7.5 Cardioversion and Defibrillation
As a nurse becomes familiar with the various types of heart rhythms, it is important to recognize that some rhythms will require immediate intervention and an attempt to restore normal electrical activity within the heart. Without prompt intervention for certain arrhythmias, the client is at risk for cardiac arrest. With any rhythm interpretation, the nurse is responsible for assessing rhythm, identifying the rhythm, and treating the rhythm in collaboration with the medical team.
The purpose of prompt rhythm identification and intervention is to reorganize the electrical conduction within the heart before significant damage can occur. In order to understand how the reorganization of electrical pathways occurs, it is important to recall the normal cardiac conduction pathways. The normal cardiac conduction pathway begins with an electrical impulse from the sinoatrial node (SA) located in the right atrium, to the atrial-ventricle node (AV) located between the atrium and ventricles, down the bundle of His branches located within the ventricular septum, to the Purkinje fibers that deliver the electrical impulses to the ventricular myocardium. As the impulses are transmitted through the ventricular myocardium, they activate the contractions of the right and left ventricles.
When a client is experiencing a serious dysrhythmia, the conduction of the electrical impuse has become altered and the SA node is no longer initiating the rhythm. Cardioversion and defibrillation are used to attempt to reset the heart’s normal electrical conduction pathway and put the SA node back in charge.
Cardioversion
Cardioversion involves the use of low-energy electrical shocks to resume the heart’s normal electrical rhythm. It is important to remember that cardioversion is only used for dysrhythmia in which the client has a pulse. The typical rhythms that require cardioversion are paroxysmal supraventricular tachycardia (PSVT), supraventricular or narrow complex tachycardia, rapid atrial fibrillation/flutter, torsades de pointes (with a pulse), and ventricular tachycardia (with a pulse). If the client is hemodynamically stable, a provider may first attempt to convert the rhythm with the use of medications. However, if the client is unstable, immediate cardioversion may be required.
When a client has a heart dysrhythmia but is hemodynamically stable, such as new onset atrial fibrillation or atrial flutter, cardioversion may be a scheduled procedure. In these cases, clients will typically have a transesophageal echocardiogram (TEE) prior to the cardioversion to assess for potential blood clots within the heart, particularly if the rhythm has persisted for greater than 48 hours or the time of rhythm onset is unknown. The TEE procedure involves the use of an ultrasound transducer inserted down into the client’s esophagus via endoscope to examine blood flow within the heart. If there is no sign of clot present, the provider can proceed to cardioversion. If a clot is present, the client may require anticoagulation or a different medical treatment to manage the arrhythmia.
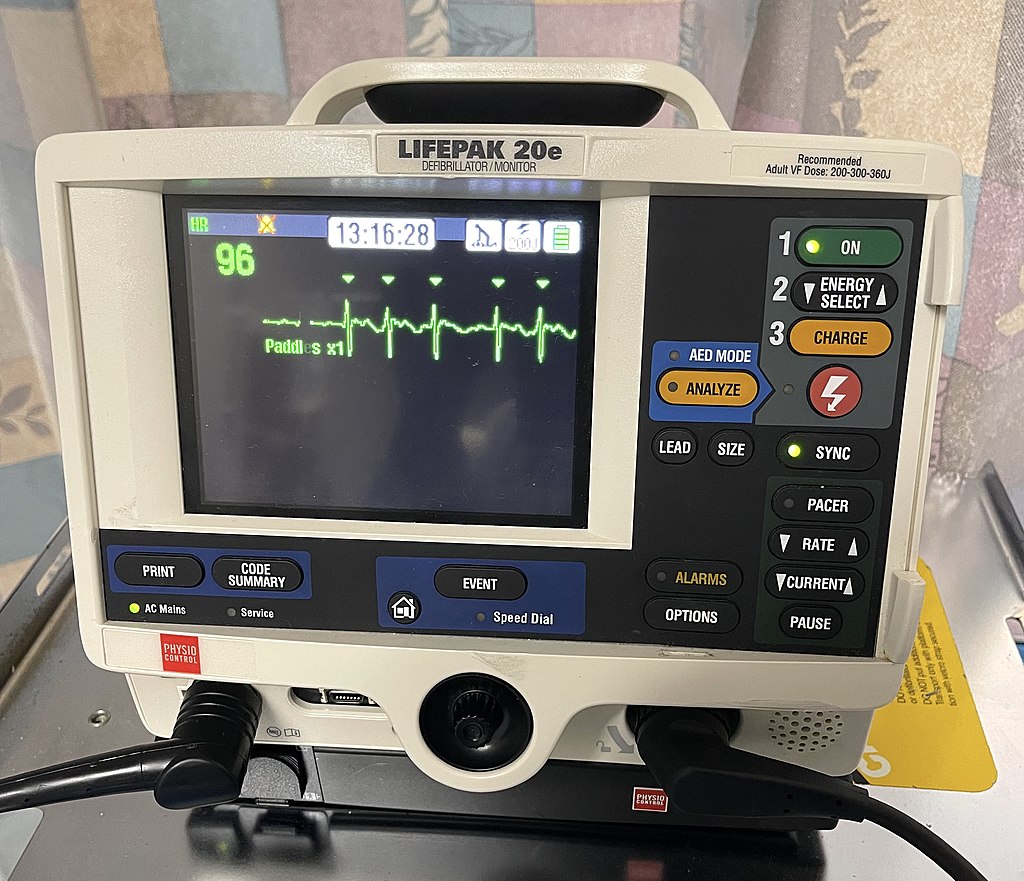
When preparing the client for cardioversion, electrode patches are placed on the chest in addition to the cardioversion pads. A cardiac monitor is used to monitor the heart rhythm then synchronizes the shock to the existing electrical activity within the client’s heart. When the monitor is “synced,” it identifies the client’s R waves and administers the electrical shock during the peak of the R wave. See Figure 7.33[1] for an image of a defibrillator monitor displaying triangles above the R waves of the client’s cardiac rhythm, which indicate the monitor has been synced. This synchronization ensures the shock is delivered at the appropriate time in the electrical cycle and minimizes the risk of developing ventricular fibrillation or asystole.
The majority of cardiac monitors, including automated external defibrillators (AEDs), are biphasic. Biphasic monitors deliver current to the client in two directions. In the first phase, current moves from one paddle to the other. In the second phase, it reverses direction.[2] The electrical energy levels are determined by the provider and may be as low as 100 to 200 joules. To maintain a safe environment, everyone must remain clear of the client when delivering the electrical shock. No one should touch the client, or the hospital bed, and oxygen equipment should be moved away from the client when the shock is delivered. Because the synced cardiac monitor will deliver the electrical shock at the optimal moment of the client’s existing cardiac electrical activity, there may be a few second delay from the time the shock is implemented to when it is actually delivered.
Defibrillation
Defibrillation is the immediate administration of an electrical current to help restore normal cardiac function. Defibrillation is administered when the client does not have a pulse. The typical rhythms for defibrillation are ventricular fibrillation, torsades de pointes (without a pulse), and ventricular tachycardia (without a pulse).[3] Automated external defibrillators (AEDs) search for these rhythms to determine if a client is experiencing a “shockable rhythm” that may be responsive to an electrical shock.
If a client has a dysrhythmia requiring defibrillation, the nurse must understand that blood is not circulating in the client. Therefore, in addition to the shock, the client requires cardiopulmonary resuscitation (CPR) to circulate blood throughout the body. Because these dysrhythmias are life-threatening and require emergency treatment, informed consent is not obtained. It is imperative for the client to receive the defibrillation shock as rapidly as possible, but high-quality compressions must be administered to maintain perfusion of vital organs until the defibrillator is connected to the client, the rhythm interpreted by the monitor, and shock is advised.
After the defibrillation monitor has arrived near the client, the pads must be placed on the client’s chest as quickly as possible to allow the monitor to analyze the rhythm. During the rhythm analysis process, is important that no one touches or moves the client. Once the monitor determines if a shock is advised, the staff should continue compressions until the monitor is charged and ready to administer shock at the required joules.
The goal of rapid defibrillation is to stop the disorganized rhythm promptly so the heart’s natural pacemaker can hopefully take over with an organized rhythm. Because disorganized rhythms use a tremendous amount of oxygen in already depleted heart tissue, continuing chest compressions for at least two minutes after defibrillation is required to reoxygenate the heart tissue and decrease the risk of the heart going back into ventricular tachycardia or ventricular defibrillation.
Defibrillation does not resolve asystole because an underlying electrical rhythm must be present. During asystole, the heart is in constant polarization and no electrical conduction is occurring.
- “LIFEPAK_20e_Defibrillator_and_Monitor_displaying_synchronization_with_QRS_complexes._(arrowheads).jpg” by StudentDoctorDG is licensed under CC BY-SA 4.0 ↵
- Li, W., Li, J., Wei, L., Wang, J., Peng, L., Wang, J., Yin, C., & Li, Y. (2021). A framework of current based defibrillation improves defibrillation efficacy of biphasic truncated exponential waveform in rabbits. Scientific Reports, 11(1), 1586-1586. https://doi.org/10.1038/s41598-020-80521-9 ↵
- Choi, H. J., & Noh, H. (2021). Successful defibrillation using double sequence defibrillation: Case reports. Medicine, 100(10), e24992-e24992. https://doi.org/10.1097/MD.0000000000024992 ↵
The use of low-energy shocks to resume the heart's normal electrical rhythm.
Delivery of electrical current to the patient in two directions.
The use of an electrical current administered immediately to a patient to help restore normal cardiac function.

