7.2 Basic Concepts
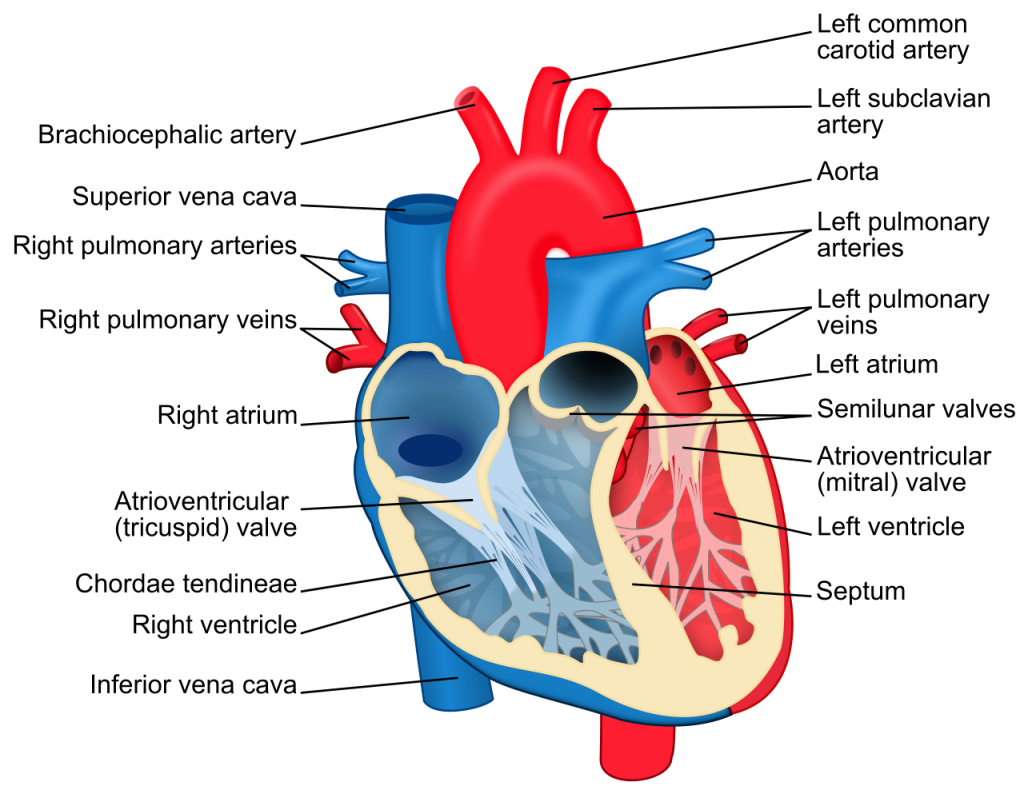
Before interpreting cardiac rhythms, it is vital to understand the anatomy and physiology of the heart. Let’s begin with a basic review of the cardiovascular system. The heart is a fist-sized organ that pumps blood throughout the body. It is the primary organ of the circulatory system. The heart contains four main chambers made of muscle and powered by electrical impulses. The brain and nervous system direct the heart’s function. The electrophysiology of the heart will determine the rate and rhythm. The blood pressure is maintained by the contractility of the heart muscle.[1] See Figure 7.1[2] for an illustration of the heart.
The parts of the heart are similar to the parts of a house. Both the heart and a house have the following components[3]:
- Walls
- Chambers (the rooms)
- Valves (the doors)
- Blood vessels (the plumbing)
- Electrical conduction system (the electricity)
Heart walls are muscles that contract (squeeze) and relax to send blood throughout the body. A layer of muscular tissue called the septum divides the heart walls into the left and right sides. Heart walls have three layers:
- Endocardium: The inner layer
- Myocardium: The muscular middle layer
- Epicardium: The protective outer layer (also known as the visceral pericardium)
The epicardium is one layer of the pericardium. The pericardium is a protective sac that covers the entire heart. It produces fluid to lubricate the heart and keeps it from rubbing against other organs.[4]
The heart is divided into four chambers. There are two chambers on the top (called the left and right atria) and two chambers on the bottom (called the left and right ventricles). Blood flows through the chambers of the heart in the following order:
- Right atrium: Two large veins called the superior vena cava and the inferior vena cava deliver oxygen-poor blood to the upper right chamber of the heart called the right atrium. The superior vena cava carries deoxygenated blood from the upper body. The inferior vena cava carries deoxygenated blood from the lower body. The right atrium pumps this blood through the tricuspid valve into the right ventricle.
- Right ventricle: This lower right chamber of the heart pumps the oxygen-poor blood through the pulmonary valves and then through the pulmonary arteries to the lungs. (Note that arteries usually carry oxygenated blood, but pulmonary arteries carry deoxygenated blood to the lungs.) The lungs reload blood with oxygen while removing carbon dioxide, and the pulmonary veins carry oxygenated blood back to the left atrium. (Note that veins usually carry deoxygenated blood, but pulmonary veins are the only veins in an adult that carry oxygenated blood.)
- Left atrium: The upper left chamber of the heart receives the oxygenated blood and pumps it through the mitral valve into the left ventricle.
- Left ventricle: The lower left chamber of the heart is called the left ventricle. It is slightly larger than the right ventricle because it pumps oxygen-rich blood through the aortic valve to the coronary arteries and out to the rest of the body.[5] See Figure 7.2[6] for an illustration of blood flow through the heart.
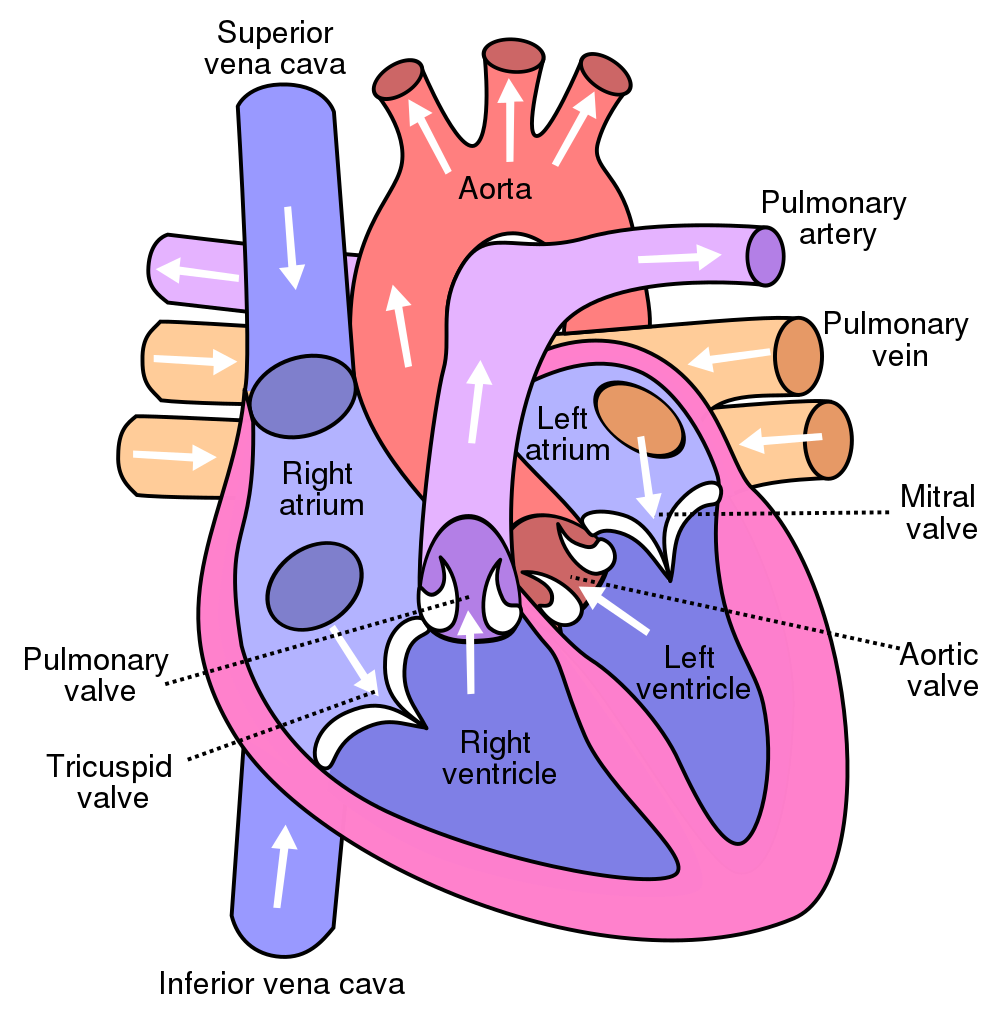
The heart valves are like doors between the four heart chambers that open and close to allow blood to flow through while preventing blood from moving backwards through the heart. The atrioventricular (AV) valves open between the atria and the ventricles (i.e., the upper and lower chambers of the heart). There are two AV valves[7]:
- Tricuspid valve: A three leaflet valve between the right atrium and right ventricle
- Mitral valve: A two leaflet (bicuspid) valve between the left atrium and left ventricle
Semilunar (SL) valves open when blood flows out of the ventricles. SL valves include the following[8]:
- Pulmonic valve: A three leaflet valve that opens when blood flows from the right ventricle into the pulmonary arteries (then to the lungs)
- Aortic valve: A three leaflet valve that opens when blood flows out of the left ventricle to the aorta
The heart pumps blood through three types of blood vessels called arteries, veins, and capillaries[9]:
- Arteries carry oxygen-rich blood from the heart to the body’s tissues. (As previously noted, the exception is the pulmonary arteries that carry deoxygenated blood to the lungs.) The aorta is a large artery that carries oxygen-rich blood from the heart to the rest of the body. The heart itself receives oxygen and nutrients through a network of coronary arteries that run along the heart’s surface.
- Veins carry oxygen-poor blood back to the heart. (As previously noted, the exception is the pulmonary veins that carry oxygenated blood from the lungs to the heart.)
- Capillaries are small blood vessels where the body exchanges oxygen and carbon dioxide in the blood at the cellular level.
View a supplementary YouTube video[10] on the anatomy and physiology of the heart in a virtual reality lab: Heart Anatomy and Flow by Dr. Nick Slamon.
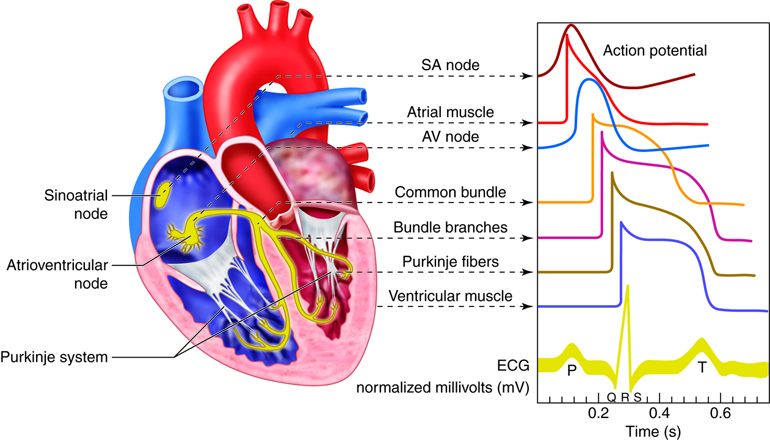
The electrical conduction system of the heart is similar to the electrical wiring of a house. The heart has a network of electrical bundles and fibers that control the rhythm and pace of the heartbeat. The electrical conduction system includes these components[11]:
- Sinoatrial (SA) node: The SA node is located in the upper part of the right atrium and is a major element of the conduction system. The SA node is often referred to as the heart’s natural pacemaker. The natural pacemaker rate for the SA node is 60-100 beats per minute. It sends the signals that make the heart beat with a normal rate and rhythm.
- Atrioventricular (AV) node: The AV node is located in the lower part of the right atrium. The AV node carries electrical signals from the SA node to the ventricles. If the SA node fails to send signals, the AV node takes over. The AV node is the “backup” pacemaker if the SA node fails. The AV node will pace the heart at a rate of 40-60 beats per minute.
- Bundle of His: A collection of cardiac cells found along the septum between the ventricles that sends electrical impulses from the AV node to the left and right bundle branches.
- Left bundle branch: Offshoots from the bundle of His that send electrical impulses to the left ventricle.
- Right bundle branch: Offshoots from the bundle of His that send electrical impulses to the right ventricle.
- Purkinje fibers: A network of thin filaments that carry electrical impulses that cause the ventricles to contract and pump blood out of the heart. If all other “backup” pacemakers in the heart fail, the Purkinje fibers will pace the heart at 20-40 beats per minute. See Figure 7.3[12] for an illustration of the electrical conduction system of the heart.
View the following YouTube video[13] explaining the electrical conduction system of the heart: Electrical Conduction System of the Heart: Cardiac SA Node, AV Node, Bundle of His.
Dysrhythmias
Occasionally, an area of the heart other than the SA node will initiate an impulse that will be followed by a premature contraction. Premature contractions simply mean these impulses happen too soon and may originate from a different place than a regular beat. These premature contractions can happen in the atrium (premature atrial contraction), ventricle (premature ventricular contraction), or AV junction (premature junctional contractions). Such a contraction is known as an ectopic beat, and the premature contraction causes an irregular heart rate and rhythm during that beat. The underlying heart rate and rhythm can be either regular or irregular. An ectopic focus may be stimulated by localized ischemia, exposure to certain drugs, abnormal electrolytes or acid-base balance, hypoxia, elevated stimulation by both sympathetic or parasympathetic divisions of the autonomic nervous system, or several diseases or pathological conditions. Occasional occurrences of dysrhythmias are generally transitory and not life-threatening. However, if the condition becomes a chronic deviation from the normal pattern of impulse conduction and contraction, it is referred to as dysrhythmia or arrhythmia. Severe arrhythmias can lead to cardiac arrest, which is fatal if not treated within a few minutes.
Electrocardiograms
Electrocardiograms (ECGs) use lead wires connected to electrodes attached to the client’s body to record the electrical activity of the heart on special graph paper or on a cardiac monitor. These electrodes detect the small electrical changes of cardiac muscle depolarization followed by repolarization during each cardiac cycle (heartbeat).
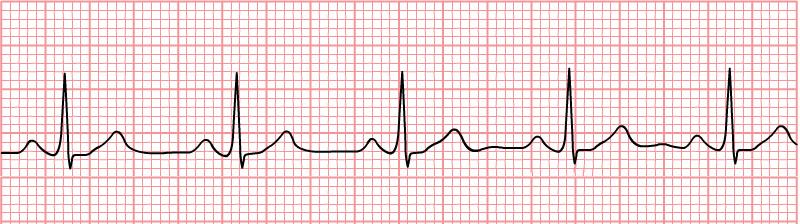
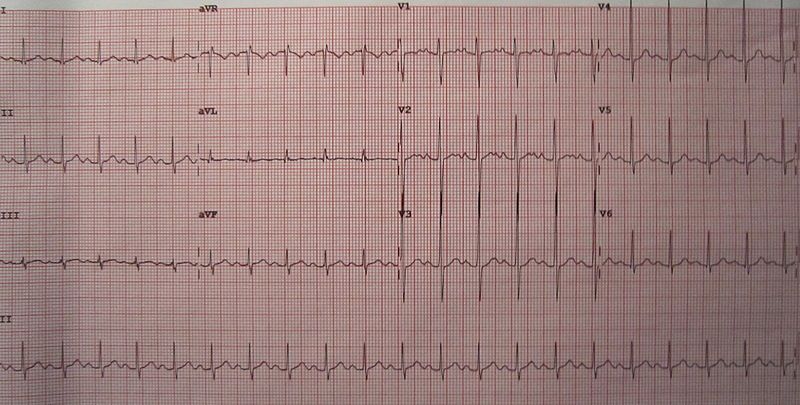
A paper rhythm strip is at least a 6-second tracing printed out on special graph paper that shows activity from one or two leads. See Figure 7.4[14] for an example of an ECG rhythm strip. When interpreting a paper ECG, the vertical lines indicate voltage of a given waveform. The thin lines, thick lines, and boxes along the horizontal axis represent various amounts of time as the electrical signal is conducted through the heart tissue:
- Thin lines or small box (1 mm intervals): 0.04 seconds
- Thick lines or big box (5 mm intervals): 0.2 seconds
12-Lead ECG
A 12-lead electrocardiogram is a diagnostic test that uses 12 leads to record information through 12 different perspectives of the heart to display a complete picture of its electrical activity. Electrodes are placed on the surface of the client’s chest (i.e., leads V1, V2, V3, V4, V5, and V6), and four are placed bilaterally on their upper and lower extremities (i.e., RA, LA, RL, LL). In this manner, the heart’s electrical activity is measured from twelve different angles (referred to as “leads”) to capture each moment throughout the cardiac cycle. Accurate placement of electrodes to obtain a 12-lead ECG is further described in “Checklist: Obtain a 12-Lead ECG.”
A standard 12-lead ECG report displays a 2.5 second tracing of each of the twelve leads. The tracings are most commonly arranged in a grid of four columns and three rows. The first column is the limb leads (I, II, and III), the second column is the augmented limb leads (aVR, aVL, and aVF), and the last two columns are the precordial leads (V1 to V6). See Figure 7.5[15] for an image of a 12-lead ECG with the various waveforms.
Each of the 12 ECG leads records the electrical activity of the heart from a different angle and, therefore, aligns with different anatomical areas of the heart:
- Inferior leads (II, III, and aVF): Inferior surface of the heart
- Lateral leads (I, aVL, V5, and V6): Lateral wall of the left ventricle
- Septal leads (V1 and V2): Septal surface of the heart
- Anterior leads (V3 and V4): Anterior wall of the right and left ventricles
When administered and interpreted accurately, an ECG can detect and monitor several types of heart conditions such as dysrhythmias, heart attacks (myocardial infarction), and electrolyte imbalances.
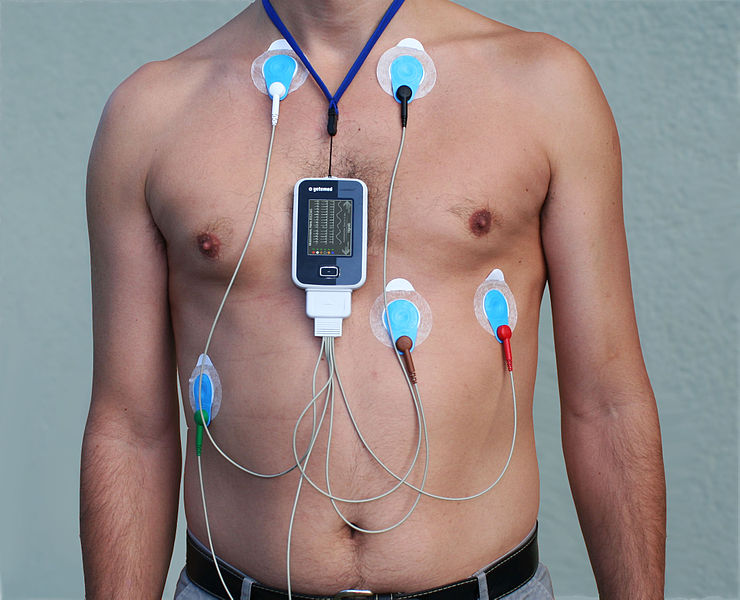
Telemetry
Telemetry refers to a portable device used to continuously monitor clients’ heart rhythms. While a client is on telemetry (also referred to as cardiac monitoring), their heart’s electrical patterns are displayed on a monitor. The patterns are continuously monitored by specially trained technicians and nurses who interpret the heart’s electrical activity. Nurses must be able to identify normal and abnormal heart rhythms displayed on a cardiac monitor. Health care agencies provide specialized training to nurses who work on units with clients on telemetry. See Figure 7.6[16] for an image of a client on telemetry.
Artifact
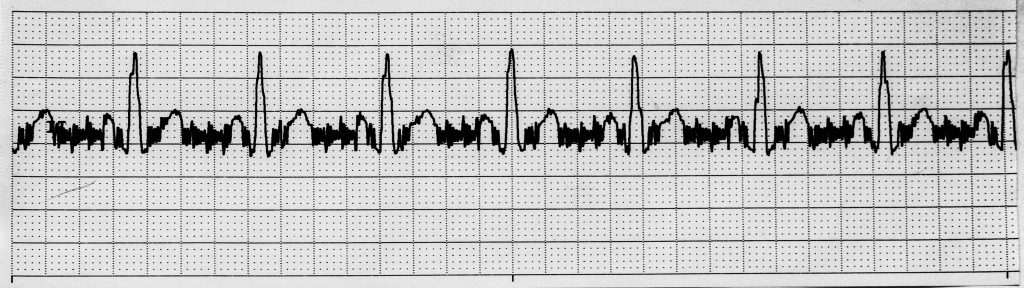
The monitor or ECG strip typically displays the name of the cardiac rhythm the client is experiencing, but this display is not always correct due to artifact. Artifact occurs when the electrodes are not making good contact with the skin and/or if the client moves during the tracing. See an image of artifact on an ECG strip in Figure 7.7[17]. Artifact may be interpreted by the monitor as ventricular beats or other abnormal cardiac patterns when, in reality, there are no cardiac abnormalities occurring. For this reason, it is important for nurses to observe the client to ensure what is displayed on the monitor is accurate according to the client’s condition.
Components of ECG Waveforms
There are five prominent components on an ECG waveform: the P wave; the Q, R, and S components (often referred to as the QRS complex); and the T wave. Each wave represents a specific electrical impulse in the heart with a specific appearance and normal ranges of measurements on the ECG graph paper. See Figure 7.8[18] for an image of these components.
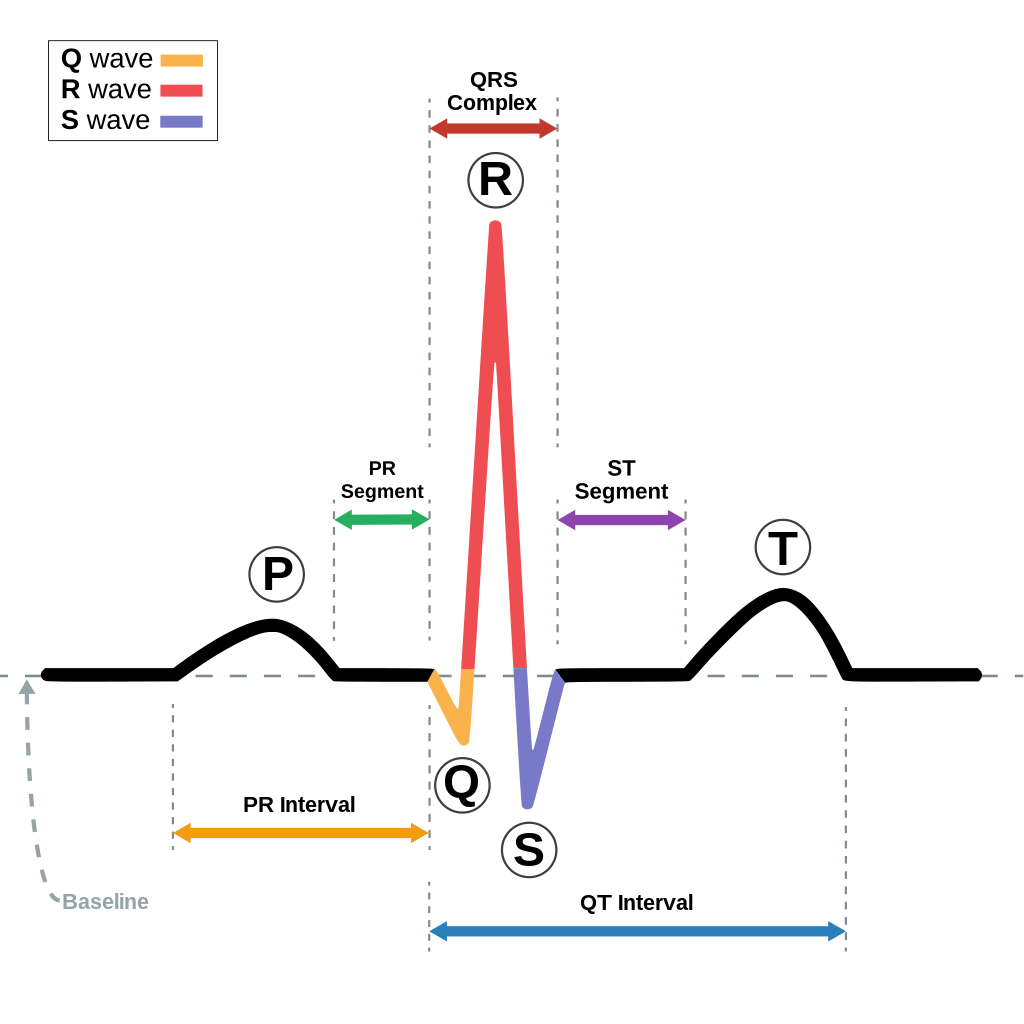
The small P wave represents the depolarization of the atria. The large QRS complex represents the depolarization of the ventricles, which requires a much stronger impulse because of the larger size of the ventricular cardiac muscle. The ventricles begin to contract as the QRS reaches the peak of the R wave, causing a “heartbeat” that is felt when assessing a client’s pulse. Lastly, the T wave represents the repolarization of the ventricle.[19]
Intervals between waveforms are assessed on an ECG. The P-P interval represents the duration between atrial heartbeats. The R-R interval represents the duration between the ventricular heartbeats. Both of these intervals should be consistent if the heart rhythm is regular. However, the P-P interval and the R-R interval may not be the same if a client has a dysrhythmia with different atrial and ventricular heart rates. For example, in atrial flutter the atrial rate will be much faster than the ventricular rate.
The isometric line (also known as isoelectric line) is used to measure intervals. It is an imaginary line that can be drawn horizontally through the telemetry strip. This is also called the baseline and is used to determine where each component of the heartbeat starts and ends. It also helps to determine if the component has a positive or negative deflection. See Figure 7.9[20] for an illustration of the isoelectric line.
The PR interval is measured from the start of the P wave to the start of the QRS complex. This is where the P wave starts to have a positive deflection off the isometric line to the first negative deflection. The QRS complex is measured from the first negative deflection (Q) through the upward spike (R) to the second negative deflection (S) once it returns to the isometric line. The QT interval is measured from the first negative deflection (Q) to the end of the T wave or where the T wave returns to the isometric line.
Table 7.2a reviews the characteristics of ECG components and intervals.
Table 7.2a Components and Intervals on an ECG Waveform
| Representation | Duration | Amplitude | Shape | Notes | |
|---|---|---|---|---|---|
| P wave | Atrial depolarization by the SA node | Less than 0.12 seconds | Less than 2.5 mm | Upward, rounded, and similar appearance | P wave may be inverted or biphasic (i.e., 2 phases) based on the lead being observed, but is typically upward and rounded. |
| PR interval | Conduction from the atria through the AV node into the ventricles | 0.12-0.20 seconds | Can be shortened or lengthened depending on heart rate. Lengthened past 0.2 seconds is referred to as a “heart block” dysrhythmia. | ||
| QRS complex | Atrial repolarization and relaxation and ventricular depolarization and contraction | 0.06-0.12 seconds | 1.0-3.0 mm | Q: Downward deflection
R: Upward spike; represents electrical stimulus passing through ventricles on depolarization S: Downward deflection; reflects final depolarization of Purkinje fibers |
All 3 waves may not be visible depending on which lead is being observed.
A Q wave duration greater than 0.04 seconds, depth greater than 1 mm, or size greater than 25% of the QRS complex amplitude is a sign of a previous myocardial infarction (commonly referred to as a pathological Q wave).
|
| QT interval | Ventricular depolarization and repolarization | 0.36-0.44 seconds | Normal QT interval varies based on gender and heart rate. It may be lengthened (bradycardia) or shortened (tachycardia) depending on heart rate. Corrected QT interval (QTc) is typically monitored because it takes heart rate and gender into consideration. A side effect of many medications is a prolonged QTc interval. | ||
| T wave | Ventricular repolarization | Less than 10 mm | Upward, rounded, and similar in appearance; should have a higher amplitude than P wave | Size should be between one eighth and two thirds of the size of the R wave.
|
|
| ST segment | Isoelectric period when the ventricles are in between depolarization and repolarization | 0.005 – 0.150 seconds | Less than 1 mm | Flat, isoelectric section of the ECG between the end of the S wave (often referred to as the J point) and the beginning of the T wave | Depressed ST segments may indicate coronary ischemia; ST elevation may indicate myocardial infarction. ST elevation is typically seen in leads V1 and V2. |
- Cleveland Clinic. (2021, August 26). Heart. https://my.clevelandclinic.org/health/body/21704-heart ↵
- “Heart_diagram-en.svg” by ZooFari is licensed under CC BY-SA 3.0 ↵
- Cleveland Clinic. (2021, August 26). Heart. https://my.clevelandclinic.org/health/body/21704-heart ↵
- Cleveland Clinic. (2021, August 26). Heart. https://my.clevelandclinic.org/health/body/21704-heart ↵
- Cleveland Clinic. (2021, August 26). Heart. https://my.clevelandclinic.org/health/body/21704-heart ↵
- “Diagram_of_the_human_heart.svg” by Wapcaplet, Yaddah is licensed under CC BY-SA 3.0 ↵
- Cleveland Clinic. (2021, August 26). Heart. https://my.clevelandclinic.org/health/body/21704-heart ↵
- Cleveland Clinic. (2021, August 26). Heart. https://my.clevelandclinic.org/health/body/21704-heart ↵
- Cleveland Clinic. (2021, August 26). Heart. https://my.clevelandclinic.org/health/body/21704-heart ↵
- Acadicus. (2021, January 21). Heart anatomy and flow by Dr. Nick Slamon [Video]. YouTube. All rights reserved. https://youtu.be/SE9MFFjJW8A ↵
- Cleveland Clinic. (2021, August 26). Heart. https://my.clevelandclinic.org/health/body/21704-heart ↵
- “C_M3_37.jpg” by CCCOnline is licensed under CC BY-SA 4.0. Access for free at https://pressbooks.ccconline.org/bio106/chapter/cardiovascular-levels-of-organization/ ↵
- RegisteredNurseRN. (2015, May 20). Electrical conduction system of the heart cardiac | SA node, AV node, bundle of His [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=-X9rYD8zSQg ↵
- “Normal_Sinus_Rhythm_Unlabeled.jpg” by Andrewmeyerson is licensed under CC BY-SA 3.0 ↵
- “Sinustachy.JPG” by James Heilman, MD is licensed under CC BY-SA 3.0 ↵
- “Alex_CM4000.jpg” by Misscurry is licensed under CC BY-SA 3.0 ↵
- “Sinus Rhythm with Artifact” by Deanna Hoyord is licensed under CC BY 4.0 ↵
- “SinusRhythmLabels.svg” by Agateller (Anthony Atkielski) is licensed in the Public Domain. ↵
- Physical Therapy Reviewer. (n.d.). How to read an ECG. https://ptreviewer.com/electrocardiogram-ecg-2/reading-an-ecg/ ↵
- “ECG deflection.gif” is a derivative of Tachycardia_ECG_paper.svg by Madhero88 and licensed under CC BY-SA 3.0. Access for free at http://simple-cardio.blogspot.com/2012/12/ecg-ekg-paper.html ↵
The inner layer of the heart.
The muscular middle layer of the heart.
The protective outer layer of the heart.
A protective sac that covers the entire heart. It produces fluid to lubricate the heart and keeps it from rubbing against other organs.
The upper right chamber of the heart.
A blood vessel that carries deoxygenated blood from the upper body.
The blood vessel that carries deoxygenated blood from the lower body.
Lower right chamber of the heart.
The blood vessels that carry deoxygenated blood to the lungs.
The blood vessels that carry oxygenated blood to the left atrium.
The upper left chamber of the heart.
The lower left chamber of the heart.
The valves that open between the atria and the ventricles.
A three leaflet valve between the right atrium and right ventricle.
A two leaflet (bicuspid) valve between the left atrium and left ventricle.
The valves that open when blood flows out of the ventricles.
A three leaflet valve that opens when blood flows from the right ventricle into the pulmonary arteries (then to the lungs).
A three leaflet valve that opens when blood flows out of the left ventricle to the aorta.
The blood vessels that carry oxygen-rich blood from the heart to the body’s tissues.
A large artery that carries oxygen-rich blood to the rest of the body.
A network of arteries that run along the heart’s surface.
The vessels that carry oxygen-poor blood back to the heart.
Small blood vessels where the body exchanges oxygen and carbon dioxide in the blood at the cellular level.
The node located in the upper part of the right atrium and is a major element of the conduction system.
The node that carries electrical signals from the SA node to the ventricles.
A collection of cardiac cells found along the septum between the ventricles that sends electrical impulses from the AV node to the left and right bundle branches.
Offshoots from the bundle of His that send electrical impulses to the left ventricle.
Offshoots from the bundle of His that send electrical impulses to the right ventricle.
A network of thin filaments that carry electrical impulses that cause the ventricles to contract and pump blood out of the heart.
A chronic deviation from the normal pattern of impulse conduction and contraction.
A chronic deviation from the normal pattern of impulse conduction and contraction.
Use lead wires connected to electrodes which are attached to the client’s body to record the electrical activity of the heart on special graph paper or on a cardiac monitor.
A diagnostic test that uses 12 leads to record information through 12 different perspectives of the heart to paint a complete picture of the electrical activity.
A portable device used to continuously monitor clients’ heart rhythms.
Displayed on the monitor when the electrodes are not making good contact with the skin and/or if the client moves during the tracing.
Duration between atrial heartbeats.
Duration between the ventricular heartbeats.
An imaginary line that can be drawn horizontally through the telemetry strip.

