4.1 MDI/DPI and SVN
The lungs have a large surface area with an increased amount of blood flow, so medications are easily absorbed. Medications inhaled from the mouth into the lungs can be administered using a metered-dose inhaler (MDI), a dry powder inhaler (DPI), or a small-volume nebulizer (SVN).
Metered-Dose Inhaler (MDI)
A metered-dose inhaler (MDI) provides a mist of medication that is inhaled through the mouth into the lungs (see Figure 23[1]). However, during inhalation from an MDI, small medication particles can get trapped on the tongue or aerosolize into the air and not make it into the lungs, so a spacer is optimally used for full absorption of medication.

Dry Powder Inhaler (DPI)
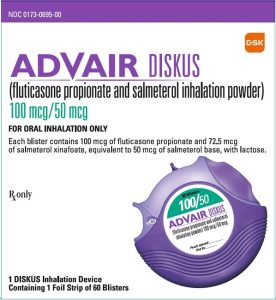
A dry powder inhaler (DPI) is medication provided in a powder form that is inhaled from the mouth into the lungs using a quick breath to activate the medication and move it into the lungs from the inhaler (see Figures 24[2] and 25[3]).

Small-Volume Nebulizer (SVN)
Since the development of the field of respiratory therapy, the small-volume nebulizer (SVN) has been the primary way that medications are delivered to a patient’s lungs. The SVN requires a pneumatic gas source that runs 6–8 L/min. Some SVNs are breath-actuated and have a more complex design. There are simpler versions, referred to as high-humidity nebulizers (HHN), which run continuously and have a lower percentage of the medication that deposits into the lung compared to the breath actuated systems. There are also vibrating mesh nebulizers that do not add additional inspiratory flow to the patient and studies have shown greater medication deposition when using these types of nebulizers.
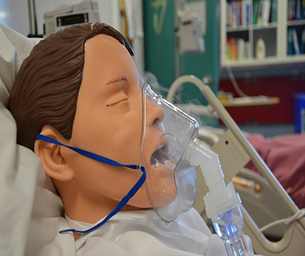
Hand-held, small-volume nebulizers provide a fine mist using oxygen or compressed air to transport the liquid medication (see Figure 26[4]) from the nebulizer cup into the mouth and into the lungs as the patient breathes normally.[5]

MDI/DPI and nebulized medications are delivered to the lungs by inhalation. Respiratory therapists are the primary health care providers responsible for delivery of inhaled medication. Deposition of the medication is determined by a number of factors such as the type of device used, the patient, the drug delivered, and the patient’s disease state. One of the major factors affecting the deposition of inhaled aerosolized medications in the lungs is particle size.
View the following supplementary YouTube video[6] that explains particle deposition in detail: Particle Deposition in Respiratory Tract
Medication Administration
Before administering an inhaler, the respiratory therapist should perform hand hygiene and check medication rights as with all medication. If the patient is self-administering the medication, advise them to wash their hands. The patient’s respiratory system should be assessed and documented before and after the administration of inhaled medications, including assessment of respiratory rate, pulse oximetry, heart rate, and lung sounds.
When administering an MDI, the respiratory therapist should shake the inhaler and add a spacer or a valved holding chamber onto the mouthpiece. The use of spacers with MDIs is considered best practice because they help ensure the medication is inhaled rather than inadvertently placed in the mouth. They also reduce waste by ensuring the patient receives the full amount of medication. The patient should be instructed to exhale while placing the spacer’s mouthpiece into their mouth. The inhaler is depressed to move the aerosolized medication into the spacer, and the patient should breathe in normally through the spacer to receive the medication. If a spacer is not available, the patient should exhale and hold the inhaler mouthpiece about 1–2 inches away from their mouth to help ensure the medication is inhaled via the larynx and not sprayed onto the posterior pharynx. As the inhaler is depressed, the patient should inhale the medication deeply through their mouth and into their lungs. The patient should be advised to hold their breath for 5–10 seconds after inhaling the medication and then exhale through pursed lips. The patient should wait for 1–5 minutes between each puff of medication. When administering inhaled corticosteroids via MDI, the patient should rinse their mouth with water afterwards to prevent fungal infection.[7]
When using a DPI, the respiratory therapist should load the medication into the devices as required and then activate the inhaler per the manufacturer’s guidelines. The patient should be instructed to hold the device level once the dose has been loaded and activated. Then, the patient should exhale and then place their lips around the mouthpiece and inhale strongly and deeply. After they have inhaled, they should hold their breath for 10 seconds or as long as comfortable and then exhale through pursed lips. The patient should wait 1–5 minutes between puffs of medication. If the DPI contains a corticosteroid medication, the patient should gargle and rinse with tap water to decrease the risk of developing a fungal infection.
When using an SVN, the respiratory therapist pours the liquid medication (using sterile technique – without touching the inside of the cup) into the medication cup of the nebulizer. When possible, the patient should be sitting or positioned in high-Fowler’s position to enhance deep breaths and absorption of medication. The bottom end of the tubing is attached to the oxygen flowmeter, and the flow rate should be set between 6 to 10 L/min, based on the manufacturer’s recommendations. The top end of the tubing is connected to either a nebulizer mask or mouthpiece. The patient should be instructed to inhale slowly through the device into their mouth and hold each breath for a slight pause before exhaling. (See Figure 27.[8]) Remain with the patient during the nebulizer treatment, which usually takes about 8–10 minutes. After treatment, the patient should be encouraged to cough and perform oral care. The patient’s respiratory system should be reevaluated after the administration of inhaled medications to document therapeutic effects, as well as to monitor for adverse effects.[9]
- RESIZED+SERIALIZED+1202-1.jpg” courtesy of the U.S.National Library of Medicine is in the Public Domain. ↵
- “advair-diskus-spl-graphic-16.jpg” courtesy of the U.S.National Library of Medicine in the Public Domain. ↵
- “breo-ellipta-for-article_765295.jpg” courtesy of EMPR.com. This image is included on the basis of Fair Use. ↵
- “Ipratropium_Bromide_(1).JPG” by Intropin is licensed under CC BY-SA 3.0 ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2023). Nursing skills 2e. Open RN. https://wtcs.pressbooks.pub/nursingskills/ ↵
- METPHAST. (2018, November 19). Particle deposition in respiratory tract [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=6ih3F1S9MZw ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2023). Nursing skills 2e. Open RN. https://wtcs.pressbooks.pub/nursingskills/ ↵
- “Administering_inhaled_medication.jpg” by British Columbia Institute of Technology (BCIT) is licensed under CC BY 4.0 ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2023). Nursing skills 2e. Open RN. https://wtcs.pressbooks.pub/nursingskills/ ↵

