8.9 Male Reproductive System Disorders
Benign Prostatic Hypertrophy
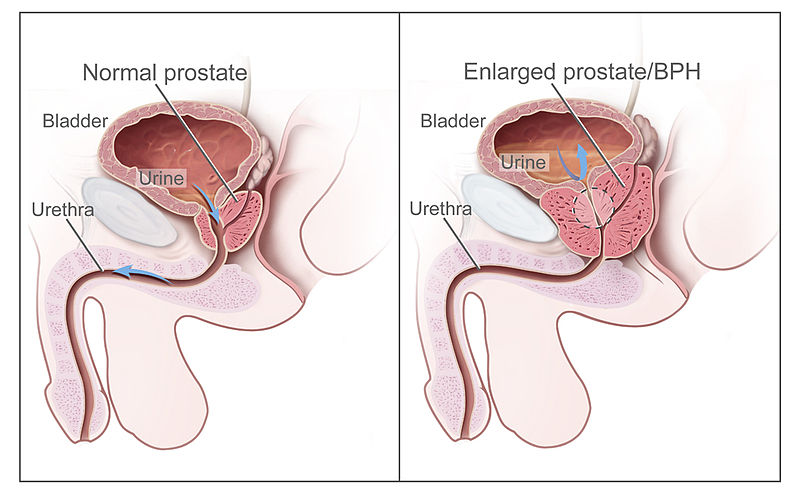
Benign prostatic hyperplasia (BPH) refers to enlargement of the prostate that is not cancerous. See Figure 8.29[1] for an illustration of BPH. BPH is a common condition in males aged 50 and older. The prostate presses against the urethra, causing it to narrow. Eventually, the bladder becomes weak from trying to pass urine through the narrowed urethra. It loses its ability to completely empty, leaving some urine in the bladder called urinary retention. The inability to completely empty the bladder causes many of the symptoms associated with BPH, such as a frequent and intense urge to urinate, urinating frequently at night, difficulty starting a urine stream or a weak stream, and a sensation that the bladder has not emptied completely. If urinary retention is not addressed, it can cause complications such as urinary tract infections, bladder damage, and kidney damage.[2]
A health care provider may order several types of medical tests to diagnose BPH, such as urodynamic testing or a cystoscopy. BPH may be treated with medications or transurethral procedures where an instrument is inserted through the urethra to widen the urethra or destroy part of the prostate with heat. Surgery may be performed when symptoms are severe, other treatments haven’t helped, or a complication has developed such as bladder damage. Surgeries remove part or all of the prostate or make cuts in the prostate to take pressure off the urethra. For example, transurethral incision of the prostate (TUIP) is a procedure that widens the urethra by making a few small incisions in the bladder neck and the prostate gland. Transurethral resection of the prostate (TURP) is the surgical removal of pieces of the prostate gland by using an instrument inserted through the urethra.[3]
Read more about BPH in the “Benign Prostate Hypertrophy” section of the “Renal and Urinary System Alterations” chapter in Open RN Health Alterations.
Epididymitis
Epididymitis is infection or inflammation of the epididymis, a tubular structure on the testis where sperms mature. Epididymitis is a relatively common condition that is easily confused with testicular torsion. Epididymitis is managed medically, whereas testicular torsion is a surgical emergency. The majority of cases of epididymitis occur due to bacterial infection from common urinary pathogens or sexually transmitted diseases. It can also occur due to trauma or repetitive activities such as sports. Symptoms of epididymitis include scrotal pain and swelling that is often gradual in onset rather than acute. Urinary symptoms such as dysuria, urinary frequency, urgency, incontinence, or urethral discharge may also occur. Diagnostic testing begins with urinalysis, and ultrasound is often performed to evaluate vascular flow to the testis and rule out testicular torsion. Treatment typically includes antibiotic therapy depending upon the causative organism, rest, ice, scrotal support, and anti-inflammatory medication. If sexual abuse is suspected as a cause of trauma, the nurse and/or health care provider should contact local authorities, child protective services, or other social service agencies based upon state law.[4]
Epispadias
Epispadias is a rare congenital anomaly in which the urethra opens onto the dorsal aspect of the penis with other characteristic anatomic abnormalities, including a short, upward-pointing phallus. Epispadias is apparent at birth and is treated surgically. There is no urgent need for surgery in newborns, but it is recommended that the procedure be performed before the age of toilet training.[5]
Erectile Dysfunction
Erectile dysfunction (ED) is the inability to achieve or maintain an erection. ED is a common condition as men age, with 40% of men at age 40 and up to 70% of men by age 70 years experiencing ED. ED is also associated with side effects of some medications and many medical disorders such as high blood pressure, diabetes, cardiovascular disease, kidney disease, prostate disorders, and low testosterone levels. ED may be treated with lifestyle changes, medications that relax smooth muscle and increase blood flow in the penis during sexual stimulation (such as sildenafil), or surgical implantation of a device to create an erection.[6]
Hydrocele
A hydrocele is a type of swelling in the scrotum, the pouch of skin that holds the testicles. This swelling happens when fluid collects in the thin sac that surrounds a testicle. Hydroceles are common in newborns. They often go away without treatment by age one. Older children and adults can get a hydrocele due to an injury to the scrotum or other health problems. For example, a hydrocele may develop after surgery for varicocele, enlarged veins of the spermatic cord that can cause scrotal swelling.[7]
Hypospadias
Hypospadias is a common penile congenital malformation causing abnormal positioning of the urethral opening and possible abnormal penile positioning. Hypospadias is classified based on the location of the urethra[8]:
- Anterior (subcoronal and glandular)
- Middle (distal penile, proximal penile, and midshaft)
- Posterior (scrotal, penoscrotal, and perineal)
Diagnosis is made during physical examination soon after birth. In almost all cases the prepuce is incomplete ventrally, as well as the urethra being in an abnormal location. If the infant has a complete foreskin, hypospadias may become obvious after circumcision. Some cases also have coexisting conditions of cryptorchidism, inguinal hernia, or other genetic syndromes. Infants are referred to a urologist for diagnostic treatment and surgical repair. Nurses can help counsel adult males with hypospadias who may experience disturbed body image that affects their sexual health.[9]
Male Infertility
Nearly 1 in 7 couples is infertile, which means they haven’t been able to conceive a child even though they’ve had frequent, unprotected sexual intercourse for a year or longer. In up to half of these couples, male infertility plays a role. Male infertility can be caused by low sperm production, abnormal sperm function, or blockages that prevent the delivery of sperm. Illnesses, injuries, chronic health problems, lifestyle choices, and other factors may contribute to male infertility.[10]
For a male to cause pregnancy, the following processes must occur[11]:
- Healthy sperm are produced. At least one testicle must be functioning, and the body must produce testosterone and other hormones to trigger and maintain sperm production.
- Sperm must be carried into the semen. After sperm are produced in the testicles, tubes transport them until they mix with semen and are ejaculated out of the penis.
- There must be enough sperm in the semen. If the number of sperm in the semen (referred to as sperm count) is low, it decreases the odds that one sperm will fertilize a partner’s egg. A low sperm count is fewer than 15 million sperm per milliliter of semen or fewer than 39 million per ejaculate. Aspermia refers to failure to produce sperm.
- Sperm must be functional and able to move. If the movement (referred to as motility) or the function of sperm is abnormal, the sperm may not be able to reach or penetrate the partner’s egg.
There are several possible causes of male infertility. If a couple is not able to conceive within one year of having unprotected sex, nurses encourage the couple to see fertility specialists for diagnostic testing and infertility treatment.[12] Read additional information about male infertility in the “Infertility” section of the “Reproductive System Alterations” chapter.
Paraphimosis
Paraphimosis is a urologic emergency that occurs in uncircumcised males when the foreskin becomes trapped behind the corona of the glans penis. It causes strangulation of the glans, painful vascular compromise, distal venous engorgement, edema, and necrosis. The client typically experiences acute, distal penile pain and swelling. Paraphimosis may occur when the foreskin is retracted for cleaning or placement of a urinary catheter, or during a procedure such as a cystoscopy. Mild, uncomplicated paraphimosis can be reduced manually by a urologist, but more difficult cases may require local anesthesia and/or surgical intervention. It is essential for nurses to routinely replace the foreskin after inserting a urinary catheter to prevent the development of a paraphimosis in uncircumcised males.[13]
Peyronie’s Disease
Peyronie’s disease is a disorder in which scar tissue forms under the skin of the penis in the thick elastic membrane called the tunica albuginea. The tunica albuginea helps keep the penis stiff during an erection. The scar tissue pulls on the surrounding tissues and causes the penis to curve or bend. Curves in the penis can make erections painful and may make sexual intercourse painful, difficult, or impossible. Men who are at higher risk of developing Peyronie’s disease include those who engage in vigorous sexual or nonsexual activities that cause micro-injuries to the penis, have certain connective tissue or autoimmune disorders, have a family history of Peyronie’s disease, have diabetes, erectile dysfunction, or prostate cancer that was treated with surgery. Urologists treat Peyronie’s disease with lifestyle changes, medications, or surgical treatment.[14]
Phimosis
Phimosis refers to difficulty retracting the prepuce beyond the glans of the penis. There are two types of phimoses called physiologic and pathologic. Physiologic phimosis is common in children between two and four years of age and resolves once the foreskin becomes more retractile. Pathologic phimosis is caused by a skin condition that is thought to be related to an autoimmune reaction. There may be associated irritation, local infection, dysuria, bleeding, and meatal stenosis. Pathological phimosis is typically treated with topical steroids or circumcision.[15]
Prostate Cancer
Cancer of the prostate gland is the second most common cancer occurring in men. In the U.S., about 1 out of 8 men will be diagnosed with prostate cancer. Symptoms of prostate cancer are initially similar to benign prostatic hypertrophy (BPH), such as trouble starting a urine stream and frequent urination, especially at night, and trouble emptying the bladder. Symptoms of advanced prostate cancer that have metastasized to other areas of the body include pain in the back, hips, or pelvis that doesn’t go away, shortness of breath, fatigue, fast heartbeat, dizziness, pale skin caused by anemia, hematuria, blood in the semen, dysuria, and erectile dysfunction. Prostate cancer usually grows very slowly, so treating it before symptoms occur may not improve men’s health or help them live longer.[16]
Diagnostic testing for prostate cancer may include a prostate-specific antigen (PSA) blood test that measures a substance made by the prostate that may be found in higher-than-normal amounts in the blood of men who have prostate cancer. However, PSA levels may also be elevated in men who have BPH or prostatitis, so it is not a very reliable test. Additional imaging and biopsy tests are also performed.[17]
There are several types of treatment for clients with prostate cancer, depending on the stage of the cancer and if it has metastasized[18]:
- Watchful waiting
- Surgery
- Radiation therapy and radiopharmaceutical therapy
- Hormone therapy
- Bisphosphonate therapy
- Chemotherapy
- Targeted therapy
- Immunotherapy
Watchful waiting refers to treatment used for older men whose prostate cancer is found during a screening test, but do not have signs or symptoms. Watchful waiting means closely monitoring a client’s condition without treatment unless signs or symptoms appear, or test results change. Treatment is provided to relieve symptoms and improve quality of life.
Read more about prostate cancer in the “Bladder and Prostate Cancer” section of the “Renal and Urinary System Alterations” chapter of Open RN Health Alterations.
Prostatitis
Prostatitis refers to inflammation of the prostate gland and sometimes areas surrounding it. Prostatitis can be acute or chronic, and some types are caused by a bacterial infection. Symptoms of acute bacterial prostatitis are typically severe and come on suddenly, whereas chronic prostatitis develops slowly and lasts three or more months. Symptoms may include the following[19]:
- Urinary frequency
- Urinary urgency
- A weak or an interrupted urine stream
- Dysuria
- Fever and/or chills
- Painful ejaculation
- Pain in the penis or testicles
A health care provider diagnoses prostatitis by performing diagnostic tests, such as a urinalysis and cystoscopy. Treatment depends upon the cause and may include antibiotics and pain relievers.[20]
Spermatocele
A spermatocele is an abnormal sac (cyst) that develops in the epididymis, the small, coiled tube located on the upper testicle that collects and transports sperm. The cause of spermatoceles is unknown but could be due to a blockage in one of the tubes that transports sperm. If a spermatocele grows large enough to cause discomfort, surgery may be required.[21]
Testicular Torsion
Testicular torsion occurs when a testicle rotates, twisting the spermatic cord that brings blood to the scrotum. The reduced blood flow causes sudden, severe pain and swelling. Testicular torsion commonly occurs between ages 12 and 18 and usually requires emergency surgery. If treated quickly, the testicle can usually be saved. But when blood flow has been cut off for too long, a testicle might become so badly damaged that it has to be removed.[22]
Testicular Cancer
Testicular cancer is cancer that begins in the cells that make sperm in the testicle. It is rare and is most frequently diagnosed in men ages 20 to 34. Most testicular cancers can be cured, even if diagnosed at an advanced stage. Common symptoms of testicular cancer are a painless lump in the testicle, a dull ache in the lower abdomen or the groin, a sudden build-up of fluid in the scrotum, and pain in a testicle or in the scrotum. Diagnostic tests include an ultrasound of the testes and blood tests for tumor markers. Treatment includes inguinal orchiectomy, a procedure to remove the entire testicle through an incision in the inguinal region of the groin.[23]
Nurses encourage male clients to be aware of their bodies and to report concerning symptoms to their health care provider. The U.S. Preventive Services Task Force (USPSTF) has reaffirmed its 2004 recommendation against routine screening for testicular cancer in adolescent and adult males without any symptoms.[24]
- “Benign_Prostatic_Hyperplasia_nci-vol-7137-300.jpg” by unknown author for National Cancer Institute is licensed in the Public Domain. ↵
- MedlinePlus [Internet]. (2022). Enlarged prostate (BPH). https://medlineplus.gov/enlargedprostatebph.html ↵
- MedlinePlus [Internet]. (2022). Enlarged prostate (BPH). https://medlineplus.gov/enlargedprostatebph.html ↵
- Rupp, T. J., & Leslie, S. W. (2023). Epididymitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK430814/ ↵
- Anand, S., Leslie, S. W., & Lotfollahzadeh, S. (2024). Epispadias. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK563180/ ↵
- National Institute of Diabetes and Digestive and Kidney Diseases. (2017). Definitions & facts for erectile dysfunction. https://www.niddk.nih.gov/health-information/urologic-diseases/erectile-dysfunction/definition-facts ↵
- Mayo Clinic. (2023). Hydrocele. https://www.mayoclinic.org/diseases-conditions/hydrocele/symptoms-causes/syc-20363969 ↵
- Donaire, A. E., & Mendez, M. D. (2023). Hypospadias. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK482122 ↵
- Donaire, A. E., & Mendez, M. D. (2023). Hypospadias. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK482122 ↵
- Mayo Clinic. (2022). Male infertility. https://www.mayoclinic.org/diseases-conditions/male-infertility/symptoms-causes/syc-20374773 ↵
- Mayo Clinic. (2022). Male infertility. https://www.mayoclinic.org/diseases-conditions/male-infertility/symptoms-causes/syc-20374773 ↵
- Mayo Clinic. (2022). Male infertility. https://www.mayoclinic.org/diseases-conditions/male-infertility/symptoms-causes/syc-20374773 ↵
- Bragg, B. N., Kong, E. L., & Leslie, S. W. (2023). Paraphimosis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK459233/ ↵
- National Institute of Diabetes and Digestive and Kidney Diseases. (2019). Penile curvature (Peyronie’s disease). https://www.niddk.nih.gov/health-information/urologic-diseases/penile-curvature-peyronies-disease ↵
- Bragg, B. N., Kong, E. L., & Leslie, S. W. (2023). Paraphimosis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK459233/ ↵
- National Cancer Institute. (2023). Prostate cancer treatment (PDQ) - Patient version. National Institutes of Health. https://www.cancer.gov/types/prostate/patient/prostate-treatment-pdq ↵
- National Cancer Institute. (2023). Prostate cancer treatment (PDQ) - Patient version. National Institutes of Health. https://www.cancer.gov/types/prostate/patient/prostate-treatment-pdq ↵
- National Cancer Institute. (2023). Prostate cancer treatment (PDQ) - Patient version. National Institutes of Health. https://www.cancer.gov/types/prostate/patient/prostate-treatment-pdq ↵
- Mayo Clinic. (2022). Prostatitis. https://www.mayoclinic.org/diseases-conditions/male-infertility/symptoms-causes/syc-20374773 ↵
- Mayo Clinic. (2022). Prostatitis. https://www.mayoclinic.org/diseases-conditions/male-infertility/symptoms-causes/syc-20374773 ↵
- Mayo Clinic. (2022). Spermatocele. https://www.mayoclinic.org/diseases-conditions/spermatocele/symptoms-causes/syc-20377829 ↵
- Mayo Clinic. (2022). Testicular torsion. https://www.mayoclinic.org/diseases-conditions/testicular-torsion/symptoms-causes/syc-20378270 ↵
- National Cancer Institute. (2023). Testicular cancer treatment (PDQ) - Patient version. National Institutes of Health. https://www.cancer.gov/types/testicular/patient/testicular-treatment-pdq ↵
- U.S. Preventive Services Task Force. (2011). Testicular cancer: Screening. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/testicular-cancer-screening ↵
A non-cancerous enlargement of the prostate gland that can cause urinary symptoms such as difficulty starting urination, a weak urine stream, or frequent urination.
A surgical procedure used to treat BPH. Small cuts are made in the prostate to widen the urethra and improve urine flow.
A surgical procedure to remove part of the prostate gland through the urethra. It is commonly used to treat BPH when medication is ineffective.
Inflammation of the epididymis, the tube that stores and carries sperm.
A congenital abnormality in which the urethra opens on the upper surface of the penis instead of at the tip.
The inability to achieve or maintain an erection sufficient for sexual intercourse.
An opening permits passage of fluid into the scrotum.
An enlargement of veins within the scrotum, similar to varicose veins, which can affect fertility.
Urethral placement on the underside of the penis rather than the tip.
A condition in which the foreskin becomes trapped behind the head of the penis and cannot be pulled forward. This can restrict blood flow and is a medical emergency.
A condition in which fibrous scar tissue develops inside the penis, causing curved and painful erections. It can affect sexual function and may require medical or surgical treatment.
A condition in which the foreskin is too tight to be pulled back over the head of the penis. It can cause pain and lead to infections. Treatment options include topical steroids or circumcision.
A protein produced by the prostate gland.
A management strategy where the patient and doctor monitor a condition over time without immediate intervention. This approach is often used for conditions like BPH or early-stage prostate cancer.
Inflammation of the prostate gland, which can be caused by bacterial infection or other factors.
A fluid-filled sac that develops in the epididymis, often containing dead sperm cells. It is usually painless and benign.
A medical emergency where the spermatic cord, which provides blood to the testicle, twists and cuts off the blood supply. This condition can cause severe pain and swelling and requires immediate surgery.
A type of cancer that occurs in the testicles, the male reproductive glands.
A surgical procedure to remove one or both testicles through an incision in the groin.

