13.5 Disorders of the Respiratory System
Disorders of the Respiratory System
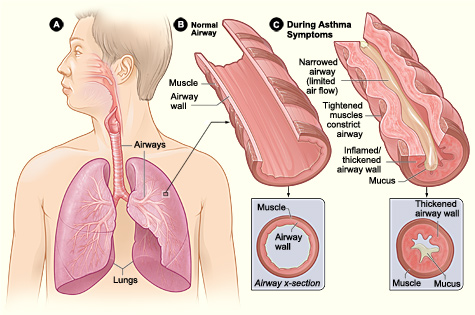
Asthma[1],[2]
Asthma is a common chronic respiratory disease characterized by episodes of bronchospasms (constriction of the bronchioles), inflammation, and edema of the airway that makes it difficult to exhale air, commonly referred to as an “asthma attack.” In addition, excessive mucus secretion further contributes to airway occlusion. Approximately 8.2 percent of adults (18.7 million) and 9.4 percent of children (7 million) in the United States have asthma. In addition, asthma is the most frequent cause of hospitalization in children.
An asthma attack can be triggered by a variety of environmental factors such as dust, pollen, pet hair, or dander, changes in the weather, mold, tobacco smoke, respiratory infections, or by exercise and stress. Cells of the immune system, such as eosinophils and mononuclear cells, may be involved in an allergic response that triggers the asthma attack. See Figure 13.18[3] for an illustration comparing a normal airway to an airway during asthma symptoms.
Symptoms of an asthma attack include shortness of breath, a whistling sound in the lungs called wheezing, chest tightness, and coughing. Severe asthma attacks are life-threatening and require emergency medical treatment. Symptoms of a severe asthma attack include worsening shortness of breath that results in cyanotic (blue) lips or face, confusion, drowsiness, a rapid pulse, sweating, and severe anxiety. The severity of the condition, frequency of attacks, and identified triggers influence the type of medications prescribed to manage the condition. Short-term, fast-acting medications are used to treat an asthma attack, and long-term medications are used to help prevent asthma attacks from occurring.
Read more information about asthma symptoms and treatments in the “Asthma” section of Open RN Health Alterations.
Atelectasis[4]
Atelectasis occurs when alveoli lose air and collapse. If left untreated, atelectasis can cause the collapse of part or all of a lung. Atelectasis is asymptomatic if only a few alveoli are affected, but as more alveoli become involved, the patient may report dyspnea, cough with or without sputum production, and pleuritic chest pain. Atelectasis is one of the most common breathing complications after surgery and can be prevented with adequate pain control, position changes, deep breathing and coughing, and walking soon after surgery.
Carbon Monoxide Poisoning[5]
Carbon monoxide poisoning occurs when carbon monoxide (CO) builds up in the blood and can lead to serious tissue damage or death. Carbon monoxide is a gas that has no odor, taste, or color and is produced from burning fuels such as gasoline, wood, propane, or charcoal. Appliances and engines that are not well-vented can cause carbon monoxide to build up to dangerous levels in the air. A tightly enclosed space makes the buildup worse. Carbon monoxide binds to hemoglobin with a much higher affinity than oxygen, displacing oxygen and reducing the blood’s oxygen-carrying capacity.
Carbon monoxide poisoning significantly affects the brain and heart. Symptoms of carbon monoxide poisoning include headache, weakness, dizziness, nausea or vomiting, shortness of breath, confusion, blurred vision, sleepiness, loss of muscle control, and loss of consciousness. Initial symptoms can be mistaken for flu symptoms without a fever. Individuals exposed to carbon monoxide should be moved to fresh air immediately and seek prompt medical attention.
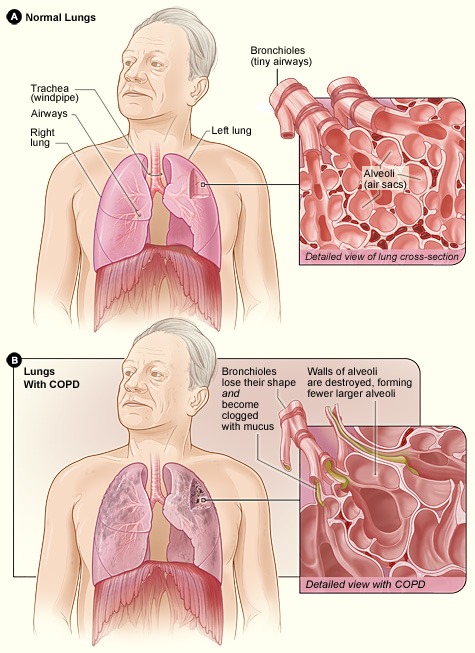
Chronic Obstructive Pulmonary Disease (COPD)[6],[7]
Chronic obstructive pulmonary disease (COPD) is a chronic, progressive lung disease caused by inflammation inside the airways resulting in limited airflow out of the lungs, known as obstruction. COPD is often caused by long-term exposure to irritating smoke, fumes, dust, or chemicals, with the most common cause being exposure to cigarette smoke. Unlike asthma with reversible, periodic episodes, COPD symptoms are continuous. Symptoms of COPD include shortness of breath, coughing, wheezing, and excessive mucus production. Symptoms may worsen during COPD exacerbations that are triggered by an illness or infection and typically require hospitalization.
Chronic obstructive pulmonary disease (COPD) is characterized by two main conditions: chronic bronchitis and emphysema. These two conditions may occur together and can vary in severity across individuals with COPD. Chronic bronchitis is inflammation of the lining of the bronchi, which leads to excessive mucus production. The inflammation prevents airflow into and out of the lungs. In emphysema, the alveoli are damaged and lose their elasticity, making it difficult to expel air out of the lungs and affecting gas exchange. The obstructions caused by chronic bronchitis and emphysema cause decreased levels of oxygen and elevated levels of carbon dioxide in the blood. See Figure 13.19[8] for an image comparing healthy lungs to lungs affected by COPD.
Although COPD is a condition that worsens over time, COPD symptoms are treatable with medications, supplementary oxygen administration, and other medical treatments. With proper management, many people with COPD can control symptoms and improve their quality of life.
Read more about COPD symptoms and management in the “COPD” section of Open RN Health Alterations.
Coronavirus (COVID-19)[9][10]
Coronavirus disease (COVID-19) is an infectious respiratory disease caused by the SARS-CoV-2 virus. Most people infected with the virus experience mild to moderate respiratory illness. However, some individuals become seriously ill and require urgent medical attention. Older adults and those with underlying medical conditions such as cardiovascular disease, diabetes, chronic respiratory disease, obesity, or cancer are more likely to develop serious illness.
The COVID-19 virus spreads from respiratory droplets and aerosols released from an infected person’s mouth or nose when they cough, sneeze, speak, sing, or breathe. These particles range from larger respiratory droplets to smaller aerosols, so respiratory etiquette is essential by covering your coughs and sneezes. Individuals infected with COVID-19 should also wash their hands or use an alcohol-based hand sanitizer frequently and stay home until they are recovered. Wearing a mask can also help prevent transmission of the virus. The best way to prevent COVID-19 is to be well-informed about how the virus spreads and stay up-to-date with CDC-recommended vaccinations.
Cystic Fibrosis[11]
Cystic fibrosis (CF) is a genetic condition that alters a protein in the body involved in the function of the cells, tissues, and glands responsible for producing mucus and sweat. Normal mucus is slippery and protects the airways, digestive tract, and other organs and tissues. Cystic fibrosis causes mucus to become thick and sticky. As mucus builds up, it can cause blockages, damage, or infections in affected organs. See Figure 13.20[12] for a depiction of signs and symptoms that may occur in patients with CF.
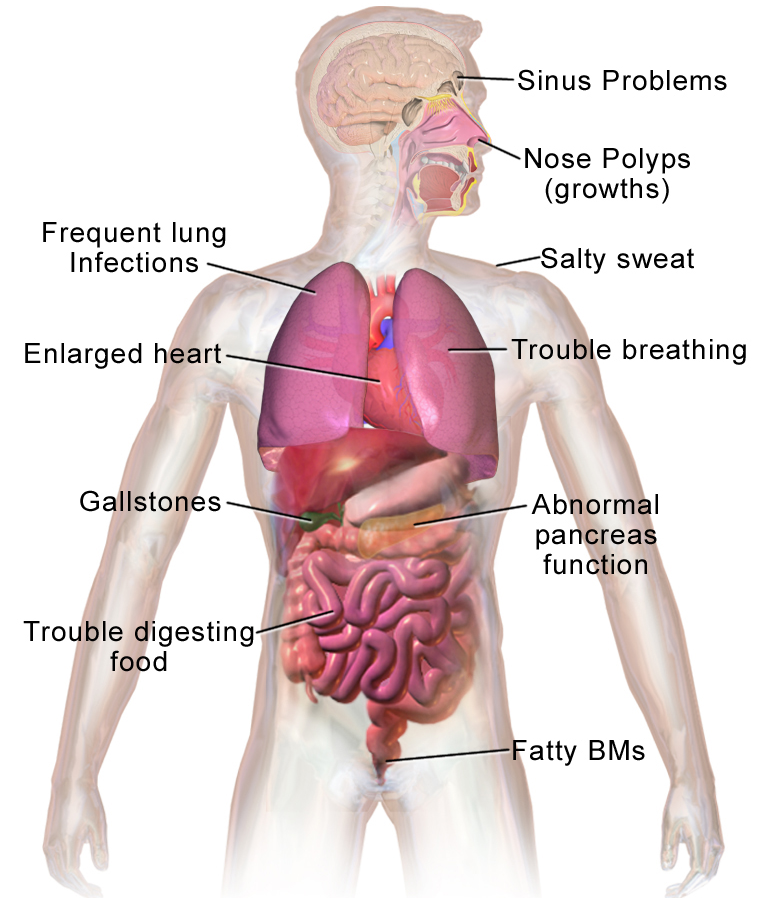
Nearly 40,000 children and adults in the United States — and more than 100,000 worldwide — are now living with cystic fibrosis. Cystic fibrosis was historically known as a disease that caused death in childhood, but survival rates have significantly improved because of advances in newborn screening, medications, nutrition, and lung transplants. With proper treatment, children diagnosed with cystic fibrosis are now expected to reach the age of 68 or older.
Influenza[13]
Influenza, commonly called “the flu,” is a viral infection that affects the epithelial cells lining the respiratory tract. Influenza viruses are different from viruses that cause the common cold. Influenza symptoms commonly include fever, headache, body aches, sore throat, nasal congestion, and cough. Some individuals, especially small children, may experience nausea and diarrhea because of the immune response to the virus, but the influenza virus is different from viruses that cause the “stomach flu.” While most individuals with influenza can manage symptoms at home and recover within several days, it can be severe and even life-threatening for those at higher risk due to potential complications. Risk factors for severe illness include children under age 2 and adults aged 65 or older, women who are pregnant, and individuals with chronic illness or weakened immune systems.
Annual flu vaccines can help protect individuals from becoming infected with seasonal influenza viruses and decrease the risk of developing severe complications. Administration of the flu vaccine to health care workers and family members can also help prevent the transmission of the virus to vulnerable individuals. Other steps to help prevent infection during “flu season” include cleaning and disinfecting surfaces, frequently washing hands, and circulating fresh air indoors.
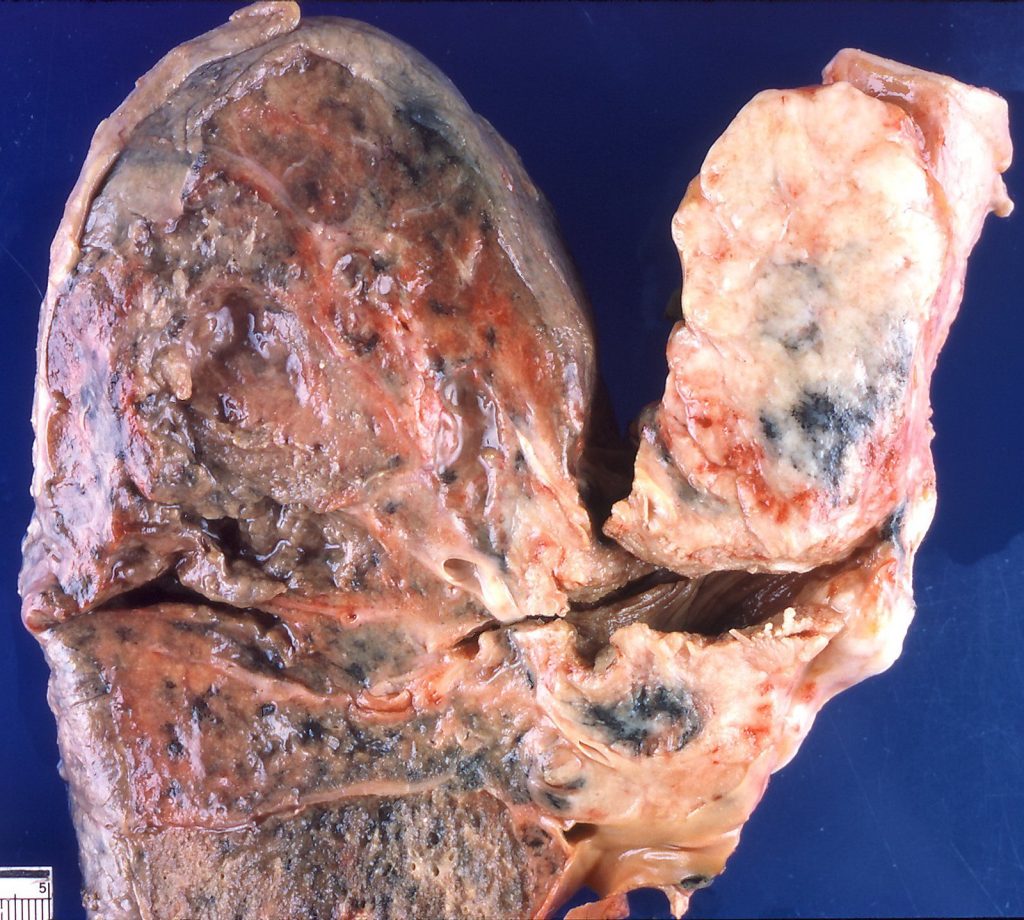
Lung Cancer[14],[15]
Lung cancer is the leading cause of cancer death in both men and women. It forms in tissues of the lung, typically in the cells that line the air passages. There are two main types of lung cancer that grow differently and are treated differently: small cell lung cancer and non-small cell lung cancer. See Figure 13.21[16] for an image of a cancerous lung.
Anyone can develop lung cancer, but factors that increase risk include the following:
- Smoking: Smoking poses the greatest risk for developing lung cancer. Tobacco smoking causes about 8 out of 10 cases of lung cancer. The number of years a person smokes and the number of cigarettes smoked each day increase the risk. Risk is also increased if a person smokes and drinks alcohol daily. If a person quits smoking, their risk is lower than if they had kept smoking, but they still have a higher risk than people who never smoked.
- Secondhand smoke: Secondhand smoke is the combination of smoke that comes from a cigarette and smoke breathed out by a smoker. People who breathe in secondhand smoke are exposed to the same cancer-causing agents as smokers, although in smaller amounts.
- Family history of lung cancer: A family history of lung cancer can increase the risk for the disease in both smokers and non-smokers.
- Exposure to toxic substances: Exposure to asbestos, arsenic, chromium, beryllium, nickel, soot, or tar in the workplace; exposure to air pollution; exposure to radiation to the chest from radiation therapy; and exposure to radon in the home increase the risk of lung cancer.
- Age: The risk of developing lung cancer increases with age, with the majority of people diagnosed with lung cancer aged 65 or older.
Lung cancer may not cause any signs or symptoms until the cancer is advanced. In fact, sometimes lung cancer is found during a chest X-ray performed for another condition. Symptoms of lung cancer may include chest discomfort, a persistent cough that does not go away or gets worse over time, coughing up blood, trouble breathing, wheezing, hoarseness, weight loss for no known reason, feeling very tired, and trouble swallowing.
Treatment of lung cancer depends on the type of lung cancer, whether it has metastasized, the patient’s overall health, and other factors. Treatments may include surgical interventions, radiation therapy, chemotherapy, and/or immunotherapy.
Read more information about the benefits of quitting smoking at The American Lung Association’s website: Benefits of Quitting.
Read more information about quitting smoking or smokeless tobacco at The American Cancer Society’s website: Quitting Smoking or Smokeless Tobacco.
Read more information about quitting e-cigarettes at The American Cancer Society’s website: Quitting E-cigarettes (Vapes, Vape Pens).
Read more information about lung cancer in the “Lung Cancer” section of Open RN Health Alterations.
Pharyngitis/Tonsillitis[17],[18],[19]
Pharyngitis refers to inflammation of the pharynx or throat, and tonsillitis refers to inflammation of the tonsils. Although there is a distinction between the two disorders, they can coexist. Both disorders are commonly referred to as a “sore throat” and have similar pathophysiologies, signs and symptoms, and treatment. Pharyngitis and tonsillitis are typically caused by bacterial or viral infections. However, pharyngitis can also be caused by allergies, acid reflux, or cancer. Common viral causes of pharyngitis and tonsillitis are rhinovirus, coronavirus, and adenovirus. Although there are a variety of bacteria that can lead to pharyngitis or tonsillitis, the most common is Group A beta-hemolytic streptococcus (GABHS), also called GBS. This is also known as “strep throat” and is common in school-aged children. When pharyngitis and/or tonsillitis caused by GABHS is not treated, scarlet fever or post-streptococcal glomerulonephritis can develop. Scarlet fever is an inflammatory disease that causes inflammation of the joints and the valves of the heart. Classic symptoms of scarlet fever are a bright red rash that covers most of the body and a high fever. Post-streptococcal glomerulonephritis refers to inflammation of the glomeruli of the kidneys, leading to edema, increased blood pressure, and alterations in kidney function. Medical treatment for pharyngitis and tonsillitis is based on the causative factor of the disorder. When caused by a bacterial infection such as GABHS, antibiotics are required. However, antibiotic therapy is ineffective if the causative organisms are viral or fungal. Antibiotics will not only treat the bacterial infection but also shorten the duration of the illness and prevent the development of scarlet fever. They may also help prevent the development of post-streptococcal glomerulonephritis.
Pleuritis/Pleurisy[20]
Pleuritis, also known as pleurisy, is inflammation of the pleura, the membranes surrounding the lungs and chest wall. It is characterized by sharp chest pain that worsens with breathing, coughing, or movement and may radiate to the shoulder and back. The pain is caused by the plurae rubbing together instead of smoothly gliding. Pleuritis can be caused by a variety of conditions, but the most common cause is a viral infection. Treatment depends upon the underlying cause, but the pain is often managed with acetaminophen (Tylenol) or nonsteroidal anti-inflammatory drugs (NSAIDs).
Pneumonia[21]
Pneumonia is an infection that inflames the alveoli, causing them to fill with fluid or pus. Symptoms include a productive cough with fever, chills, and difficulty breathing. A variety of organisms, including bacteria, viruses, and fungi, can cause pneumonia. See Figure 13.22[22] for an image depicting healthy alveoli compared to the alveoli of someone with pneumonia.
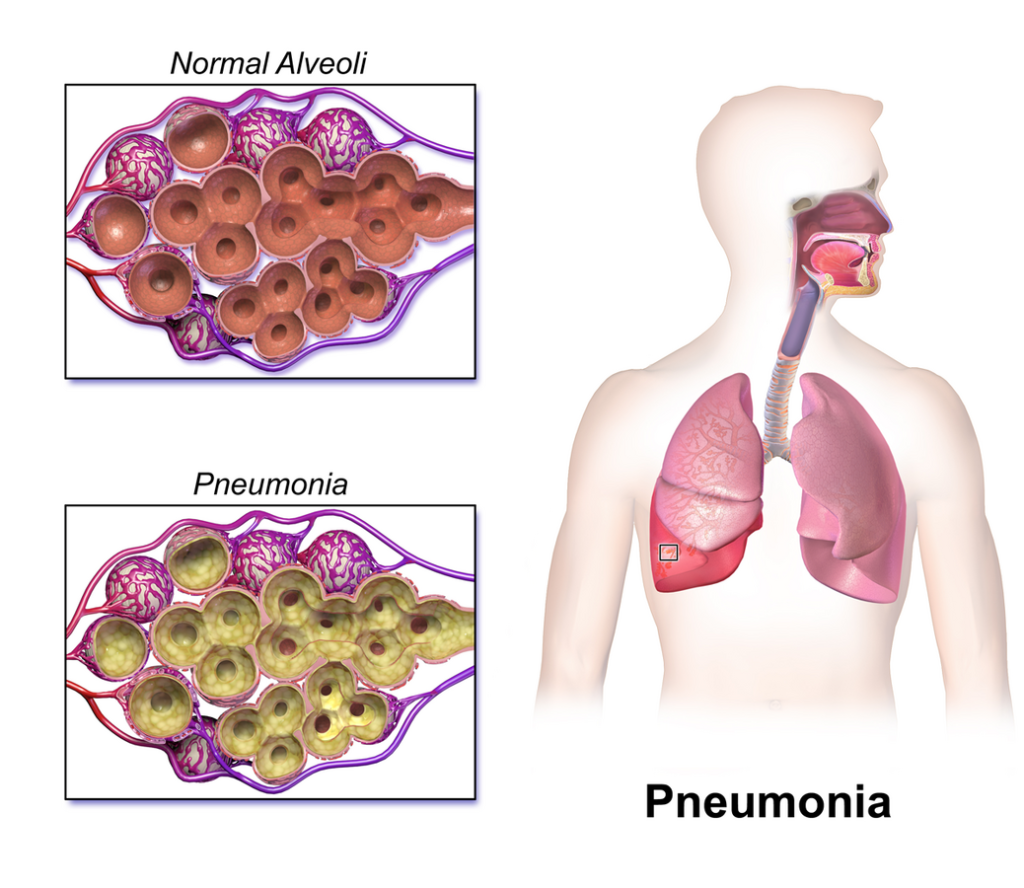
Pneumonia can range in severity from mild to life-threatening, with increased risk for infants and young children, adults aged 65 or older, and people with health problems or weakened immune systems. Vaccinations are available to prevent certain types of pneumonia for those at increased risk.
Treatment depends on the type and severity of the pneumonia. Common treatments include antibiotics for bacterial cases, antivirals for viral cases, antifungals for fungal cases, cough medications, and acetaminophen or ibuprofen to relieve pain and/or fever. Severe cases require hospitalization for intravenous antibiotics, oxygen administration, and other medical treatments.
Read more information about pneumonia in the “Pneumonia” section of Open RN Health Alterations.
Pneumothorax[23]
A pneumothorax occurs when air leaks into the space between the lung and the chest wall, causing the lung to collapse. This can happen due to injuries such as from a car accident or stab wounds; certain medical procedures like placement of central lines or biopsies that damage the lung; or lung disorders like asthma, COPD, pneumonia, or lung cancer. In some cases, a pneumothorax occurs spontaneously without an obvious cause. A tension pneumothorax is a medical emergency that occurs when pressure builds up inside the chest as air enters and cannot escape.
Symptoms of a pneumothorax include sudden chest pain, shortness of breath, and cyanosis (bluish skin due to lack of oxygen). Treatment depends on the cause, size, and severity of the pneumothorax. In severe cases, a thoracentesis is performed, where a needle is placed between the ribs to evacuate the excess air in the chest. A chest tube may be placed inside the chest for a few days or longer to reduce the air in the pleural space. As the air pressure decreases, the lung re-expands and heals. To prevent the lung from collapsing again, pleurodesis may be performed where a chemical powder is placed in the lung to help attach it to the chest cavity, eliminating extra space.
Pulmonary Edema[24]
Pulmonary edema is a serious condition where fluid accumulates in the lungs, making it difficult to breathe. This buildup of fluid interferes with the gas exchange of oxygen and carbon dioxide, potentially leading to hypoxemia (low blood oxygen levels) and respiratory failure. Acute pulmonary edema can be life-threatening and requires immediate medical attention. Pulmonary edema is often caused by heart failure, where the heart’s inability to pump efficiently leads to blood backing up in the lungs. It may also be caused by kidney failure, liver failure, infections, certain medications, lung injury, or exposure to high altitudes.
Symptoms of pulmonary edema include dyspnea, especially when lying down, a productive cough of pink, frothy liquid, sweating, and anxiety. It is commonly treated with medications to remove excess fluid buildup and oxygen administration. In severe cases, respiratory therapy with noninvasive ventilation or intubation and mechanical ventilation may be required.
Pulmonary Embolism[25]
A pulmonary embolism (PE) is a blood clot or other substance, such as fat or an air bubble, that has traveled through the bloodstream and lodged in a smaller vessel within the pulmonary circulation in the lungs and obstructed blood flow. This blockage causes lack of oxygen delivery to the tissues supplied by that blood vessel. A PE is a medical emergency that requires rapid treatment to prevent severe damage to the lungs or heart and death. Symptoms of a PE may include sudden, severe shortness of breath; sharp pain in the chest or arm; and pale, clammy skin. Treatment includes medications to dissolve the clot or procedures to remove the clot in order to quickly restore adequate pulmonary circulation.
Respiratory Distress Syndrome[26]
Respiratory distress syndrome (RDS) is a condition that primarily affects premature babies, causing difficulty breathing. It is commonly caused by insufficient surfactant in the lungs that keep the alveoli inflated. Symptoms of RDS include rapid, shallow breathing; grunting; flaring of the nostrils; and subcostal, subxiphoid, intercostal, and suprasternal contractions. Treatment usually involves surfactant replacement therapy, oxygen administration, and respiratory treatments. In severe cases, intubation and mechanical ventilation are required. Many patients will continue to have complications during and after the acute course of RDS. RDS can be reduced by the administration of corticosteroids before a premature infant is born.
Sleep Apnea[27]
Sleep apnea is a chronic disorder that can occur in children or adults and is characterized by the cessation of breathing during sleep for several seconds. Sleep apnea leads to poor sleep, reflected in the symptoms of fatigue, morning headaches, evening napping, irritability, and memory problems. In addition, many individuals with sleep apnea experience a dry throat in the morning after waking from sleep, which may be due to excessive snoring.
There are two types of sleep apnea: obstructive sleep apnea and central sleep apnea. Obstructive sleep apnea is caused by an obstruction of the airway during sleep, which can occur at different parts in the airway, depending on the underlying cause of the obstruction. For example, the tongue and throat muscles of some individuals with obstructive sleep apnea may relax excessively, causing the muscles to push into the airway. Another example is obesity as excess adipose tissue in the neck region can push the soft tissues towards the lumen of the airway, causing the trachea to narrow.
In central sleep apnea, the respiratory centers of the brain do not respond properly to rising carbon dioxide levels and, therefore, do not stimulate the contraction of the diaphragm and intercostal muscles regularly. As a result, inspiration does not occur and breathing stops for a short period. In some cases, the cause of central sleep apnea is unknown. However, some medical conditions, such as stroke and heart failure, may cause damage to the pons or medulla oblongata. In addition, some medications, such as morphine can affect the respiratory center and decrease the respiratory rate to life-threatening levels. The symptoms of central sleep apnea are similar to those of obstructive sleep apnea.
Sleep apnea is diagnosed with a sleep study where the patient’s blood oxygen levels, heart rate, respiratory rate, and blood pressure are monitored. In severe cases, brain activity and the volume of air that is inhaled and exhaled are also monitored.
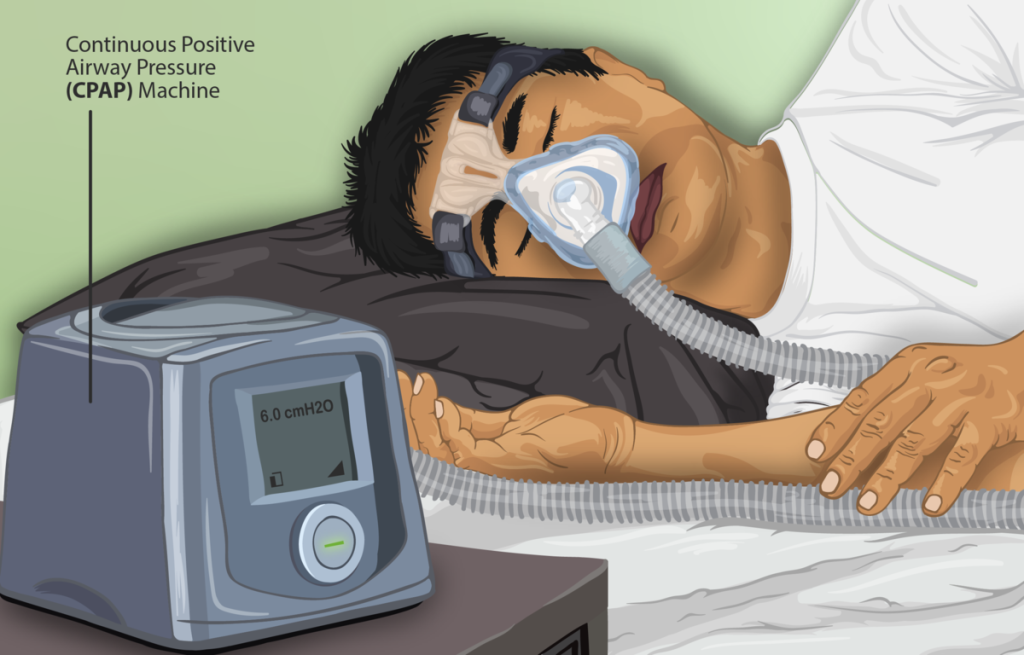
Treatment of obstructive sleep apnea commonly includes the use of a device called a continuous positive airway pressure (CPAP) machine during sleep. The CPAP machine has a mask that covers the nose, or both the nose and mouth, and forces air into the airway at regular intervals. This pressurized air can help to gently force the airway to remain open, allowing more normal ventilation to occur. See Figure 13.23[28] for an image of a patient using a CPAP machine. Other treatments include lifestyle changes to lose weight, changes in sleeping position, and eliminating alcohol and medications that trigger sleep apnea. In addition to these treatments, patients with central sleep apnea may need supplemental oxygen during sleep.
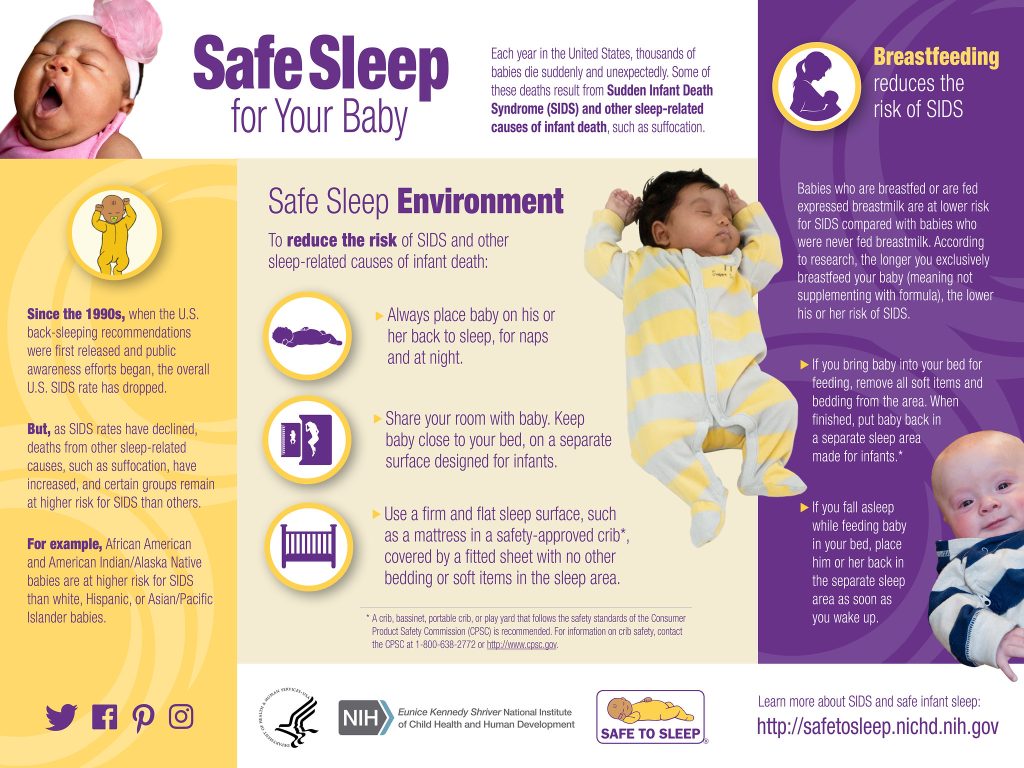
Sudden Infant Death Syndrome (SIDS)[29],[30]
Sudden infant death syndrome (SIDS) is the sudden and unexplained death of a baby younger than one year old who otherwise appears healthy. SIDS is one of the leading causes of death in babies from ages 1 month to 1 year and happens most often between 2 and 4 months old. The cause of SIDS is unknown, but there are multiple factors related to SIDS. SIDS may be caused by problems in the area of an infant’s brain that controls breathing and waking up from sleep. SIDS can happen to any infant, but premature infants and those with low-birth weight are at higher risk. Exposure to secondhand smoke and a recent upper respiratory infection also increase the risk for SIDS. Other risk factors for SIDS include the following:
- Sleeping on their stomach or side: Babies placed in these positions to sleep may have more trouble breathing than those placed on their backs, especially premature infants.
- Sleeping on a soft surface: Lying face down on a fluffy comforter, a soft mattress, or a waterbed can block an infant’s airway.
- Sharing a bed: The risk of SIDS rises if a baby sleeps in the same bed with parents, siblings, or pets, but sleeping in a separate bed in the same room with parents lowers the risk of SIDS.
- Overheating: Being too warm while sleeping can increase a baby’s risk of SIDS.
Safe sleep practices play a large role in preventing SIDS. Infants should be placed on their back to sleep in a crib with a firm mattress and without toys, blankets, crib bumpers, or pillows. Infants should not be placed in a bed with other children or adults, and overheating should be avoided. Mothers are encouraged to breastfeed because this has been shown to reduce the risk of SIDS. Vaccinations should be kept up-to-date, especially to prevent respiratory illnesses that increase the risk of SIDS. See Figure 13.24[31] for tips on safe sleep practices for infants.
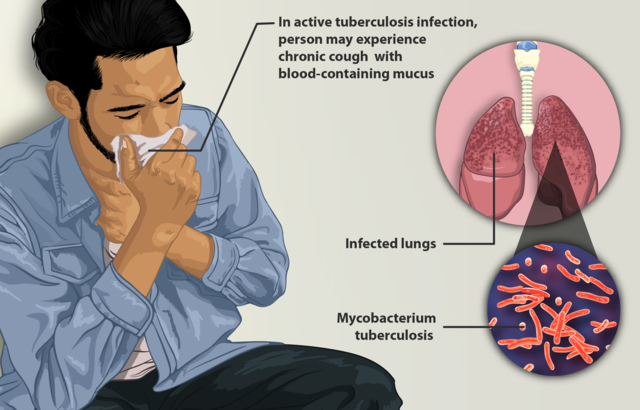
Tuberculosis[32],[33]
Tuberculosis (TB) is a leading cause of death worldwide due to infectious disease. TB usually affects the lungs but can also affect multiple parts of the body, such as the brain, the kidneys, or the spine. In the United States, the majority of TB cases are caused by Mycobacterium tuberculosis. Other mycobacteria (such as Mycobacterium bovis) can also cause TB disease in people.
Primary risk factors include close contact with a TB-infected person, HIV infection or otherwise weakened immune system, and substance abuse. TB is a common disease around the world, so individuals who travel or live in regions with high TB prevalence such as Africa, Asia, or parts of Latin America have increased risk. Individuals who emigrate from high-incidence countries or experience homelessness are also at increased risk. Additionally, individuals who live in overcrowded environments are at increased risk for TB transmission, including individuals who work or live in long-term health care settings or prisons.
Not everyone exposed to TB bacteria becomes sick. There are two types of TB: latent TB (or inactive TB infection) and active TB disease. When the TB bacillus enters the lung, it replicates over the course of 2-12 weeks and the immune response becomes activated. The immune response involves macrophages and lymphocytes migrating to the site of inflammation and walling off the bacillus, forming a tubercle. Individuals with healthy immune systems may heal this initial lesion and develop latent TB before any signs or symptoms of the illness occur. However, the tubercle may calcify and remain dormant for many years, but over time, or in immunocompromised states, spread to other areas of the lung or to other organs. The CDC estimates up to 13 million people in the United States live with inactive TB. These individuals do not feel sick or have symptoms and cannot spread TB to others.
Active TB disease occurs if an individual’s immune system cannot stop the TB bacilli from multiplying. People with active TB disease feel sick. Common symptoms of active TB are a cough (that may or may not contain blood), weight loss, night sweats, fatigue, chills, and fever. The TB infection can spread to people through respiratory droplets that are coughed into the air. Without treatment, active TB disease is typically fatal. See Figure 13.25[34] for a depiction of a patient with active TB disease.
The CDC recommends that people who are at increased risk for TB should be tested regularly. There are two types of tests that can detect TB infection, but these tests cannot distinguish between active and latent TB:
- Tuberculin Skin Test (Mantoux Test): A small amount of tuberculin protein is injected just beneath the skin, usually in the forearm. The test is read 48 to 72 hours later. A positive reaction indicates exposure to TB or the BCG vaccine, but it does not confirm active disease. In regions of the world with high TB prevalence, a Bacillus Calmette-Guérin (BCG) vaccine is commonly administered. Receiving a BCG vaccine has a substantial effect on tuberculin skin tests, with individuals who received BCG after infancy having tuberculin skin test reactions up to 55 years post-immunization.
- TB blood test: The TB blood test is also called an interferon-gamma release assay (IGRA). The TB blood test measures how the immune system reacts to the bacteria that cause TB. (If an individual received a BCG vaccine, they should be tested using the TB blood test. Unlike the TB skin test, TB blood tests are not affected by the BCG vaccine.)
If a patient has a positive TB skin or blood test, further testing is needed to determine if they have a latent or active infection. These tests include a chest X-ray, as well as sputum cultures.
TB is treated with multiple antibiotics for one year or longer. Mycobacterium tuberculosis has developed drug resistance in many areas of the world, causing a significant treatment problem. After medication therapy has been initiated, sputum cultures are obtained to assess treatment response. Patients are considered infectious until three negative sputum samples have been obtained, typically after approximately three months of treatment.
Read more about tuberculosis in the “Tuberculosis” section of Open RN Health Alterations.
Upper Respiratory Infection[35],[36]
An upper respiratory tract infection (URI), also known as the common cold, can be described as the swelling and irritation of the upper airways, including the nose, sinuses, throat, larynx, and larger airways. Although a variety of infectious organisms can lead to a URI, the most common causative organism is rhinovirus. Risk factors for a URI include contact with school-aged children, underlying respiratory issues, exposure to smoke, and immunodeficiency.
A URI results when a client inhales infected respiratory droplets that then invade the mucosa of the upper respiratory tract. Once deposited in the mucosa, the infectious organism begins to replicate. The infected individual will then mount an inflammatory response, which leads to dilation and increased permeability of blood vessels, ultimately contributing to the symptoms of the URI. Common symptoms include cough; sore throat; runny nose; stuffy nose; headache; fever; sneezing; and a general feeling of illness, weakness, or discomfort. Symptoms begin one to three days after exposure to the infectious organism and usually last seven to ten days. However, symptoms can sometimes last up to three weeks. Potential complications of a URI caused by rhinovirus are exacerbations of asthma, ear infections, sinus infections, bronchitis, or pneumonia.
There is no cure for the common cold. Treatment focuses on symptomatic relief with the use of over-the-counter medications.
- Centers for Disease Control and Prevention. (n.d.). Asthma. https://www.cdc.gov/asthma/ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Health alterations. Open RN | WisTech Open. https://wtcs.pressbooks.pub/healthalts/ ↵
- “Asthma Illustration” by National Heart, Lung and Blood Institute, National Institutes of Health is licensed under CC BY-NC 2.0 ↵
- Grott, K., Chauhan, S., Sanghavi, D. K., et al. (2024). Atelectasis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK545316/ ↵
- Mayo Clinic. (2025). Carbon monoxide poisoning. https://www.mayoclinic.org/diseases-conditions/carbon-monoxide/symptoms-causes/syc-20370642 ↵
- Mayo Clinic. (2024). COPD. https://www.mayoclinic.org/diseases-conditions/copd/symptoms-causes/syc-20353679 ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Health alterations. Open RN | WisTech Open. https://wtcs.pressbooks.pub/healthalts/ ↵
- “COPD (Chronic Obstructive Pulmonary Disease) Illustration” by National Heart, Lung and Blood Institute, National Institutes of Health is licensed under CC BY-NC 2.0 ↵
- World Health Organization. (2024). Coronavirus disease (COVID-19). https://www.who.int/health-topics/coronavirus#tab=tab_1 ↵
- Centers for Disease Control and Prevention. (2025). How to protect yourself and others. https://www.cdc.gov/covid/prevention/index.html ↵
- National Heart, Lung, and Blood Institute. (2024). What is cystic fibrosis? https://www.nhlbi.nih.gov/health/cystic-fibrosis ↵
- “Blausen_0286_CysticFibrosis” by Blausen.com staff (2014). “Medical gallery of Blausen Medical 2014” is licensed under CC BY 3.0 ↵
- Mayo Clinic. (2024). Influenza (flu). https://www.mayoclinic.org/diseases-conditions/flu/symptoms-causes/syc-20351719 ↵
- National Cancer Institute. (n.d.). Lung cancer. MedlinePlus [Internet]. https://medlineplus.gov/lungcancer.html ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Health alterations. Open RN | WisTech Open. https://wtcs.pressbooks.pub/healthalts/ ↵
- “Small cell carcinoma” by Dr. Yale Rose Atlas of Pulmonary Pathology is licensed under CC BY-SA 2.0 ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Health alterations. Open RN | WisTech Open. https://wtcs.pressbooks.pub/healthalts/ ↵
- Johns Hopkins Medicine. (n.d.). Pharyngitis and tonsillitis. https://www.hopkinsmedicine.org/health/conditions-and-diseases/pharyngitis-and-tonsillitis ↵
- Anderson, J., & Paterek, E. (2023). Tonsillitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK544342 ↵
- National Heart, Lung, and Blood Institute. (2022). What are pleural disorders? https://www.nhlbi.nih.gov/health/pleural-disorders ↵
- Mayo Clinic. (2020). Pneumonia. https://www.mayoclinic.org/diseases-conditions/pneumonia/symptoms-causes/syc-20354204 ↵
- “Blausen_0994_Pneumonia” by BruceBlaus is licensed under CC BY-SA 4.0 ↵
- Cleveland Clinic. (2022). Pneumothorax (collapsed lung). https://my.clevelandclinic.org/health/diseases/15304-collapsed-lung-pneumothorax ↵
- Malek, R., & Soufi, S. (2023). Pulmonary edema. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK557611/ ↵
- Cleveland Clinic. (2022). Pulmonary embolism. https://my.clevelandclinic.org/health/diseases/17400-pulmonary-embolism ↵
- Yadav, S., & Lee, B. (2023). Neonatal respiratory distress syndrome. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK560779/ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Health alterations. Open RN | WisTech Open. https://wtcs.pressbooks.pub/healthalts/ ↵
- “Depiction_of_a_Sleep_Apnea_patient_using_a_CPAP_machine” by https://www.myupchar.com/en is licensed under CC BY-SA 4.0 ↵
- Stanford Medicine Children’s Health. (n.d.). Sudden infant death syndrome (SIDS). https://www.stanfordchildrens.org/en/topic/default?id=sudden-infant-death-syndrome-sids-90-P02412&sid=33192 ↵
- Mayo Clinic. (2024). Sudden infant death syndrome (SIDS). https://www.mayoclinic.org/diseases-conditions/sudden-infant-death-syndrome/symptoms-causes/syc-20352800 ↵
- “Safe Sleep for Your Baby” by NICHD is licensed under CC BY-ND 2.0 ↵
- Centers for Disease Control and Prevention. (n.d.). About tuberculosis. https://www.cdc.gov/tb/about/index.html[ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Health alterations. Open RN | WisTech Open. https://wtcs.pressbooks.pub/healthalts/ ↵
- “Depiction_of_a_tuberculosis_patient” by https://www.myupchar.com/en is licensed under CC BY-SA 4.0 ↵
- Thomas, M., & Bomar, P. A. (2023). Upper respiratory tract infection. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK532961/ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2025). Nursing health promotion. Open RN | WisTech Open. https://wtcs.pressbooks.pub/healthpromo/ ↵
A common chronic respiratory disease characterized by episodes of bronchospasms (constriction of the bronchioles), inflammation, and edema of the airway that makes it difficult to exhale air.
Constriction of the bronchioles.
Occurs when alveoli lose air and collapse.
Occurs when carbon monoxide (CO) builds up in the blood that can lead to serious tissue damage or death.
A chronic, progressive lung disease caused by inflammation inside the airways resulting in limited airflow out of the lungs, known as obstruction.
An infectious respiratory disease caused by the SARS-CoV-2 virus.
A genetic condition that alters a protein in the body involved in the function of the cells, tissues, and glands responsible for producing mucus and sweat.
Commonly called “the flu,” is a viral infection that affects the epithelial cells lining the respiratory tract.
The leading cause of cancer death in both men and women.
Inflammation of the pharynx or throat.
Inflammation of the tonsils.
Inflammation of the pleura, the membranes surrounding the lungs and chest wall.
An infection that inflames the alveoli, causing them to fill with fluid or pus.
Occurs when air leaks into the space between the lung and the chest wall, causing the lung to collapse.
A serious condition where fluid accumulates in the lungs, making it difficult to breathe.
A blood clot or other substance, such as fat or an air bubble, that has traveled through the bloodstream and lodged in a smaller vessel within the pulmonary circulation in the lungs and obstructed blood flow.
A condition that primarily affects premature babies, causing difficulty breathing.
Chronic disorder that can occur in children or adults and is characterized by the cessation of breathing during sleep for several seconds.
Sudden and unexplained death of a baby younger than one year old who otherwise appears healthy.
A potentially fatal infectious disease, primarily affecting the lungs but capable of spreading to other organs; caused by Mycobacterium tuberculosis in most U.S. cases.
Known as the common cold, can be described as the swelling and irritation of the upper airways, including the nose, sinuses, throat, larynx, and larger airways.

