11.2 Postpartum Physiological Adaptations
During the postpartum period, the changes that occurred during the 40 weeks of pregnancy gradually return to their prepregnant state. During the first few days after birth, fluid shifts occur, and many changes take place in body systems throughout the postpartum period. This section will review these physiological adaptations. Related nursing assessments and interventions are discussed in more detail in the “Applying the Nursing Process and Clinical Judgment Model to Postpartum Care” section.
Fluid Shifts
During pregnancy, many clients experience edema due to fluid retention. After delivery, excess extracellular fluid is pulled back into the venous system and eliminated via diuresis (increased urine output) and diaphoresis. Diaphoresis (excess sweating) is stimulated by decreasing levels of estrogen and progesterone and continues throughout lactation. The average amount of postpartum fluid loss is two liters over the first five to seven days after giving birth, effectively reducing edema. However, if the client received IV fluids during labor and delivery, edema may take more than a week to resolve. Nurses teach postpartum clients that excessive sweating is common, they will be urinating frequently, and their swelling should subside over several days.[1]
Cardiovascular and Respiratory Systems
Blood pressure and cardiac output are typically elevated for the first 48 hours postpartum. This is a result of increased extracellular fluid shifts into the intravascular system after birth. Increased intravascular fluid increases preload (filling pressure of the heart) and makes the heart work harder. As a result, preexisting cardiac conditions such as heart failure can worsen. The nurse should be aware if a postpartum client has preexisting cardiac conditions and monitor for worsening signs and symptoms such as increasing shortness of breath, tachycardia, or crackles in the lungs.[2] Pink-tinged frothy sputum is a sign of pulmonary edema, a serious complication that requires prompt provider notification and interventions such as diuretics. Left untreated, pulmonary edema can progress to respiratory failure, circulatory collapse, and, ultimately, death.
The respiratory system quickly returns to a prepregnant state after birth. As the fetus is no longer exerting pressure on the maternal diaphragm, the diaphragm has more room for expansion. Clients should feel less shortness of breath after delivery. New chest pain on inspiration, shortness of breath, tachypnea, or decreased oxygen saturation levels can indicate complications such as pulmonary edema (from fluid overload) or pulmonary emboli (from a deep vein thrombosis).
Reproductive System
After birth, the uterus, cervix, vagina, and perineum begin the process of returning to their prepregnant state.
Uterus
During the first 24 to 48 hours postpartum, the uterus experiences involution (shrinkage) to approximately the level of the umbilicus. The uterus then shrinks approximately one centimeter (cm) per day and reaches the suprapubic bone by Day 10. As involution occurs, the fundus (top of the uterus) is firm, mildline, and at the anticipated level of shrinkage. Complete involution of the uterus to the prepregnant size occurs over approximately six weeks. Subinvolution refers to the uterus not adequately returning to its prepregnant size.[3]
Fundal assessment is further discussed in the “Applying the Nursing Process and Clinical Judgment Model to Postpartum Care” section.
Involution is facilitated by postpartum uterine contractions that are stimulated by endogenous oxytocin release. Postpartum uterine contractions decrease the size of the uterus and also stop blood flow from spiral arteries in the uterine wall that perfused the placenta during pregnancy. These arteries are torn with detachment of the placenta from the uterine wall after birth and continue to attempt to perfuse the placenta after delivery. For this reason, it is crucial that these artery endings are compressed through uterine contractions and involution to stop the blood flow. Without adequate uterine contractions and involution, the risk of postpartum hemorrhage increases. Involution is inhibited by a full bladder, so if the nurse assesses the fundus and finds it boggy (soft), deviated from midline, or above the level of the umbilicus, a priority intervention is to have the client empty their bladder. Oxytocin is administered intravenously immediately after birth to facilitate involution and prevent postpartum hemorrhage. Oxytocin administration is further discussed in the “Postpartum Hemorrhage” subsection of the “Postpartum Complications” section.
The placental attachment site heals within six weeks by sloughing off old tissue as the endometrium generates new tissue. Placental fragments or membranes that are not sloughed off can cause endometritis (inflammation of the uterus generally caused by infection) and subinvolution of the uterus, which can result in postpartum hemorrhage.[4]
Lochia
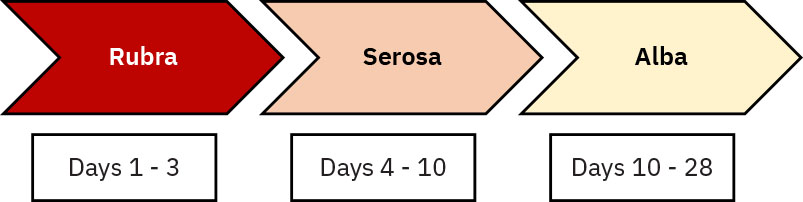
Vaginal bleeding that occurs during the postpartum period is called lochia. There are different stages of lochia called rubra, serosa, and alba. See Figure 11.2[5] for an illustration of these stages[6]:
- Lochia rubra: Lochia rubra occurs during the first one to three days postpartum and originates from the placental site. It is bright to dark red and consists of blood, cervical discharge, and uterine lining.
- Lochia serosa: As the placental site heals, the lochia changes to pinkish-brown and consists of white blood cells, cervical mucus, and discharge from the healing placental site. Lochia serosa lasts from postpartum Days 4 to 10.
- Lochia alba: Lochia alba is the final type of postpartum lochia and is yellow-white and consists of white blood cells, epithelial cells, and mucus. It occurs from approximately postpartum Days 10 to 28.
Cervical Changes
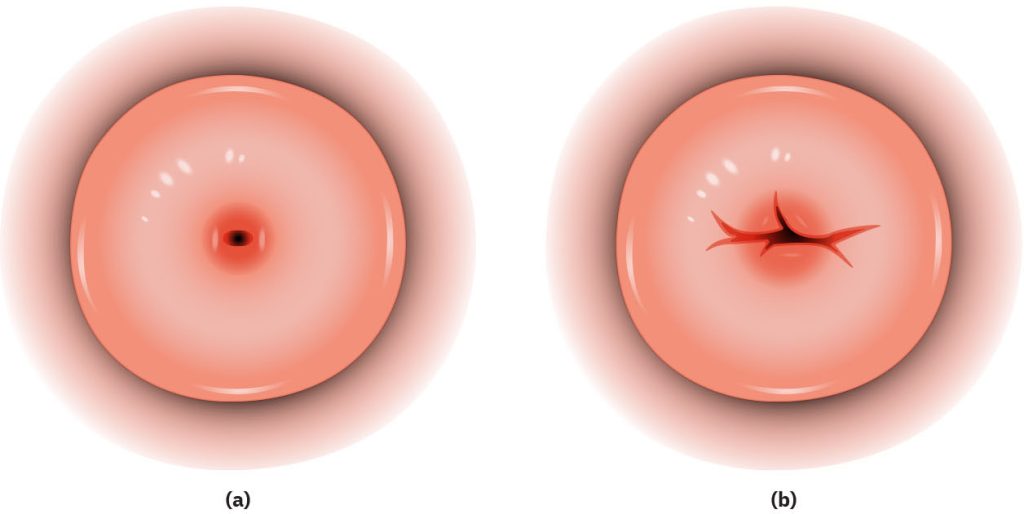
The cervix is bruised and remains slightly dilated and changed in shape if the woman experienced labor during vaginal birth or before an unplanned cesarean section. The cervical dilation gradually returns to less than one centimeter dilation after seven days. However, if the woman experienced a vaginal birth, the cervical os remains permanently changed in shape from a round pinhole to a transverse slit, as illustrated in Figure 11.3b.[7] After a planned cesarean birth, the cervix also goes through a recovery period and returns to its prepregnant status of a round pinhole shape as illustrated in Figure 11.3a.
Vagina, Perineum, and Pelvic Floor Muscles
The vagina is enlarged and often swollen after a vaginal birth. The perineum may have lacerations or an episiotomy repair. An episiotomy is an incision made in the perineum to allow more room for childbirth. Lacerations or episiotomies are typically repaired using absorbable sutures and take two to three weeks to heal.[8]
The pelvic floor muscles decrease in tone due to the stretching that occurs during labor to accommodate the fetus. This decreased tone often causes stress incontinence (urine leakage with increased abdominal pressure like coughing or sneezing). Nurses encourage pelvic floor muscle exercises called Kegel exercises to strengthen the pelvic floor and reduce incontinence.
Read more information about Kegel exercises in the “Interventions” subsection of “Applying the Nursing Process and Clinical Judgment Model to Postpartum Care” section.
Breast Changes and Lactation
The growth of the breasts during pregnancy may cause striae (stretch marks) and loss of elasticity of the skin. Superficial veins that occurred during pregnancy will fade in clients who do not breast feed but will continue to be seen in breastfeeding clients, especially during engorgement as breasts fill with milk and become firm. Darkening of the areola during pregnancy will fade over the first six weeks postpartum.[9]
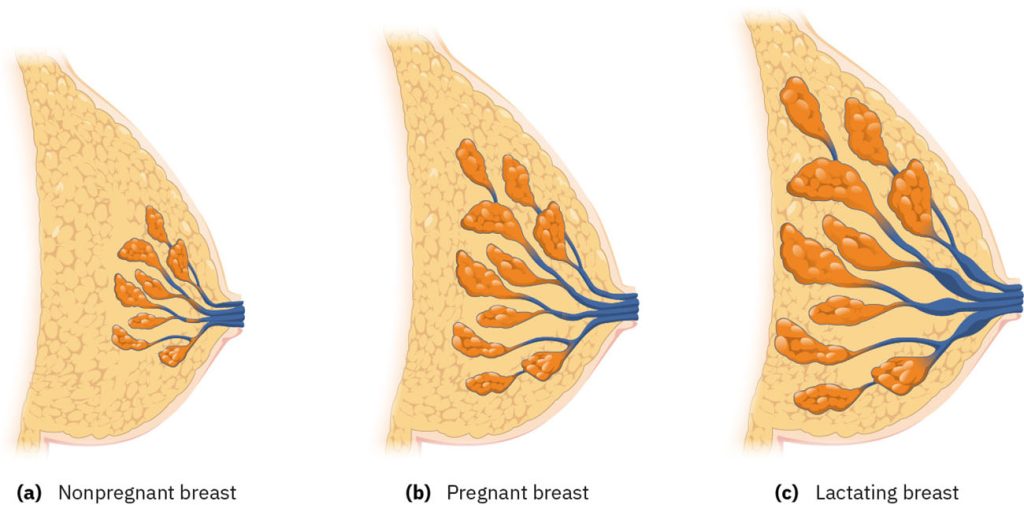
Lactogenesis
Lactogenesis is the physiologic process of developing the means to secrete milk. The first stage of lactogenesis occurs during pregnancy and results in the growth of the mammary lobes, ducts, and alveoli within the breast. After the birth of the placenta, estrogen and progesterone levels suddenly drop, which signal the anterior pituitary to produce prolactin to stimulate milk production. The lobes, ducts, and alveoli further increase in size within the lactating breast. See Figure 11.4[10] for an illustration comparing the nonpregnant breast, pregnant breast, and lactating breast.[11]
Colostrum is a thick, whitish-yellow, nutrient-dense initial milk that contains antibodies that build the newborn’s immune system. It is present in the breasts at the time of birth and secreted in small amounts during breastfeeding. At approximately postpartum Day 2 or 3, milk changes from colostrum to transitional milk, which is thinner and is secreted in greater amounts. At about two weeks postpartum, mature milk is produced, meeting the needs of the newborn and continually changing to meet the needs of the growing infant. Postpartum clients may have an elevated temperature and feel feverish as their milk comes in. During the first 12-24 hours after birth, temperatures may elevate higher than 38 C temporarily. However, a temperature of 38 C or higher during the first week postpartum should be reported to the health care provider as this could indicate infection. A fever occurring several weeks after breastfeeding starts is often due to mastitis, or inflammation and infection of the breast tissue, and should be reported to the health care provider for treatment. Postpartum women often experience an uncomfortable sensation of engorgement as their breasts fill with milk and become firm.[12],[13]
Letdown is a reflex caused by oxytocin release that contracts the alveoli and ejects milk from the breast. Letdown can be caused by heat, hearing a baby cry, thinking about the infant, or nipple stimulation by the infant. Milk production is stimulated by supply and demand. As the newborn empties the breast of milk, prolactin is released and the breasts are stimulated to produce more milk.[14]
Milk released during breastfeeding has different nutritional content from the beginning to the end of the session. Foremilk is released at the beginning of the breastfeeding session and is high in water and protein content but low in fat. Hindmilk is released later in the breastfeeding session and is high in fat and calories. The client should completely empty one breast prior to changing the infant to the other breast so the infant obtains both foremilk and hindmilk during each breastfeeding session.[15]
Urinary System
After childbirth, maternal urinary output may be as much as 3,000 mL in the first 24 hours, as extracellular fluid shifts back into the intravascular system. Clients are encouraged to urinate when they feel the urge to do so because postponing urination increases the risk for a urinary tract infection. However, clients may have difficulty emptying their bladder in the immediate postpartum period due to the normal physiologic accommodations made during vaginal birth, swelling, and trauma to the perineal area during vaginal birth, as well as the effects of epidural or spinal anesthesia. As a result, urinary retention may occur, resulting in overdistention of the bladder. An overdistended bladder interferes with uterine involution and increases the risk for postpartum hemorrhage. Nurses should promptly implement interventions such as intermittent catheterization to reduce urinary retention and facilitate involution of the uterus.
Assessing for bladder distension and implementing interventions for urinary retention are further discussed in the “Applying the Nursing Process and Clinical Judgment Model to Postpartum Care” section.
Musculoskeletal System
General muscle fatigue and body aches occur from the work of labor and delivery and typically resolve within a few days.
Some clients experience diastasis recti abdominis during pregnancy, where the muscles in the midline of the abdomen stretch to the point of separation. See Figure 11.5[16] for an illustration of diastasis recti abdominis.
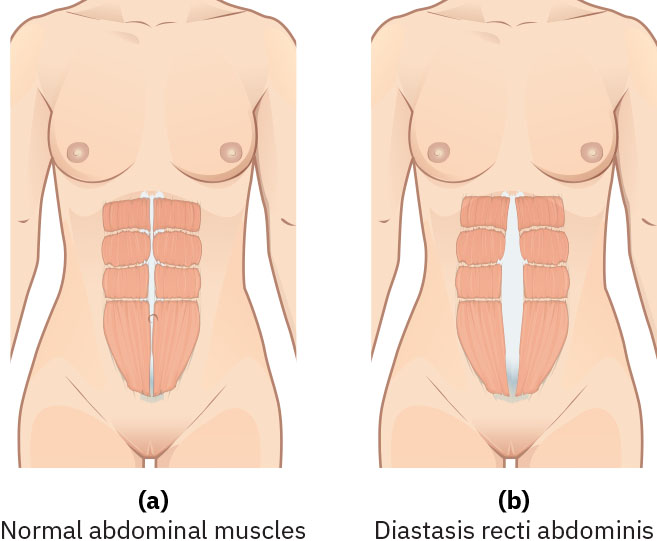
Clients at risk for diastasis recti abdominis are those who experienced cesarean birth or have a history of polyhydramnios, macrosomia, short intervals between pregnancies, multiple gestation, or multiple deliveries. As the client’s abdominal muscles begin to strengthen during the postpartum period, the separation of the diastasis recti muscles will decrease. Clients who experienced cesarean birth should be instructed to roll to their side while getting out of bed to avoid using the abdominal muscles. If diastasis recti abdominis has not healed by six weeks postpartum (meaning the diastasis is still more than two centimeters in width), the client should consult their health care provider for possible referral to physical therapy.[17]
Other musculoskeletal changes during pregnancy can cause pelvic instability and pain. During pregnancy, increased estrogen, progesterone, and relaxin levels cause relaxation and softening of the pelvic bones, muscles, and ligaments. Relaxin allows the pelvic bones to separate and increases the diameter of the pelvis to accommodate fetal descent. Relaxin also causes separation of the symphysis pubis, and the growing uterus and fetus cause alterations in center of gravity. These hormones, combined with a shifted center of gravity, cause the lumbar vertebrae to separate slightly, which often results in lordosis (curving in of the lumbar spine). After delivery of the placenta, relaxin levels gradually decrease, and the pelvic bones return to their prepregnant state. Lordosis generally resolves within several months.[18] Pelvic floor exercises and abdominal strength-building exercises are helpful to improve pelvic stability.
View a supplementary YouTube video[19] on healing the diastasis muscles: Heal Diastasis Recti FAST – Physiotherapy Guide to FIX & FLATTEN Your BELLY.
Integumentary System
Skin changes that were caused by pregnancy hormones gradually diminish, such as linea nigra (a dark vertical line on the abdomen) and other hyperpigmentation. Striae, also known as stretch marks, may occur on the skin during pregnancy and become less visible over time, though they don’t completely resolve. Figure 11.6[20] shows an example of linea nigra and striae on a pregnant abdomen. Striae in light-skinned persons are pink-purple during pregnancy and fade to a silver color. People with darker skin have striae that appear darker than their skin tone during pregnancy and fade over time.[21]

Gastrointestinal System
As the gastrointestinal system regains motility after the birth process, some postpartum clients initially experience nausea and vomiting. The nurse can encourage small, bland meals or administer prescribed antiemetics to reduce nausea and vomiting.[22]
If a client experienced a cesarean birth, peristalsis is slowed due to abdominal surgery, as well as the effects of anesthesia. Diet orders are typically progressed as peristalsis returns, evidenced by normoactive bowel sounds and the passage of flatus.[23]
After childbirth, factors such as decreased peristalsis, dehydration, decreased food intake during labor, and side effects of analgesics and anesthetics commonly cause constipation. Furthermore, clients may be afraid of experiencing perineal pain or tearing perineal sutures during bowel movements, resulting in ignoring the urge to defecate. Hemorrhoids may also be present, causing pain during defecation. To promote the easy passage of soft stools and reduce straining, nurses encourage early ambulation, increased fluid intake, and a high-fiber diet. Prescribed stool softeners and laxatives may also be administered as indicated.[24]
Nutrition and Weight Loss
Weight loss of approximately 10 to 15 pounds occurs immediately after the delivery of the infant, placenta, and amniotic fluid. Depending on the amount of edema experienced during pregnancy and labor, some clients lose an additional five or more pounds of extracellular fluid over the first few postpartum days. Loss of the remaining weight that was gained during pregnancy is a gradual process based on caloric intake and energy expenditure that varies across individuals. Nurses teach postpartum clients about healthy diet choices based on MyPlate recommendations. Recommendations include fruits and vegetables for vitamin and fiber intake, whole grains for energy, lean proteins to rebuild muscle and heal tissue, dairy products for calcium and bone health, and a small amount of healthy fat for producing breast milk. The Centers for Disease Control and Prevention (CDC) recommends breastfeeding mothers eat 340 to 400 more kilocalories (kcal) per day than the amount they consumed before pregnancy. This means approximately 2,000 to 2,800 kcal per day for breastfeeding women versus 1,600 to 2,400 kcal per day for moderately active women who are not pregnant and not breastfeeding. The number of additional calories needed for a breastfeeding woman is affected by their age, body mass index, activity level, and whether they are exclusively breastfeeding or both breastfeeding and formula feeding.[25],[26]
Review MyPlate nutrition recommendations in the “Dietary Recommendations According to Age and Developmental Level” section of the “Healthy Diets” chapter.
Nervous System
If a client received spinal or epidural anesthesia, transitory neurologic changes such as dizziness and numbness in the lower extremities may occur. A common complication of spinal or epidural anesthesia is a spinal headache due to the dura mater being punctured when the epidural or spinal needle was inserted. Puncture of the dura mater causes leakage of cerebrospinal fluid, resulting in decreased amount of cerebrospinal fluid around the brain. The decreased fluid causes a spinal headache, a severe headache that worsens when the person sits in an upright position. If the nurse suspects a spinal headache, the client is assisted to a lying position and the anesthesia provider is notified to further address the problem.[27]
Headaches that are persistent despite position changes may indicate postpartum preeclampsia. The nurse assesses for other signs of preeclampsia, including elevated blood pressure, blurred vision, epigastric pain, photophobia, and increased deep tendon reflexes. A client with preeclampsia is at risk for an eclamptic seizure for up to six weeks after birth.[28]
Rapid changes in estrogen, progesterone, and prolactin levels that occur immediately after birth can contribute to postpartum depression. Postpartum depression (PPD) includes feelings of extreme sadness, anxiety, and exhaustion that may make it difficult for new mothers to complete daily care activities for themselves and/or their babies. Untreated postpartum depression is not only a problem for the mother’s health and quality of life but can also affect the well-being of the newborn.
Read more about postpartum depression and preeclampsia in the “Postpartum Complications” section.
Hematological System
The normal reference ranges for several lab values change during the antepartum and postpartum periods. See Table 11.1 for a comparison of prepregnancy, antepartum, and postpartum normal reference values. Keep in mind that normal reference ranges fluctuate slightly across facilities.
Table 11.1. Normal Reference Ranges for Prepregnancy, Antepartum, and Postpartum[29]
| Lab Value | Prepregnant | Antepartum | Postpartum (24 hours) |
|---|---|---|---|
| Hemoglobin | 12–16 g/dL | 9.5–15 g/dL | 8–13.7 g/dL |
| Hematocrit | 35–44 g/dL | 28–41 g/dL | 24.5–40.8 g/dL |
| WBC | 4–10 × 109/L | 6–16 × 109/L | 7–21 × 109/L |
| Platelets | 150–400 × 109/L | 145–400 × 109/L | 67–251 × 109/L |
| Fibrinogen | 1.5–4.0 g/dL | 2.38–5.9 g/dL | 2.5 g/dL |
| Ferritin | 10–150 ng/mL | 16–24 ng/mL | 32–50 ng/mL |
Postpartum anemia (PPA) affects 50-80% of postpartum clients due to blood loss during delivery, as well as preexisting iron deficiency. Blood loss of 500 mL during vaginal delivery commonly results in a one-gram drop in hemoglobin, and blood loss of 1,000 mL during cesarean birth commonly results in a two-gram drop in hemoglobin. There is a lack of consensus regarding the definition of PPA, but most guidelines define PPA as a hemoglobin less than 10 g/dL measured at least 48 hours after delivery.[30] Although maternal iron stores eventually replenish after delivery, the effects of PPA can impact maternal health and well-being with symptoms of fatigue, dizziness, impaired concentration, breathlessness, and palpitations. Research also indicates that PPA increases the risk of depression, and the administration of intravenous iron can significantly reduce depression scores.[31] Nurses monitor hemoglobin and hematocrit values, notify the provider of abnormal values and symptoms of anemia, and educate clients about taking prescribed supplemental iron and selecting foods high in iron.[32],[33]
Review information about anemia in the “Anemia” and “Iron-Deficiency Anemia” sections of the “Hematology Alterations” chapter of Open RN Health Alterations.
During labor, the white blood cell (WBC) count may increase up to 20-30 × 109/L and remain elevated for several days due to the stress of labor, as well as inflammation that occurs during postpartum healing. However, WBCs should return to prepregnancy values after seven days. Nurses monitor WBC results, assess for signs of infection, and notify the health care provider of abnormal findings.[34]
Platelet counts typically decrease during pregnancy, with the lowest count occurring on the first day after delivery and recovering to prepregnant levels within two to seven days after delivery. If a client had low platelet and coagulation factor XIII levels before labor, there is increased risk of postpartum hemorrhage (PPH). A platelet count below 100,000/µL on the first day after delivery can indicate complications such as preeclampsia or disseminated intravascular coagulation (DIC).[35],[36],[37]
Plasma fibrinogen may be elevated for one week following childbirth to facilitate clotting and prevent excessive bleeding. However, this elevated level also increases the client’s risk for developing deep vein thrombosis (DVT). The nurse routinely assesses for signs of DVT such as unilateral extremity edema, redness, and warmth.[38] If a DVT is suspected, the nurse avoids massaging the extremity and removes sequential compression devices while promptly notifying the health care provider for further evaluation and treatment. The client’s respiratory status is closely monitored for signs of the development of a pulmonary embolism (PE).
Read more about DVT in the “Deep Vein Thrombosis” section of the “Cardiovascular Alterations” chapter of Open RN Health Alterations.
Read more about preeclampsia and DIC in the “Complications Associated With Labor” section of the “Labor and Delivery Care” chapter.
View a supplementary YouTube video[39] on postpartum physiological changes: How The Body Changes After Pregnancy | Postpartum Physiologic Changes.
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- “9adf88740e89b2e70c840cf900e045b8c2c16019” by Rice University/OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- “f62410c80227d53b751569ceded7026e95245583”by Rice University/OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- “2706d333a20d02f4e3c548f3ae0f2fcb9d696129” by Rice University/OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- United States Department of Agriculture. WIC Breastfeeding Support. (n.d.). The phases of breastmilk. https://wicbreastfeeding.fns.usda.gov/phases-breast-milk ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- “1d7f7f7997de7edb09b10362ea40ded356aeff6c” by Rice University/OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Kenway, M. (2021, April 26). Heal diastasis recti FAST - Physiotherapy guide to fix & flatten your belly [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=qyhdvWQoRME ↵
- This image is a derivative of “pexels-directorvinny-10690897” by directorvinny studios, Pexels.com is licensed under CC0 ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Centers for Disease Control and Prevention. (2024). Maternal diet and breastfeeding. https://www.cdc.gov/breastfeeding-special-circumstances/ ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Neef, V., Choorapoikayil, S., Hof, L., Meybohm, P., & Zacharowski, K. (2024). Current concepts in postpartum anemia management. Current Opinion in Anaesthesiology, 37(3), 234–238. https://doi.org/10.1097/ACO.0000000000001338. https://pmc.ncbi.nlm.nih.gov/articles/PMC11062600/ ↵
- Neef, V., Choorapoikayil, S., Hof, L., Meybohm, P., & Zacharowski, K. (2024). Current concepts in postpartum anemia management. Current Opinion in Anaesthesiology, 37(3), 234–238. https://pmc.ncbi.nlm.nih.gov/articles/PMC11062600/ ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Neef, V., Choorapoikayil, S., Hof, L., Meybohm, P., & Zacharowski, K. (2024). Current concepts in postpartum anemia management. Current Opinion in Anaesthesiology, 37(3), 234–238. https://pmc.ncbi.nlm.nih.gov/articles/PMC11062600/ ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Reese, J. A., Peck, J. D., McIntosh, J. J., Vesely, S. K., & George, J. N. (2017). Platelet counts in women with normal pregnancies: A systematic review. American Journal of Hematology, 92(11), 1224–1232. https://doi.org/10.1002/ajh.24829. ↵
- Beveridge, C. (2023). Blood platelet levels and postpartum hemorrhage risk. The Waiting Room. https://thewaitingroom.karger.com/knowledge-transfer/blood-platelet-levels-and-postpartum-hemorrhage-risk ↵
- Dahlstrøm, B. L., & Nesheim, B. I. (1994). Postpartum platelet count in maternal blood. Acta Obstetricia et Gynecologica Scandinavica, 73(9), 695–697. https://pubmed.ncbi.nlm.nih.gov/7976243/ ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Lecturio Nursing. (2022, April 25). How the body changes after pregnancy | Postpartum physiologic changes [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=Q46PlTpWBTc ↵
Increased urine output.
Excess sweating.
Filling pressure of the heart.
Shrinkage.
The uterus not adequately returning to its prepregnant size.
Inflammation of the inner lining of the uterus (endometrium), often caused by infection. It can occur after childbirth, miscarriage.
Maternal postpartum vaginal discharge.
Occurs during the first one to three days postpartum and originates from the placental site. It is bright to dark red and consists of blood, cervical discharge, and uterine lining.
Lochia from postpartum days 4 to 10 which changes to pinkish-brown and consists of white blood cells, cervical mucus, and discharge from the healing placental site.
The final type of postpartum lochia and is yellow-white and consists of white blood cells, epithelial cells, and mucus. It occurs from approximately postpartum days 10 to 28.
A surgical procedure to deliver a baby through incisions in the mother's abdomen and uterus.
Performed by the health care provider during the second stage of labor to quickly facilitate vaginal delivery or to prevent large, irregular tears of the vaginal wall.
Urine leakage with increased abdominal pressure like coughing or sneezing.
Pelvic floor muscle exercises.
Stretch marks.
Breasts fill with milk and become firm.
The physiologic process of developing the means to secrete milk.
An antibody-rich secretion that helps develop the newborn’s immunity.
A reflex caused by oxytocin release that contracts the alveoli and ejects milk from the breast.
Released at the beginning of the breastfeeding session and is high in water and protein content but low in fat.
Released later in the breastfeeding session and is high in fat and calories.
The natural process of the uterus returning to its pre-pregnancy state after giving birth.
The muscles in the midline of the abdomen stretch to the point of separation.
Inward curvature of the lumbar spine.
A vertical line of increased pigmentation, which starts at the pubic hair line, passes through the umbilicus, and goes up to the xiphoid process.
A severe headache that worsens when the person sits in an upright position.
Feelings of extreme sadness, anxiety, and exhaustion that may make it difficult for new mothers to complete daily care activities for themselves and/or for their babies.
Affects 50-80% of postpartum clients due to blood loss during delivery, as well as preexisting iron deficiency.

