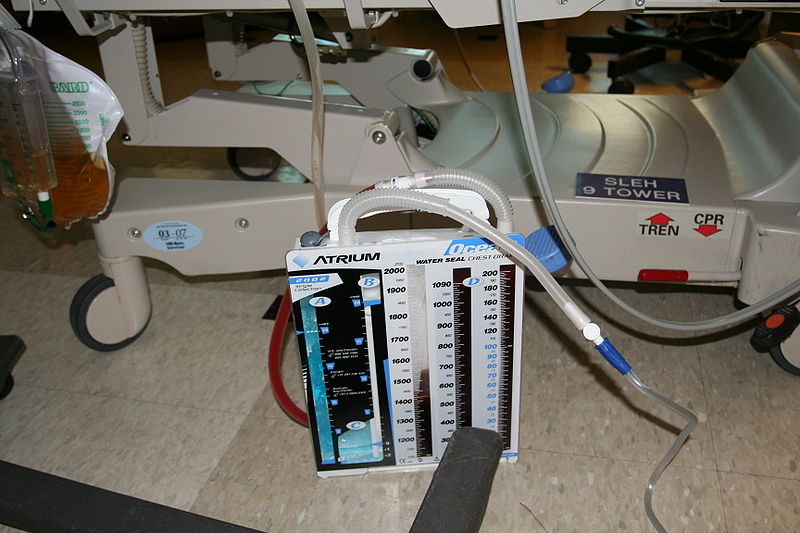
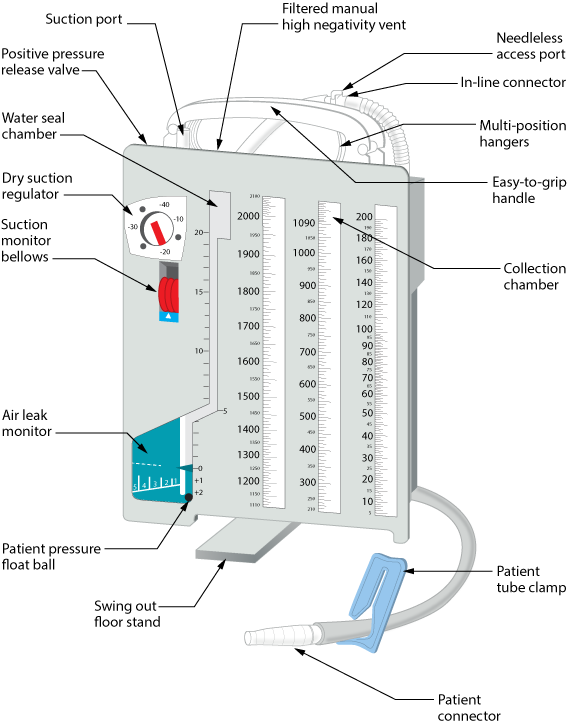
The distal end of the chest tube is connected to a closed drainage system. See Figure 6.4[11] for an image of a closed chest tube drainage system connected to a mannikin. The closed system drains air and fluid from the patient’s pleural space and prevents air or fluid from entering the pleural space. It is airtight and helps restore negative pressure in the thoracic cavity.[12] The chest tube drainage system must be maintained in an upright position below the patient’s chest to facilitate drainage. It should be placed on a non-movable surface or hung on the bed to prevent accidental dislodgment.

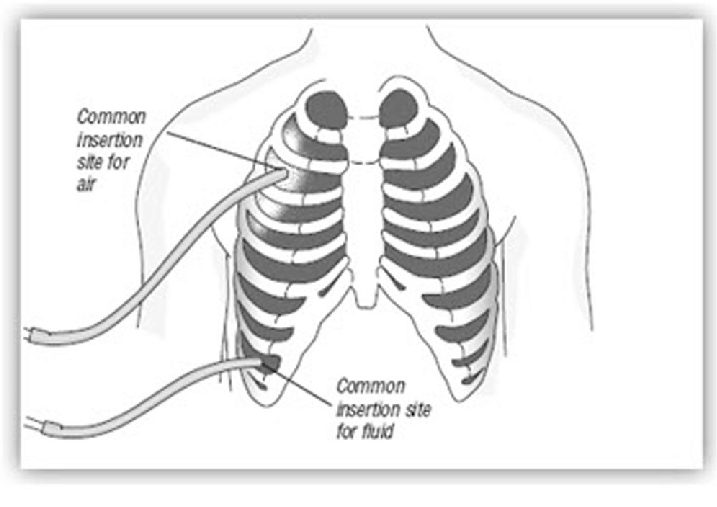
The location where the chest tube is inserted in the patient’s chest is based on the medical condition and the contents that need to be drained from the pleural space. For example, if a patient has a pneumothorax and air needs to be removed from the pleural space, the chest tube is placed higher within the thoracic cavity because air rises. It is typically placed in the second or third intercostal space of the anterior chest. As the air is removed from the patient’s pleural space, it disperses into the atmosphere, so there is little or no drainage collecting in the drainage system.[13]
Conversely, if fluid must be removed from the pleural space, it tends to settle in the lower portion of the lung cavity due to gravity. For this reason, chest tubes are often inserted in the lower posterior or lateral chest to drain blood and fluid. Suction is often applied to help promote the removal of the fluid. See Figure 6.5[14] for an illustration of common chest tube placement sites.
Chest tubes are also routinely placed postoperatively after cardiac surgery to eliminate mediastinal blood. They are typically placed through incisions near the inferior aspect of the sternotomy incision.
Chest Tube Drainage System Chambers
There is a wide range of chest tube drainage system models that have evolved over time with new technology. However, the basic design principles of these systems are the same: to prevent air from entering the pleural cavity during the various phases of the respiratory cycle and to allow for continuous drainage of air and/or fluid from the pleural cavity. To ensure successful and safe treatment of patients with chest tubes, nurses must have a good understanding of the functioning of the specific models of chest tube drainage systems used in their agency.[15] Always follow agency policy and manufacturer’s directions for setup, monitoring, and use.
In general, traditional chest tube drainage systems have three chambers[16]:
- Collection chamber: The chest tube exits the incision from the patient’s chest wall and connects directly to the collection chamber to collect drainage from the pleural space. The collection chamber is calibrated so that drainage can be directly measured in the device. The outer surface of the chamber has a surface that can be written on to document the date, time, and amount of fluid collected. This chamber is typically on the far right side of the system.[17]
- Water seal chamber: The water seal chamber has a one-way valve that allows air to exit the patient’s pleural cavity during exhalation but does not allow it to reenter during inhalation. The water seal chamber is filled with sterile water and maintained at the 2 cm mark to ensure proper operation. This level should be checked regularly and filled with additional sterile water as needed. The water in the water seal chamber may rise with inhalation and fall with exhalation (referred to as tidaling). Tidaling indicates the chest tube is patent. However, continuous bubbling in the water seal chamber may indicate an air leak. Some chest drainage systems have a feature that allows for measurements of air leaks. Read more about this feature later in this section.[18]
- Suction control chamber: Not all patients require suction. If a patient has suction ordered, the amount of suction should be prescribed by the provider. There are two types of suction systems that may be used, referred to as a wet suction system or a dry suction system.
- A wet suction system controls suction by the level of water in the suction control chamber and is typically set at -20 cm for adults. If there is less water in this chamber, there is less suction. There should be gentle bubbling in this chamber because it is directly attached to a suction device. However, excessive bubbling can cause rapid evaporation of the water. See Figure 6.6[19] for an image of a wet suction chest tube drainage system. In this image note the drainage in the collection chamber in the right compartment labeled “D,” the water seal chamber in the middle compartment labeled “C,” and -20 cm of water in the suction control chamber in the left compartment labeled “A.”
- A dry suction system uses a regulator to adjust the amount of suction and also responds to air leaks to deliver consistent suction for the patient.[20] See Figure 6.7[21] for an image of a dry suction chest tube system. Note the collection chamber on the right, the water seal chamber in the middle, and the dry suction regulator on the left.
Air Leak Monitor
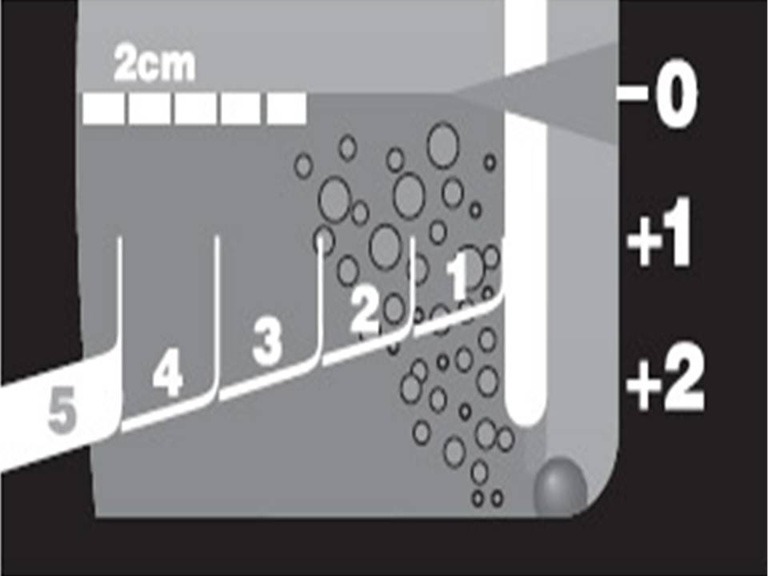
Chest tube drainage systems may include many safety features. For example, an air leak in the water seal chamber can indicate that air is reentering the patient’s pleural space, which can indicate worsening of a pneumothorax. Some chest tube drainage systems contain a feature in the water seal chamber that facilitates the measurement of the degree of an air leak from the chest cavity. See Figure 6.8[22] for an image of an air leak meter. The meter is made up of numbered columns, labeled from 1 (low) to 5 (high). The higher the numbered column through which bubbling occurs, the greater the degree of air leak. By documenting the numbered column through which bubbling is occurring, the nurse can monitor the increase or decrease of the air leak.
There are many different types and manufacturers of chest tube drainage systems. View a supplementary chest drain education video[23] by Gentinge that demonstrates the various components of their dry suction water seal chest drain: Express Dry Suction Dry Seal Chest Drain.
Heimlich Valve
A Heimlich valve is an alternative to a chest tube drainage system. It is a small, specially designed flutter valve that is portable and mobile, allowing a patient with a chest tube to ambulate with ease. The valve functions in any position, never needs to be clamped, and can be hooked up to suction if required. It can also be worn under clothing.[24] See Figure 6.9[25] for an image of a Heimlich valve.

The blue end of the Heimlich valve attaches to the chest tube inserted into the patient’s chest wall, and the other end can be left open to air or attached to a drainage bag. Air enters the inlet nozzle from the patient’s pleural space and opens a rubber sleeve inside the Heimlich valve. The sleeve collapses near the inlet nozzle, preventing the backflow of air into the patient, and then reopens at the outlet nozzle and allows air to escape.[26] See Figure 6.10[27] for a visual demonstration of how the Heimlich valve works.
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2022. Breathing; [updated 2021, February 12]. https://medlineplus.gov/ency/anatomyvideos/000018.htm#:~:text=The%20second%20phase%20is%20called,and%20air%20is%20forced%20out ↵
- Merkle, A. (2022). Care of a chest tube. StatPearls. https://www.statpearls.com/ArticleLibrary/viewarticle/41781 ↵
- “2313_The_Lung_Pleurea.jpg” by OpenStax College is licensed under CC BY 3.0 ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2022. Breathing; [updated 2021, February 12]. https://medlineplus.gov/ency/anatomyvideos/000018.htm#:~:text=The%20second%20phase%20is%20called,and%20air%20is%20forced%20out ↵
- A.D.A.M. Inc. (2021, February 2). Breathing [Video]. Medline Plus. All rights reserved. https://medlineplus.gov/ency/anatomyvideos/000018.htm#:~:text=The%20second%20phase%20is%20called,and%20air%20is%20forced%20out ↵
- National Heart, Lung, and Blood Institute. (2022, March 24). What are pleural disorders? U.S. Department of Health & Human Services. https://www.nhlbi.nih.gov/health/pleural-disorders ↵
- National Heart, Lung, and Blood Institute. (2022, March 24). What are pleural disorders? U.S. Department of Health & Human Services. https://www.nhlbi.nih.gov/health/pleural-disorders ↵
- “Blausen_0742_Pneumothorax.png” by Blausen.com staff (2014) at Medical gallery of Blausen Medical 2014 is licensed under CC BY 3.0 ↵
- National Heart, Lung, and Blood Institute. (2022, March 24). What are pleural disorders? U.S. Department of Health & Human Services. https://www.nhlbi.nih.gov/health/pleural-disorders ↵
- “Chest_Tube_Drainage_Holes.jpg” by Bentplate84 is licensed under CC BY-SA 3.0 ↵
- “Book-pictures-2015-687-001.jpg” by British Columbia Institute of Technology (BCIT) is licensed under CC BY 4.0. Access for free at https://opentextbc.ca/clinicalskills/chapter/10-7-chest-drainage-systems/ ↵
- This work is a derivative of StatPearls by Ravi & McKnight and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Ravi & McKnight and is licensed under CC BY 4.0 ↵
- “Common-insertion-site-of-chest-tube-for-air-and-fluid” by unknown author is licensed under CC BY-NC-ND 4.0. Access for free at https://www.researchgate.net/figure/Common-insertion-site-of-chest-tube-for-air-and-fluid_fig2_279737006 ↵
- “Chest Drainage Systems in Use” by Zisis, et al. is licensed under CC BY-NC-ND 4.0 ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- “Chest_drain_-_bedside_with_fluids.jpg” by Johntex is licensed under CC BY-SA 3.0 ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- “Labelled_chest_tube_drainage_system.png” by British Columbia Institute of Technology (BCIT) is licensed under CC BY-SA 4.0 ↵
- “atm-03-03-43-f2.jpg” by Charalambos Zisis, et al. for Annuals of Translational Medicine is used under Fair Use. Access for free at 10.3978/j.issn.2305-5839.2015.02.09 ↵
- Gentinge. (n.d.) Express dry suction dry seal chest drain [Video]. Getinge. All rights reserved. https://www2.getinge.com/us/education/chest-drain-education/# ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- “Book-pictures-2015-688.jpg” by unknown author is licensed under CC BY 4.0. Access for free at https://opentextbc.ca/clinicalskills/chapter/10-7-chest-drainage-systems/ ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- “Heimlich_valve.GIF” by Orinoco-w is licensed under CC BY-SA 3.0 ↵
The space between the visceral pleura and parietal pleura within the thoracic cavity.
Change in pressure on inspiration.
A lung collapses due to leaked air into the pleural space.
Lung collapse due to blood, pus, or other fluid in the pleural space.
A lung collapse that can happen suddenly without any known cause.
A lung collapse caused by a chest injury, such as a bullet wound that pierces the pleural membranes, causing air to rush into the thoracic cavity.
A medical emergency caused by large pneumothorax that impacts cardiovascular functioning.
Accumulation of fluid in the pleural space, often due to a medical condition such as cancer or heart, kidney, or liver failure.
A collection of lymph in the pleural space.
A pyogenic infection (pus) of the pleural space.
Accumulation of serous fluid in the pleural space.
The water in the water seal chamber may rise with inhalation and fall with exhalation.

