1.1 The Profession, Organizations, and Legal Considerations
Respiratory therapists are members of a multidisciplinary health care team. Respiratory therapists are specialized clinicians who are involved in all aspects of respiratory care including managing oxygen therapy; drawing arterial blood gases; managing patients on specialized oxygenation devices such as mechanical ventilators and non-invasive machines; administering respiratory medications like inhalers and nebulizers; intubating patients; assisting with bronchoscopy and other respiratory-related diagnostic tests; performing pulmonary hygiene measures like chest physiotherapy; and serving an integral role during rapid responses, cardiac and respiratory arrests, traumas, and codes.[1]
A Brief Overview of Respiratory Care
Respiratory care, also known as respiratory therapy, has been defined as the health care discipline that specializes in the promotion of optimal cardiopulmonary function and health. Respiratory therapists (RTs) apply scientific principles to prevent, identify, and treat acute or chronic dysfunction of the cardiopulmonary system. Respiratory care includes the assessment, treatment, management, control, diagnostic evaluation, education, and care of patients with deficiencies and abnormalities of the cardiopulmonary system. Respiratory care is increasingly involved in the prevention of respiratory disease, the management of patients with chronic respiratory disease, and the promotion of health and wellness.
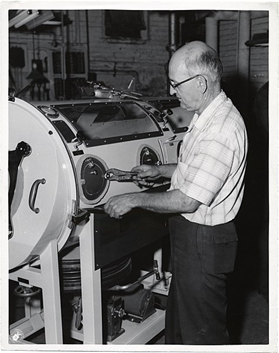
The role of respiratory therapists has significantly evolved over time. Figure 1[2] shows a technician fixing an iron lung from the 1950s. Once primarily considered technical support personnel or technicians, respiratory therapists have transitioned into highly skilled clinical practitioners. This transformation has been driven by advancements in medical technology, increased complexity in patient care, and the growing recognition of respiratory therapists as essential members of the health care team. Today, respiratory therapists play a critical role in assessing, diagnosing, and managing cardiopulmonary conditions, collaborating with physicians, and making independent clinical decisions to optimize patient outcomes.
Respiratory therapists, also known as respiratory care practitioners, are health care professionals who are educated and trained to provide respiratory care to patients. About 75% of all respiratory therapists work in hospitals or other acute care settings. However, many respiratory therapists are employed in clinics, physicians’ offices, skilled nursing facilities, cardiopulmonary diagnostic laboratories, and public schools. Others work in research, disease-management programs, home care, and the sales industry. Some respiratory therapists work in colleges and universities, teaching students the skills they need to become respiratory therapists. Regardless of the practice setting, all direct patient care services provided by respiratory therapists must be done under the direction of a qualified physician. Medical directors are usually physicians who are specialists in pulmonary or critical care medicine.
There are approximately 200,000 respiratory therapists practicing in the United States. As the incidence of chronic respiratory diseases continues to increase, the demand for respiratory therapists is expected to be even greater in the years ahead. Although the respiratory therapist as a distinct health care provider was originally a uniquely North American phenomenon, since the 1990s there has been a steady increase in interest of other countries in having specially trained professionals provide respiratory care. This trend is referred to as the “globalization of respiratory care.”[3]
Professional Organizations
American Association for Respiratory Care
The American Association for Respiratory Care (AARC) is the leading national and international professional association for respiratory care. The AARC encourages and promotes professional excellence, advances the science and practice of respiratory care, and serves as an advocate for patients and their families, the public, the profession, and the respiratory therapist.[4]
Chartered Affiliates
All 50 states are known as chartered affiliates of the AARC. The chartered affiliates work hard to represent and protect the interests of respiratory therapists within their state. Chartered affiliates represent a great way for you to network with RT colleagues who live in your state and, by doing so, can boost your career potential. Chartered affiliates do much more than just serve as a way for therapists to get together. They provide RTs with the continuing education they need to maintain their license to practice and also advocate for legislation important to patients and the professional interests of RTs.[5]
The National Board for Respiratory Care
The mission of The National Board for Respiratory Care (NBRC) is to promote excellence in respiratory care by awarding credentials based on high-competency standards. The NBRC shares the RT’s goal of protecting and enhancing patient lives. Nearly 40,000 candidates test for NBRC credentials each year, seeking to demonstrate how excellence defines them across seven specific areas of respiratory care. These include Certified Respiratory Therapist (CRT), Registered Respiratory Therapist (RRT), Adult Critical Care (RRT-ACCS), Neonatal/Pediatric Respiratory Care (RRT-NPS), Certified or Registered Sleep Disorders Testing and Therapeutic Intervention (CRT-SDS or RRT-SDS), Certified or Registered Pulmonary Function Technology (CPFT or RPFT), and Asthma Education (AE-C).
NBRC credentials provide recognition for hard work and dedication to quality. Success on the exams brings respect among colleagues and instills a sense of pride in those who earn the NBRC badges of distinction. The NBRC accredited examinations, which are developed by respiratory care professionals and predictive of job performance, provide the opportunity to prove readiness for excellence in patient care.[6]
In 1960, Sister Mary Yvonne Jeann became the first Registered Inhalation Therapist and received registry number 1. The American Registry of Inhalation Therapists administered the first registry exams in Minneapolis, MN. both written and oral exams were required.
Commission on Accreditation for Respiratory Care (CoARC)
The Commission on Accreditation for Respiratory Care (CoARC) accredits Entry into Professional Practice respiratory care programs at the associate, baccalaureate, and master’s degree levels, as well as post-professional Degree Advancement respiratory care programs at the baccalaureate and master’s degree levels and Advanced Practice respiratory care programs at the graduate level. The CoARC also accredits certificate programs that train sleep disorders specialists offered by any of its accredited respiratory care programs. CoARC accreditation is limited to programs physically located in the United States and its territories.[7]
American Thoracic Society (ATS)
The American Thoracic Society (ATS) significantly influences respiratory therapy by setting clinical practice guidelines, providing educational resources, advocating for policy changes, and promoting research. ATS guidelines help standardize care and improve patient outcomes in respiratory conditions. The organization also offers training opportunities and fosters continuous professional development for respiratory therapists. Additionally, the ATS advocates for the profession, highlighting the critical role of respiratory therapists in patient care. Through research and collaboration, the ATS ensures that respiratory therapists are equipped with the latest knowledge and tools to deliver high-quality care.[8]
Federal Organizations
The Joint Commission
The Joint Commission (TJC) is a national organization that accredits and certifies over 20,000 health care organizations in the United States. The mission of TJC is to continuously improve health care for the public by inspiring health care organizations to excel in providing safe and effective care of the highest quality and value. TJC sets standards for providing safe, high-quality health care.[9]
Centers for Medicare & Medicaid Services
The Centers for Medicare & Medicaid Services (CMS) is another federal agency that establishes regulations that affect nursing care. The CMS is a part of the U.S. Department of Health and Human Services (HHS) that administers the Medicare program and works in partnership with state governments to administer Medicaid. The CMS establishes and enforces regulations to protect patient safety in hospitals that receive Medicare and Medicaid funding. For example, one CMS regulation states that a hospital’s policies and procedures must require confirmation of specific information before medication is administered to patients. This CMS regulation is often referred to as “checking the rights of medication administration.” CMS also enforces quality standards in health care organizations that receive Medicare and Medicaid funding. These organizations are reimbursed based on the quality of their patient outcomes. For example, organizations with high rates of health care-associated infections (HAI) receive less reimbursement for services they provide. As a result, many agencies have reexamined their policies, procedures, and protocols to promote optimal patient outcomes and maximum reimbursement.[10]
Exams/Credentialing and Licensure
Therapist Multiple-Choice/Clinical Simulation Examination Credentialing Exams
The Therapist Multiple-Choice (TMC) Examination objectively measures essential knowledge, skills, and abilities required of respiratory therapists at entry into practice. Passing the TMC Examination and wearing the CRT badge of distinction signal to employers, colleagues, and patients that you are committed to excellence in respiratory care. Additionally, all 49 states that regulate the practice of respiratory care use the CRT or RRT credential as the basis for state licensure.
The TMC Examination also determines your eligibility for the Clinical Simulation Examination (CSE), which is required for the RRT credential.
The TMC Examination offers two cut scores that determine whether or not you will receive credentials as a CRT or as an RRT. If you achieve the low-cut score, you earn the CRT credential. If you achieve the high-cut score, you earn the CRT credential and become eligible for the Clinical Simulation Examination (CSE) (provided you are eligible to earn the RRT credential).
The TMC Examination consists of 160 multiple-choice questions (140 scored items and 20 pretest items). You will be given 3 hours to complete the TMC Examination.[11]
Once you are credentialed, you will need to maintain your credentials by participating in continuing education activities.
State Licensure
Once you have obtained your CRT or RRT credentials, you will have to apply for state licensure before you are able to practice. Most states require a CRT credential to obtain a license; however, there is a general movement toward the RRT credential. In 49 states, you will prepare an application and pay a fee to the licensure board for the state in which you live. Typically, professional licensure is required to be renewed, and continuing education needs to be completed to obtain licensure in certain states.
The requirements for state licensure as a respiratory therapist can vary depending on whether the individual holds a CRT or RRT credential.
Certified Respiratory Therapist (CRT): In many states, individuals who have passed the CRT examination (administered by the NBRC) are eligible to apply for state licensure. The CRT is typically the entry-level credential, and in some states, it may be sufficient to obtain a license to practice as a respiratory therapist.
Registered Respiratory Therapist (RRT): The RRT credential, which requires passing both the CRT and an advanced-level clinical examination, is often preferred by employers and may be required for certain positions or advanced responsibilities. Some states may require the RRT credential as part of their licensure process, especially for those practicing in more specialized or supervisory roles.
While state licensure requirements vary, the RRT credential is generally seen as a higher level of certification and can offer more career opportunities and job flexibility. Additionally, in states where both CRT and RRT credentials are accepted for licensure, employers may prefer candidates with the RRT due to its advanced scope of practice and recognition in the field.
Legal Considerations, Ethics, and Morality
Respiratory therapists must be aware of the legal implications associated with their practice. Since respiratory therapists are licensed in 49 states, they can be held legally liable for negligence, malpractice, or breaches of patient confidentiality. Such violations may result in legal action, financial penalties, or even licensure revocation.
Beyond legal considerations, respiratory therapists must also adhere to ethical and moral principles that guide patient care. Upholding professional integrity, maintaining patient dignity, and making evidence-based decisions are essential in ensuring safe and ethical practice. By understanding both the legal and ethical responsibilities of their role, respiratory therapists can provide high-quality, patient-centered care while protecting themselves and their profession.
Negligence and Malpractice
Negligence is a general term that denotes conduct lacking in due care, carelessness, and a deviation from the standard of care that a reasonable person would use in a particular set of circumstances. Malpractice is a more specific term that looks at a standard of care, as well as the professional status of the caregiver. (See Figure 2.) To prove negligence or malpractice, the following elements must be established in a court of law:
- Duty owed to the patient
- Breach of duty owed to the patient
- Foreseeability
- Causation
- Injury
- Damages
Patient Confidentiality
In addition to negligence and malpractice, patient confidentiality is a major legal consideration for health care providers. Patient confidentiality is the right of an individual to have personal, identifiable medical information, referred to as protected health information (PHI), kept private. This right is protected by federal regulations called the Health Insurance Portability and Accountability Act (HIPAA). HIPAA was enacted in 1996 and was prompted by the need to ensure privacy and protection of personal health records and data in an environment of electronic medical records and third-party insurance payers. There are two main sections of HIPAA law: the Privacy Rule and the Security Rule. The Privacy Rule addresses the use and disclosure of individuals’ health information. The Security Rule sets national standards for protecting the confidentiality, integrity, and availability of electronically protected health information. HIPAA regulations extend beyond medical records and apply to patient information shared with others. Therefore, all types of patient information should only be shared with health care team members who are actively providing care to them.
You are required to adhere to HIPAA guidelines from the moment you begin to provide patient care. Respiratory students may be disciplined or expelled by their program for violating HIPAA. Respiratory therapists who violate HIPAA rules may be fired from their jobs or face lawsuits.[12]
Morality and Ethics
In addition to legal considerations, there is a code of ethics that respiratory therapists should adhere to (see AARC Code of Ethics and Professional Conduct). There is a difference between morality, ethical principles, and a code of ethics. Morality refers to “personal values, character, or conduct of individuals within communities and societies.” An ethical principle is a general guide, basic truth, or assumption that can be used with clinical judgment to determine a course of action. Some common ethical principles are beneficence (do good), nonmaleficence (do no harm), autonomy (control by the individual), veracity (be truthful), respondeat superior, and justice (fairness). A code of ethics is set for a profession and makes their primary obligations, values, and ideals explicit.[13]
View this supplementary YouTube[14] video: How to be an Ethical Respiratory Therapist
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Nursing fundamentals 2E. Open RN | WisTech Open. https://wtcs.pressbooks.pub/nursingfundamentals/ ↵
- "An_unidentified_man_makes_adjustments_to_an_iron_lung_(12618013383)” by City of Boston Archives is licensed under CC BY 2.0 ↵
- Dunne, P. J. (2017). History of respiratory care. In R. M. Kacmarek, J. K. Stoller, A. J. Heuer, R. L. Chatburn, & R. H. Kallet (Eds.), Eagan’s fundamentals of respiratory care (11th ed., p. 2). Elsevier. ↵
- American Association for Respiratory Care. (n.d.). About us. https://www.aarc.org/about-us/ ↵
- Wisconsin Society for Respiratory Care. (n.d.). About the WSRC. https://www.wsrc.online/about-us ↵
- The National Board for Respiratory Care. (n.d). About us. https://www.nbrc.org/about/ ↵
- Commission on Accreditation for Respiratory Care. (n.d.). Mission statement. https://coarc.com/about/mission-and-vision-statements/ ↵
- American Thoracic Society. (n.d.). Overview. https://site.thoracic.org/about-us/overview ↵
- The Joint Commission. (n.d.). Who we are. https://www.jointcommission.org/who-we-are/ ↵
- Centers for Medicare & Medicaid Services. (n.d.). About CMS. https://www.cms.gov/about-cms ↵
- The National Board for Respiratory Care. (n.d.). About us. https://www.nbrc.org/about/ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Nursing fundamentals 2E. Open RN | WisTech Open. https://wtcs.pressbooks.pub/nursingfundamentals/ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Nursing fundamentals 2E. Open RN | WisTech Open. https://wtcs.pressbooks.pub/nursingfundamentals/ ↵
- Respiratory Therapy Zone. (2022, June 10). How to be an ethical respiratory therapist [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=53fMtKurVe4&t=7s ↵

