1.1 Noninvasive Positive Pressure Ventilation (NIPPV)
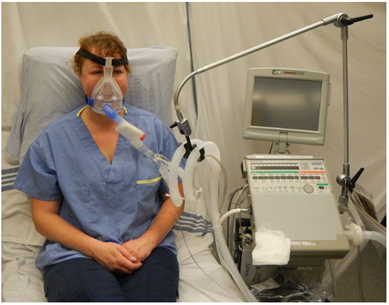
Noninvasive positive pressure ventilation (NIPPV) – sometimes just called noninvasive ventilation (NIV) – is a common therapy in critical care medicine. In the right patient population, it can be used instead of invasive ventilation and keep patients off mechanical ventilators. Selecting the appropriate patient for NIPPV is crucial, as using this intervention in an unsuitable setting can lead to treatment failure and increase the risk of patient aspiration. The classic NIPPV patient is alert with an intact drive to breathe (see Figure 1[1]). They either need some help with distending pressure or assistance with augmenting their tidal volumes with some extra support. Choosing initial settings on NIPPV is straightforward once you identify the therapy that is most beneficial to the patient.
NIPPV is the application of two different levels of pressure. There is a lower pressure that is there during expiration (EPAP), and then the pressure increases to a higher level during inspiration (IPAP). These two pressures remain constant and vary up and down based on the ventilator sensing inspiration and expiration. The IPAP and EPAP will not change unless the clinician increases or decreases the pressure settings. The EPAP may help oxygenation by methods of lung recruitment or opening collapsed airways. The IPAP is able to help improve the clearance of CO2 by augmenting each breath the patient is taking and by increasing the tidal volume, allowing more CO2 clearance with every breath.
When initiating noninvasive ventilation for a spontaneous breathing patient, there are three main settings that need to be adjusted, as well as one additional “back-up” setting. First, you will set the oxygen delivery (FiO2), a distending pressure to help recruit alveoli (EPAP), and a high pressure to augment the patient’s normal breath (IPAP). The back-up setting is a basic respiratory rate (RR). (Remember that this setting does not replace the patient spontaneously breathing.) Then, the efficacy of NIPPV is checked after 30 minutes, sometimes with an arterial blood gas or by reassessing the patient’s response to the treatment.[2]
- “BIPAP.JPG” by James Heilman, MD is licensed under CC BY-SA 4.0 ↵
- Bishop, M. (2022). Basic principles of mechanical ventilation. Sault College. https://ecampusontario.pressbooks.pub/mechanicalventilators/front-matter/introduction/ ↵

