4.1 Suctioning
Airway suctioning is routinely done in most care settings, including acute care, sub-acute care, long-term care, and home settings. Suctioning is performed when the patient is unable to effectively move secretions from the respiratory tract or the oropharynx. (See Figure 19.[1]) A respiratory therapist should be skilled and knowledgeable about all aspects of airway suctioning.
Airways suctioning is indicated for multiple reasons. Most commonly, suctioning is done for the removal of secretions from the respiratory tract, but sometimes also for the removal of blood or other materials like meconium in neonates. Airway suctioning is also performed for diagnostic purposes. For example, airway secretions may be sent for microbiological and histological review. Additionally, suctioning is performed to maintain the patency of artificial airways such as an endotracheal tube or a tracheostomy tube.

Multiple studies have shown that airway suctioning should be done as needed or based on clinical parameters, including pulse oximetry levels, respiratory rate, or visible secretions in the airway. Optimal suctioning helps reduce airway obstruction and the incidence of atelectasis, which leads to hypoxemia and impaired gas exchange.
Oral and Nasotracheal Suctioning (Open Suctioning)
Suctioning via the oropharyngeal (mouth) and nasopharyngeal (nasal) routes is performed to remove accumulated saliva, pulmonary secretions, blood, vomitus, and other foreign material from these areas that cannot be removed by the patient’s spontaneous cough or other less invasive procedures. Nasal and pharyngeal suctioning are performed in a wide variety of settings, including critical care units, emergency departments, inpatient acute care, skilled nursing facility care, home care, and outpatient/ambulatory care. Suctioning is indicated when the patient is unable to clear secretions and/or when there is audible or visible evidence of secretions in the large/central airways that persist in spite of the patient’s best cough effort.
For oropharyngeal suctioning, a device called a Yankauer suction tip is typically used for suctioning mouth secretions (see Figure 20[2]). A Yankauer device is rigid and has several holes for suctioning secretions that are commonly thick and difficult for the patient to clear.

Nasopharyngeal and nasotracheal suctioning removes secretions from the nasal cavity, pharynx, and throat by inserting a flexible, soft suction catheter through the nares. This type of suctioning is performed when oral suctioning with a Yankauer is ineffective. For nasopharyngeal/nasotracheal suctioning, it is important to use a sterile open suction catheter and use sterile technique when handling the catheter (see Figure 21[3]). When performing nasal suctioning, have the patient lean their head backwards to open the airway. This helps guide the catheter toward the trachea rather than the esophagus.
View the following supplementary YouTube video[4] that demonstrates the technique for nasopharyngeal/nasotracheal suctioning: Performing Nasotracheal and Nasopharyngeal Suctioning
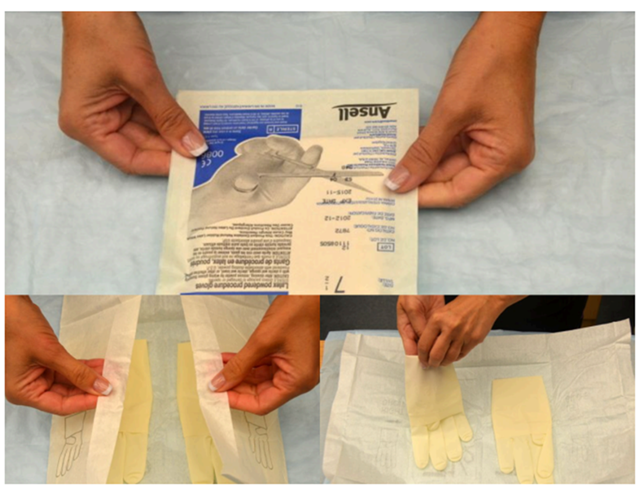
Sterile Technique for Open and Nasotracheal Suctioning
Sterile technique (also called surgical asepsis) seeks to eliminate every potential microorganism in and around a sterile field while also maintaining objects as free from microorganisms as possible. It is the standard of care for open suctioning. Sterile technique for open suctioning requires a combination of meticulous handwashing and donning sterile gloves (see Figure 22[5]).
Closed Suctioning
Closed suction catheters are preferable with ventilated patients to reduce the occurrence of airway collapse that may occur when a patient is disconnected from the ventilator. Closed suctioning is considered safer and is associated with fewer adverse events. In-line suctioning, as the name implies, includes a suction catheter that is attached as a part of the ventilator circuit connected to the patient.
Superficial suctioning implies going down with the suction catheter only up to the end of the artificial airway (endotracheal or tracheostomy tube), whereas deep suctioning implies going down with the catheter until resistance is met, which can theoretically be until the carina or primary bronchi are reached. Superficial suctioning is the most advisable to avoid mucosal injury and trauma.
View the following supplementary YouTube video[6] that demonstrates the proper technique for closed suctioning and artificial airway: Suctioning the endotracheal tube – medical animation
Procedure
The patient should be educated about the procedure (if awake and interactive) and the possibility of discomfort. Ensure preoxygenation with 100% FiO2 was done with adequate pulse oximetry measurements. Preoxygenation is required because an airway suctioning procedure may be associated with significant hypoxemia. Suctioning of the lower airways should be done in a sterile manner with single-use gloves and suction catheters to prevent contamination and secondary infection.
After preparation with appropriate equipment at the bedside, vitals should be monitored continuously, including heart rate, oxygen saturation, and intracranial pressure if transduced. Once the patient is preoxygenated, the patient should be suctioned with the appropriately sized equipment for their airway. The catheter should be introduced to a depth no more than the tip of the artificial airway to prevent trauma and bleeding from airway mucosa. Suction pressure should be set at -100 to -120 mmHG for adults, -80 to -100 mmHG for children, and -60 to -80 mmHG for infants. The catheter size used for suction should be less than 50% of the internal diameter of the endotracheal tube.
Each pass should be less than 15 seconds in duration, and the patient should be allowed to recover for at least 30 seconds to 1 minute between suction passes. Routine use of saline down the endotracheal tube is not recommended while suctioning.
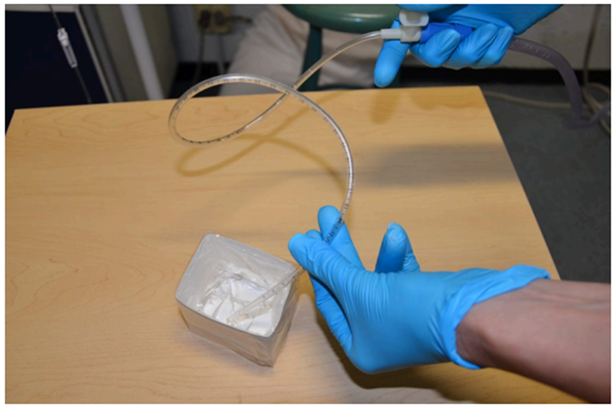
Specimen Collection
A variety of specimen collectors (commonly called Lukens traps) are available. They are packaged as sterile so that no contamination of the sputum sample occurs with nonpatient organisms. A properly working specimen collection system provides a vacuum to the tip of the suction catheter when the thumb control valve or mouthpiece is sealed, and vacuum is applied.
View the following supplementary YouTube video[7] that shows how to collect as sputum sample: Collecting a Suction Sample
- "DSC_0192" by BCcampus is licensed under CC BY 4.0. Access for free at https://opentextbc.ca/clinicalskills/ ↵
- "Yankauer_Suction_Tip" by Thomasrive is licensed under CC BY-SA 3.0 ↵
- "DSC_0210" by BCcampus is licensed under CC BY 4.0. Access for free at https://opentextbc.ca/clinicalskills/ ↵
- Ashraf Z Qotmosh. (2020, June 23). Performing Nasotracheal and Nasopharyngeal Suctioning [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=AjVw7HZ1YCk ↵
- This image is derivative of "Book-pictures-2015-199-001", "Book-pictures-2015-215", and "Book-pictures-2015-220" by BcCampus is licensed under CC BY 4.0. Access for free at https://opentextbc.ca/clinicalskills/ ↵
- Amerra Medical. (2022, May 7). Suctioning the endotracheal tube - medical animation [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=pN6-EYoeh3g ↵
- Pediatric Home Service. (2018, August 30). Collecting a Suction Sample [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=5pM5ZYngxnk ↵

