2.1 Airway Adjuncts
To become the expert at placing and utilizing nasopharyngeal (NPA) and oropharyngeal (OPA) airways, you must first understand the anatomy and physiology of the upper airway.
The pharynx is a tube that is formed by skeletal muscle and lined by a mucous membrane that is continuous with that of the nasal cavities. The pharynx is divided into three major regions: the nasopharynx, the oropharynx, and the laryngopharynx (see Figure 5[1]).
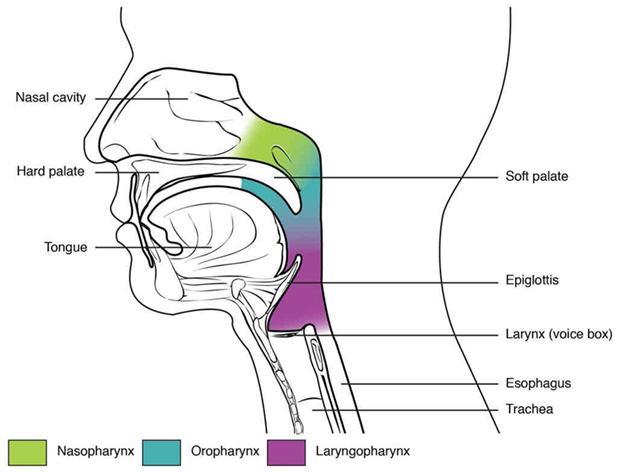
The uppermost nasopharynx sits directly posterior to the nasal cavity, and it serves only as an airway. The nasopharynx has two openings on the lateral walls. These openings are the auditory (eustachian or pharyngotympanic) tubes, which connect the nasopharynx to each middle ear cavity. These connections are why colds often lead to ear infections. As the pharynx descends behind the oral cavity, it becomes the oropharynx, which serves as a passageway for both air and food. The uvula is a small bulbous, teardrop-shaped structure located at the apex of the soft palate that partially separates the oral cavity from this region. Both the uvula and soft palate move like a pendulum during swallowing, swinging upward to close off the nasopharynx to prevent ingested materials from entering into the nasal cavity. The most inferior portion of the pharynx is the laryngopharynx, which is located posterior to the larynx. It continues the route for ingested material and air until its inferior end, where the digestive and respiratory systems diverge. The stratified squamous epithelium of the oropharynx is continuous with the laryngopharynx. Anteriorly, the laryngopharynx opens into the larynx, whereas posteriorly, it enters the esophagus.
Airway adjuncts are devices used to maintain an open upper airway or relieve an obstruction. They are often used when mask ventilation is difficult. Common airway adjuncts, such as nasopharyngeal airways (NPA), laryngeal mask airways (LMA), and oropharyngeal airways (OPA), are often used in emergency situations, and a respiratory therapist needs to be able to quickly assess the patient and insert those airways.
Oropharyngeal Airway
An oropharyngeal airway (OPA) is a short-term, easily inserted airway management device extending from the lips to the pharynx and prevents the base of the tongue from falling back and occluding the airway. A flange at the outer opening prevents the device from being inserted or pushed too far into the airway. See Figure 6[2] for an image of an oropharyngeal airway.

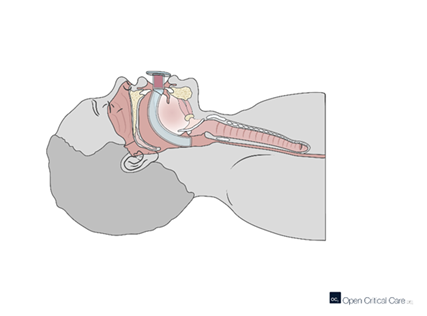
To properly insert an OPA, first select the proper size by measuring the airway from the corner of the lip to the angle of the jaw to ensure proper length. Open the patient’s mouth and insert the airway with the tip pointing toward the roof of the mouth. Observe the airway passing the uvula and rotate the OPA 180 degrees. (See Figure 7.[3])
Nasopharyngeal Airway (NPA)
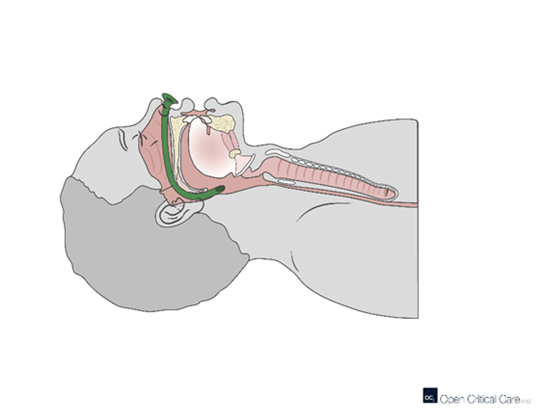
A nasopharyngeal airway (NPA) is a soft, anatomically designed airway adjunct that is inserted into the nasal passageway to provide airway patency (see Figure 8[4]). The flared distal end prevents the device from becoming lost within the nares. The NPA has advantages over the oropharyngeal airway as it can be used in patients with intact gag reflex, trismus, and oral trauma.

To properly insert an NPA, first select the proper size by measuring the airway from the tip of the nose to the earlobe. The outside diameter of the airway should be equal to the inside diameter of the patient’s internal nares. Lubricate the airway with a water-soluble gel and insert it into the patient’s nostril. The flanged end should rest against the nose, and the distal tip should rest behind the uvula. (See Figure 9.[5])
Laryngeal Mask Airway (LMA)
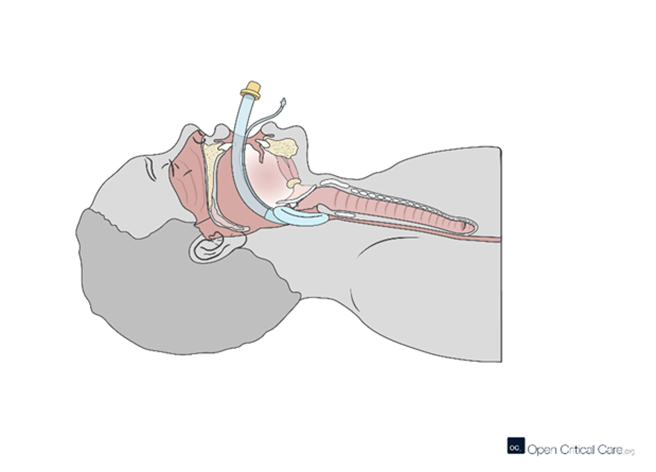
A laryngeal mask airway (LMA) is a supraglottic airway device that sits abutting the larynx, above the vocal cords. It is typically used as an alternative to endotracheal airways in short or low-risk anesthetic cases and can also be used in prehospital and cardiac arrest settings to achieve a more secure airway without endotracheal intubation.
An LMA is inserted through the mouth and into the pharynx after being lubricated with a water-soluble gel. The device is advanced until resistance is met. Then, the mask of the device is inflated, providing a low-pressure seal around the laryngeal inlet. The posterior of the tube is marked with a black line, which should be seen midline against the patient’s upper lip when the airway is placed properly. (See Figure 10.[6])
- “2305_Divisions_of_the_Pharynx.jpg” by OpenStax College is licensed under CC BY 3.0 ↵
- “Oropharyngeal_Airways” by Hospital is licensed under CC BY-SA 3.0 ↵
- “Sagittal-Cross-Section-w-Oral-Airway-87u1xb.png” by Open Critical Care is licensed under CC BY 4.0 ↵
- “Nasopharyngeal_Airway_2” by ICUnurses is licensed under CC BY-SA 4.0 ↵
- “Sagittal-cross-section-view-of-nasopharyngeal-airway-placement.png” by Open Critical Care is licensed under CC BY 4.0 ↵
- “Sagittal-Cross-Section-LMA-091122-0g4du1-1280x989” by Open Critical Care is licensed under CC BY 4.0 ↵

