1.2 Basic Concepts of Venipuncture and Intravenous Therapy
Nurses access clients’ veins to collect blood (i.e., perform phlebotomy) and to administer intravenous (IV) therapy. This section will describe several methods for collecting blood, as well as review the basic concepts of IV therapy.
Blood Collection
Nurses collect blood samples from clients using several methods, including venipuncture, capillary blood sampling, and blood draws from venous access devices. Blood may also be drawn from arteries by specially trained professionals for certain laboratory testing.
Venipuncture
Venipuncture involves the process of introducing a needle into a client’s vein to collect a blood sample or insert an IV catheter. See Figure 1.1[1] for an image of venipuncture. Blood sampling with venipuncture may be initiated by a nurse, phlebotomist, or other trained personnel. Venipuncture for collection of a blood sample is an important part of data collection to assess a client’s health status. It is commonly performed to examine hematologic and immune issues such as the body’s oxygen carrying capacity, infection, and clotting function. It is also useful for assessing metabolic and nutrition issues such as electrolyte status and kidney functioning.
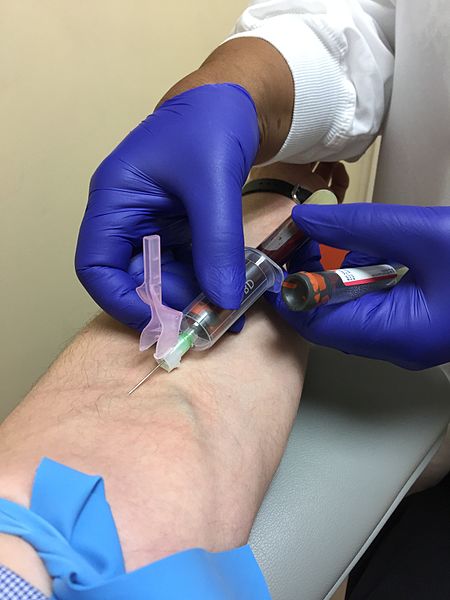
Blood collection is commonly performed via venipuncture from veins in the arms or hands. The most common sites for venipuncture are the large veins located on the antecubital fossa (i.e., the inner side of the elbow). These veins are often preferred for venipuncture because their larger size increases their ability to withstand repetitive blood sampling. However, these veins are not preferred for intravenous therapy due to the mechanical obstruction that can occur in the IV catheter when the elbow joint is contracted.
To perform the skill of venipuncture, the nurse performs many similar steps that occur with IV cannulation. The process of venipuncture for blood sample collection is outlined in the “Perform Venipuncture Blood Draw” checklist later in this chapter.
Blood Samples From Central Venous Access Devices
Blood may also be collected by nurses from a client’s existing central venous access device (CVAD). A CVAD is a type of vascular access that involves the insertion of a catheter into a large vein in the arm, neck, chest, or groin.[2] CVADs are discussed in more detail in the “Manage Central Lines” chapter that also contains the “Obtain a Blood Sample From a CVAD” checklist.
Capillary Blood Sampling
Nurses also collect small amounts of blood for testing via capillary blood sampling. Capillary blood testing occurs when blood is collected from capillaries located near the surface of the skin. Capillaries in the fingers are used for testing in adults whereas capillaries in the heels are used for infants. An example of capillary blood testing is bedside glucose testing. See Figure 1.2[3] for an image of capillary blood glucose testing.
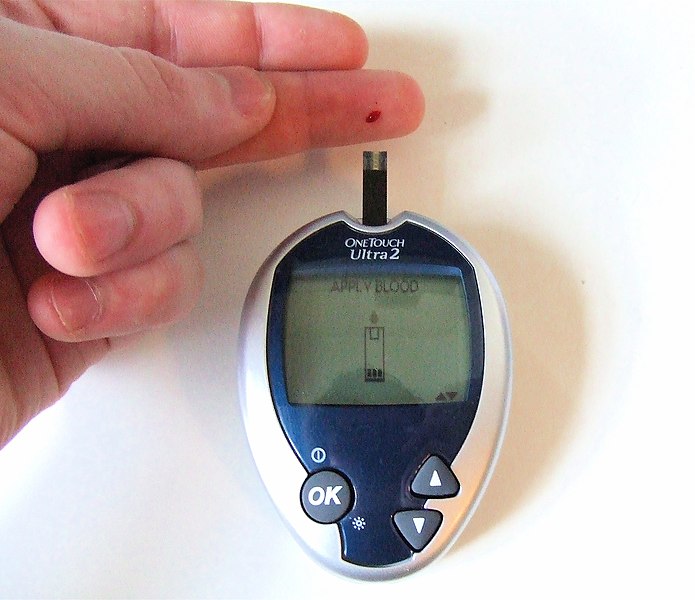
Capillary blood testing is typically used when repetitive sampling is needed. However, not all blood tests can be performed on capillary blood, and some clinical conditions make capillary blood testing inappropriate, such as when a client is hypotensive with limited venous return.
Review how to perform capillary blood glucose testing in the “Blood Glucose Monitoring” section of the “Specimen Collection” chapter of Open RN Nursing Skills.
Arterial Blood Sampling
Arterial blood sampling occurs when blood is obtained via puncture into an artery by specially trained registered nurses and other health care personnel, such as respiratory therapists, physicians, nurse practitioners, and physician assistants. Arterial blood collection is most commonly performed to assess the body’s acid-base balance in a diagnostic test called an arterial blood gas. (For more information on arterial blood gas interpretation, please review Open RN Nursing Fundamentals Chapter 15). The most common access site for arterial blood sampling is the radial artery. See Figure 1.3[4] for an image of arterial blood sampling. Arterial blood tests are known to be more painful for the patient than venipuncture and have a higher risk of complications such as bleeding and arterial occlusion with subsequent ischemia to the area distal to the puncture.
Arterial Lines
For clients who require repetitive arterial blood sampling or are hemodynamically unstable, an arterial line may be inserted by specially trained personnel. Arterial lines are specialized tubes that are inserted and maintained in an artery to assist with continuous blood pressure monitoring. They also allow for repeated blood sampling without repetitive puncture, thus decreasing the amount of discomfort for the client. The radial artery is the most common site used for arterial lines. Nurses must not confuse arterial lines with peripheral or central vein access devices. Arterial lines can be distinguished from venous lines by their specialized pressure tubing, which is firm and non-pliable and is connected to a pressure bag to maintain constant pressurized fluid in the tubing. Medications, fluid boluses, and maintenance IV fluids must never be infused through an arterial line. See Figure 1.3[5] for an image of arterial lines. The condition of the arterial access site, as well as perfusion of the client’s hand, is continually monitored when an arterial line is in place to prevent complications.

Intravenous Therapy
In addition to collecting blood samples, nurses also access clients’ veins to administer intravenous therapy.Intravenous therapy (IV therapy) involves the administration of substances such as fluids, electrolytes, blood products, nutrition, or medications directly into a client’s vein. The intravenous route is preferred to administer fluid and medications when rapid onset of the medication or fluid is needed. The direct administration of medication into the bloodstream allows for a more rapid onset of medication actions, restoration of hydration, and correction of nutritional deficits. IV therapy is often used to restore fluids and/or electrolyte balances more efficiently than what would be achieved via the oral route.
Fluid Balance
Fluid balance is an important part of optimal cellular functioning, and administration of fluids via the venous system provides an efficient way to quickly correct fluid imbalances. Additionally, many individuals who are physically unwell may not be able to tolerate fluids administered through their gastrointestinal tract, so IV administration is necessary.
When clients experience deficient fluid volume, intravenous (IV) fluids are often used to restore fluid to the intravascular compartment or to facilitate the movement of fluid between compartments through the process of osmosis. There are three types of IV fluids: isotonic, hypotonic, and hypertonic.[6]
Review movement of fluid between compartments of the body in the “Basic Fluid and Electrolyte Concepts” section of the “Fluids and Electrolytes” chapter in Open RN Nursing Fundamentals.
Isotonic Solutions
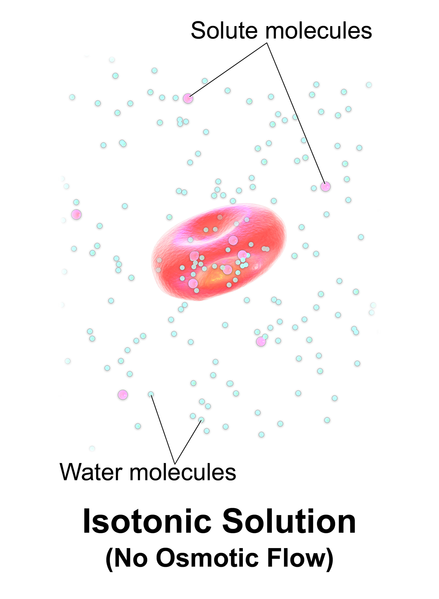
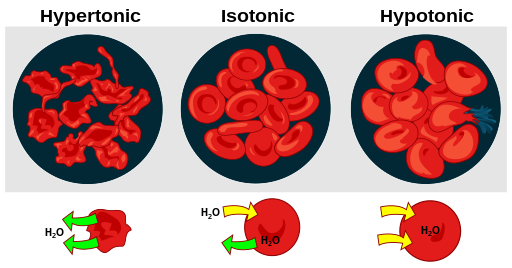
Isotonic solutions are IV fluids that have a similar concentration of dissolved solutes as found in the blood. Examples of isotonic IV solutions are 0.9% normal saline (0.9% NaCl) or lactated ringers (LR). Because the concentration of isotonic IV fluid is similar to the concentration of blood, the fluid stays in the intravascular space, and osmosis does not cause fluid movement between cells. See Figure 1.4[7] for an illustration of isotonic IV solution administration that does not cause osmotic movement of fluid. Isotonic solutions are typically used for patients with fluid volume deficit (also called hypovolemia) to raise their blood pressure. However, infusion of too much isotonic fluid can cause excessive fluid volume (also referred to as hypervolemia).[8]
Hypotonic Solutions
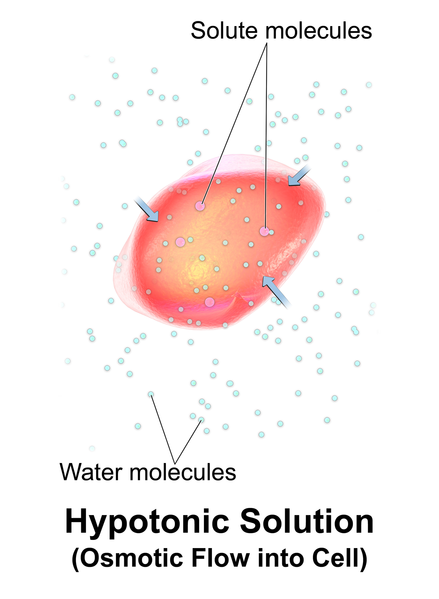
Hypotonic solutions have a lower concentration of dissolved solutes than blood. An example of a hypotonic IV solution is 0.45% normal saline (0.45% NaCl). When hypotonic IV solutions are infused, it results in a decreased concentration of dissolved solutes in the blood as compared to the intracellular space. This imbalance causes osmotic movement of water from the intravascular compartment into the intracellular space. For this reason, hypotonic fluids are used to treat cellular dehydration. See Figure 1.5[9] for an illustration of the osmotic movement of fluid into a cell when a hypotonic IV solution is administered, causing lower concentration of solutes (pink molecules) in the bloodstream compared to within the cell.[10]
However, if too much fluid moves out of the intravascular compartment into cells, cerebral edema can occur. It is also possible to cause worsening hypovolemia and hypotension if too much fluid moves out of the intravascular space and into the cells. Therefore, client status should be monitored carefully when hypotonic solutions are infused.[11]
Hypertonic Solutions
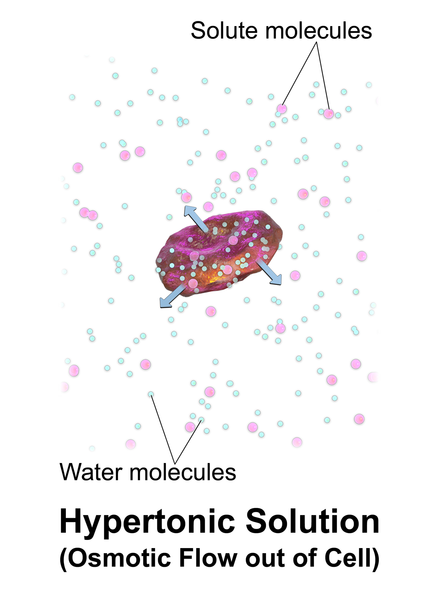
Hypertonic solutions have a higher concentration of dissolved solutes than blood. An example of hypertonic IV solution is 3% normal saline (3% NaCl). When infused, hypertonic fluids cause an increased concentration of dissolved solutes in the intravascular space compared to the cells. This causes the osmotic movement of water out of the cells and into the intravascular space to dilute the solutes in the blood. See Figure 1.6[12] for an illustration of osmotic movement of fluid out of a cell when hypertonic IV fluid is administered due to a higher concentration of solutes (pink molecules) in the bloodstream compared to the cell.
When administering hypertonic fluids, it is essential to monitor for signs of hypervolemia, such as breathing difficulties and elevated blood pressure. Additionally, if hypertonic solutions with sodium are given, the client’s serum sodium level should be closely monitored.[13]
See Figure 1.7[14] for an illustration comparing how different types of IV solutions affect red blood cell size.
IV fluids are considered medications. As with all medications, nurses must check the rights of medication administration according to agency policy before administering IV fluids. What began as five rights of medication administration has been extended to eight rights according to the American Nurses Association. These eight rights include the following[15]:
- Right Patient
- Right Medication
- Right Dose
- Right Time
- Right Route
- Right Documentation
- Right Reason
- Right Response
With any IV infusion, it is important for the nurse to pay close attention to the provider’s order and make sure that it contains the specific type of fluid, any additives or medications, amount to be infused, rate of infusion, and the length of time that the therapy should continue. The nurse should also carefully assess a client’s hydration status and oral intake to ensure that IV fluids are stopped appropriately as a client’s condition changes. For example, weight should be assessed daily for clients receiving IV fluids to monitor for fluid overload.
Review how to check the rights of medication administration in the “Administration of Enteral Medications” chapter of Open RN Nursing Skills.
Electrolyte Imbalance
In addition to rapidly improving hydration status, IV fluids may also be administered to rapidly correct electrolyte imbalances. Infusing fluids with electrolytes such as potassium, calcium, and magnesium can correct electrolyte imbalances more rapidly and effectively than by oral supplementation.
Electrolytes administered via the IV route must always be administered cautiously at the correct infusion rate because over supplementation can be deadly. For example, potassium infusions administered too rapidly into a client’s system can cause sudden cardiac arrest.
Blood Administration
Whole blood and blood components are administered by IV infusion. Blood is typically administered through larger-sized IV catheters. Read more information about blood administration in the “Administer Blood Products” chapter.
Nutrition
Nutritional therapy can be administered through an intravenous route for clients who do not have an adequately functioning gastrointestinal tract and/or are unable to take in food or fluids appropriately. Peripheral nutrition may be ordered through a peripheral IV site for nutritional needs such as albumin replacement.
Total parenteral nutrition (TPN) may be ordered for a client based on their specific electrolyte and/or nutritional needs. TPN is a very concentrated solution that must be administered via a central line. Central lines are placed in a larger vessel rather than a smaller, peripheral vessel. Accessing a central vessel requires additional training and expertise to prevent complications with insertion and is further discussed in the “Manage Central Lines” chapter. If a nurse receives an order for TPN therapy for a client who does not have central line access, the order should be clarified with the prescribing provider.
Medications
The IV route is preferred for the administration of many medications when immediate onset is required. For example, many types of pain medications can be given directly into the bloodstream with a much more rapid onset of action than if they were to be administered orally. Rapid relief of pain can be achieved in minutes rather than hours required for oral medications to reach their peak. Rapid onset can also be achieved with other medications such as those used to treat cardiac emergencies or severe allergic reactions to quickly restore clients to optimal body functioning. Additional information about IV administration of medications is discussed in the “Administer IV Push Medications” chapter. Additional information about administration of patient-controlled analgesia (PCA) is discussed in the “Specialized Infusions” section of this chapter.
IV Administration Equipment
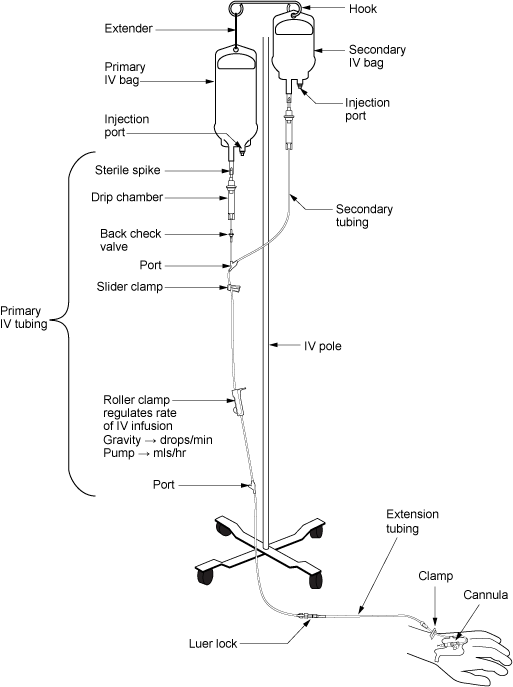
Intravenous (IV) substances are administered through flexible plastic tubing called an IV administration set. The IV administration set connects the bag of solution to the client’s IV access site. There are two major types of IV administration sets: primary administration sets and secondary administration sets. Administration sets require routine replacement to prevent infection. Follow agency policy regarding tubing changes before initiating a new bag of fluid or medications.
Primary Administration Sets
Primary administration sets can be used to infuse continuous or intermittent fluids, electrolytes, or medications. These substances may be administered by infusion pump or by gravity, and each method requires its own type of administration set.
Primary fluids are typically administered using an IV pump. An IV pump is the safest method of administration to ensure specific amounts of fluid are administered. The rate of infusion through an IV pump is typically calculated in mL/hour.
For infusion by gravity, a primary IV administration set can be a macro-drip or a micro-drip solution set. Macro-drip sets are used for routine primary infusions for adults. Micro-drip IV tubing is used in pediatric or neonatal care where small amounts of fluids are administered over a long period of time. A macro-drip infusion set delivers fluid at 10, 15, or 20 drops per milliliter, whereas a micro-drip infusion set delivers 60 drops per milliliter. The drop factor is located on the packaging of the IV tubing and is important to verify when calculating medication administration rates.
Primary IV administration sets consist of the following parts:
- Sterile spike: Used to spike the IV fluid bag and must be kept sterile.
- Roller clamp: Used to regulate the speed or stop an infusion by gravity.
- Drip chamber: This component allows air to escape from the IV fluid, preventing air from entering the client’s bloodstream. It should be kept one-quarter to one-half full of fluid. When using gravity to regulate the flow rate, the drops forming in the chamber are counted to set the rate in “drops per minute.”
- Backcheck valve: Prevents fluid or medication from travelling up into the primary IV bag.
- Access ports: Used to infuse secondary medications and to administer IV push medications. These may also be referred to as “Y ports.”
Secondary Administration Sets
Secondary IV sets are used to intermittently administer medications, such as antibiotics, while a primary IV infusion continues. The secondary tubing is shorter than primary tubing and connects to the primary line via an access port located above the infusion pump. To administer the secondary medication, the infusion pump is programmed to deliver the prescribed rate for the secondary infusion.
To ensure the secondary medication infuses first, the secondary bag is hung higher than the primary bag. This positioning uses gravity to pull fluid from the higher bag, allowing the secondary medication to infuse before the primary fluid resumes.
Secondary medications are often “piggybacked” into the primary line, using the primary fluid to prime the secondary tubing. To prime tubing, after connecting the secondary tubing to the primary line, lower the secondary bag below the level of the primary bag. This causes fluid from the primary line to flow backward into the secondary tubing, removing air.
See Figure 1.8[16] for an illustration of the setup of primary and secondary administration sets for primary administration of fluids and secondary administration of medication by gravity. See Figure 1.9[17] for an image of an IV infusion pump.

Priming IV Tubing
Primary administration sets, secondary administration sets, and extension tubing must be primed with IV solution to prevent air from entering the client’s circulatory system and causing an air embolism. Priming refers to the process of filling the IV tubing with IV solution prior to attaching it to the client. Review steps for setting up and priming primary and secondary administration sets using the information in the following box.
Review checklists of steps for “Primary IV Solution Administration” and “Secondary IV Solution Administration” in the “IV Therapy Management” chapter of Open RN Nursing Skills.
Infection Control
Aseptic technique must be maintained throughout all IV therapy procedures, including initiation of IV access, preparing and maintaining IV equipment, administering IV fluids and medications, and discontinuing an IV system. Hand hygiene and strict aseptic technique must be performed when handling all IV equipment. These standards can be reviewed in the “Aseptic Technique” chapter in Open RN Nursing Skills. Additionally, if an IV catheter or IV administration set should become contaminated by contact with a nonsterile surface, it should be replaced with a new one to prevent introducing bacteria or other contaminants into the system.
Types of Venous Access
There are several types of venous access devices used to administer IV therapy that are categorized as peripheral devices or central devices. Venous access device selection is tailored to each client’s needs and to the type, duration, and frequency of infusion.
Peripheral Devices
Peripheral venous access devices are commonly used for short-term IV therapy in the hospital setting. A peripheral IV is an intravenous catheter inserted by percutaneous venipuncture into a peripheral vein and held in place with a sterile transparent dressing. The transparent dressing helps to keep the site sterile, prevents accidental dislodgement, and allows the nurse to visualize the insertion site through the dressing. A securement device may be added to prevent accidental dislodgement.
The client’s upper extremities (hands and arms) are the preferred sites for insertion. However, a potential limitation of using the hand veins is they are smaller than the cephalic, basilic, or brachial veins in the arm. If the client requires rapid infusions where a larger gauge IV is warranted, the larger veins in the upper arm should be considered.
Peripheral IVs are used for short-term infusions of fluids, medications, or blood. Peripheral IVs are easy to monitor and can be inserted at the bedside by nurses and other trained professionals. After IV access has been obtained, the hub of an intravenous catheter is attached to a short extension set or a primary IV administration set. Luer lock connectors on the extension tubing and/or administration sets permit syringes to be attached to administer medications or fluid flushes.
Saline lock is a short extension set that provides IV access without continuous fluid infusion. When not in use, it is flushed with saline per agency policy and clamped to maintain sterility and prevent blood from backing up into the tubing. See Figure 1.10[18] for an image of a saline lock.

If the client requires continuous infusion of IV fluids, the extension tubing from the IV catheter is connected to a primary IV administration set. The IV tubing can be run through an infusion pump to administer fluids or medications at a programmed rate of infusion (typically calculated in mL/hour) or via gravity by setting a drip rate with the roller clamp (typically calculated in drops/minute). Manufacturers list the drop factor on the IV packaging. To reduce the risk of errors when using gravity to infuse fluids, many healthcare agencies require infusion pumps to ensure the correct flow rate.
Contraindications to Peripheral IV Access Sites
Before inserting a peripheral IV, the client should be assessed for contraindications related to insertion sites in the upper extremities. For example, clients who have a history of lumpectomy or mastectomy, an arteriovenous fistula, or current lymphedema often have restrictions that prohibit venipuncture into the affected extremity.[19] Additionally, deep vein thrombosis (DVT), fractures, contractures, or extensive scarring may also prohibit the placement of a peripheral IV. Hospitalized patients may have signage or a bracelet stating “limb alert” to alert heath care professionals to these conditions.
Midline Peripheral Catheters
Midline peripheral catheters have a larger catheter (i.e., 16-18 gauge) that allow for rapid infusions. Insertion is ultrasound-guided and can be inserted by RNs with additional training or other trained professionals. Midline catheters are typically inserted into the basilic, cephalic, or brachial veins of the upper arm with the tip placed near the level of the axilla. They are much longer and inserted deeper than a peripheral IV, but do not extend into a central vessel, so are not considered a central line. Therefore, they have a lower risk of infection than central venous access. Any medication that can be administered through a peripheral line can be administered via a midline peripheral catheter. They can also be used for longer duration than traditional peripheral venous access, which is ideal for clients needing extended hospital stays or IV access. Based on agency policy, midline catheters may also be used for blood sample collection, thus limiting the number of venipunctures a client receives. Site care for a midline peripheral catheter is similar to a peripheral IV dressing change.[20],[21]
Central Venous Access Devices
A central venous access device (CVAD) is a type of vascular access that involves the insertion of a tube into a vein in the neck, chest, upper arm, or groin and threaded into a central vein (most commonly the internal jugular, subclavian, or femoral) and advanced until the tip of the catheter resides within the inferior vena cava, superior vena cava, or right atrium.[22] Only specially trained health professionals may insert central venous access devices, but nurses provide routine care of CVADs, including dressing changes. See Figure 1.11[23] for an image of a central line requiring a dressing change.
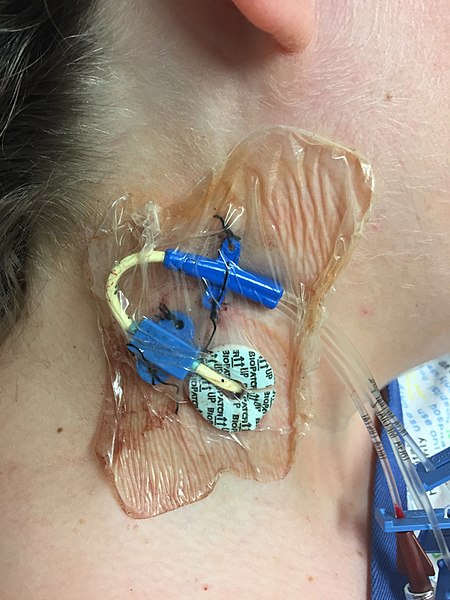
A central venous access device can be left in for longer periods of time and is useful for administering concentrated medications and fluids, such as TPN or hyperosmotic fluids, that would be otherwise irritating to smaller peripheral veins. However, central venous access devices have an increased risk for the development of bloodstream infections, so strict aseptic technique is required during insertion and maintenance. Central venous access devices are further discussed in the “Manage Central Lines” chapter.
Peripheral Inserted Central Catheters
A peripherally inserted central catheter (PICC) is a central venous access device inserted into a vein in the upper arm and threaded into the superior vena cava. It is used to give intravenous fluids, blood transfusions, chemotherapy, and other medications requiring a central line. It can also be used for blood sampling. A PICC may stay in place for weeks or months and helps avoid the need for repeated needlesticks. PICC lines are further discussed in the “Manage Central Lines” chapter.
General Guidelines for IV Therapy
The following are general guidelines for peripheral IV therapy[24]:
- IV fluid therapy is ordered by a provider. The order must include the type of solution or medication, total amount of fluid, rate of infusion, duration, date, and time.
- IV therapy is an invasive procedure. Significant complications can occur if the wrong amount of IV fluids or incorrect medication is given or if aseptic technique is not strictly followed.
- Nurses must understand the indications and duration for IV therapy for each client. Practice guidelines recommend that clients receiving IV therapy for more than six days should be assessed for an intermediate or long-term device such as a central venous access device (CVAD).
- Hospitalized patients may have an order for a small hourly infusion rate, such as 10-20 mL/hour, historically referred to in practice as a “to keep open” (TKO) or “keep vein open” (KVO) rate.
- IV administration sets require routine replacement to promote client safety and reduce the risk of infection. Primary and secondary continuous administration sets used to administer solutions other than lipids, blood, or blood products are typically changed every 96 hours, or up to every 7 days, as directed by agency policy and/or the manufacturer’s instructions. Administration sets should also be changed if contamination or compromise in the integrity of the product or system is suspected. Secondary administration sets that are detached from a primary administration set are typically changed every 24 hours or as directed by agency policy. Administration sets should be labelled according to agency policy with the date of initiation or the date of change indicated.[25]
- “Venipuncture_using_a_BD_Vacutainer.JPG” by MatthewLammers is licensed under CC BY-SA 4.0 ↵
- Centers for Disease Control and Prevention. (2025, June 12). Central line-associated bloodstream infection (CLABSI). https://www.cdc.gov/hai/bsi/bsi.html ↵
- “Blood_Glucose_Testing.JPG” by David-i98 is licensed under CC BY-SA 3.0 ↵
- American Nurses Association. (2021, April). Use of medication assistant/aides/technicians. ANA Issue Brief. https://www.nursingworld.org/~498e32/contentassets/a2ff1bd2d5ca467699c3bc764f7d9198/issue-brief-medication-aides-4-2021.docx ↵
- “Arterial line.jpg” by Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- This work is a derivative of Nursing Fundamentals by Open RN and is licensed under CC BY 4.0 ↵
- “Blausen_0685_OsmoticFlow_Isotonic.png” by BruceBlaus.com staff is licensed under CC BY 3.0 ↵
- This work is a derivative of Nursing Fundamentals by Open RN and is licensed under CC BY 4.0 ↵
- “Blausen_0684_OsmoticFlow_Hypotonic.png” by BruceBlaus.com staff is licensed under CC BY 3.0 ↵
- This work is a derivative of Nursing Fundamentals by Open RN and is licensed under CC BY 4.0 ↵
- This work is a derivative of Nursing Fundamentals by Open RN and is licensed under CC BY 4.0 ↵
- “Blausen_0683_OsmoticFlow_Hypertonic.png” by BruceBlaus.com staff is licensed under CC BY 3.0 ↵
- This work is a derivative of Nursing Fundamentals by Open RN and is licensed under CC BY 4.0 ↵
- “Osmotic pressure on blood cells diagram.svg” by LadyofHats is in the Public Domain. ↵
- American Nurses Association. (2021, April). Use of medication assistant/aides/technicians. ANA Issue Brief.https://www.nursingworld.org/practice-policy/medication-aides--assistants--technicians/contentassets/issue-brief-medication-aides-4-2021.docx ↵
- “intravenous_equipment_labels-2.png” by British Columbia Institute of Technology is licensed under CC BY 4.0. Access for free at https://opentextbc.ca/clinicalskills/chapter/8-2-types-of-iv-therapy/ ↵
- “DSC_0738-e1443533768679-678x1024.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0. Access for free at https://opentextbc.ca/clinicalskills/chapter/8-2-types-of-iv-therapy/ ↵
- “DSC_0896.jpg” by Glynda Rees Doyle and Jodie Anita McCutcheon is licensed under CC BY 4.0. Access for free at https://opentextbc.ca/clinicalskills/chapter/3-3-care-of-iv-tubing-administration-sets/ ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- Villalba-Nicolau, M., Chover-Sierra, E., Saus-Ortega, C., Ballestar-Tarín, M. L., Chover-Sierra, P., & Martínez-Sabater, A. (2022). Usefulness of midline catheters versus peripheral venous catheters in an inpatient unit: A pilot randomized clinical trial. Nursing Reports, 12(4), 814–823. https://doi.org/10.3390/nursrep12040079 ↵
- Nickel, B. (2021). Does the midline peripheral intravenous catheter have a place in critical care? Critical Care Nurse, 41(6), e1-e21. https://doi.org/10.4037/ccn2021818 ↵
- This work is a derivative of StatPearls by Kolikof, Peterson, and Baker and is licensed under CC BY 4.0 ↵
- “Central_Line_Sutures.jpg” by Red minx is licensed under CC BY-SA 4.0 ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- Gorski, L. A., Hadaway, L., Hagle, M. E., Broadhurst, D., Clare, S., Kleidon, T., Meyer, B. M., Nickel, B., Rowley, S., Sharp, E., & Alexander, M. A. (2021). Infusion therapy standards of practice. Journal of Infusion Nursing, 44(Suppl 1S), S1–S224. https://doi: 10.1097/NAN.0000000000000396.org ↵
The process of introducing a needle into a patient’s vein to collect a blood sample or insert an IV catheter.
A thin, flexible, large-bore tube inserted into a client’s large vein.
Blood sample collection from the capillary blood vessels, which are the tiny blood vessels located near the surface of the skin.
Blood sampling that occurs when blood is obtained via puncture into an artery.
The administration of a substance directly into a person’s vein.
IV fluids that have a similar concentration of dissolved solutes as found in the blood.
Solutions have a lower concentration of dissolved solutes than blood.
Solutions that have a higher concentration of dissolved solutes than blood.
A concentrated solution that is ordered for a patient based on their specific electrolyte and nutritional needs.
A short intravenous catheter inserted by percutaneous venipuncture into a peripheral vein and held in place with a sterile transparent dressing.
A short extension set that provides IV access without continuous fluid infusion.
A larger catheter (i.e., 16-18 gauge) inserted with ultrasound guidance into the basilic, cephalic, or brachial veins in the upper arm.
A type of vascular access that involves the insertion of a tube into a large vein in the neck, chest, or groin.
A central venous access device inserted into a vein in the upper arm and threaded into the superior vena cava.

