1.1 Hyperinflation
Treating and preventing atelectasis is a foundational skill for respiratory therapists to understand and master. Atelectasis is a partial or complete collapse of alveoli that can lead to a patient’s pulmonary status being compromised and can cause hypoxemia, tachycardia, desaturation, and may lead to respiratory distress or failure. Hyperinflation therapy, sometimes referred to as lung expansion therapy, is a common treatment for patients with respiratory compromise that involves inflating the lungs with a greater than normal volume of air to inflate collapsed alveoli. Hyperinflation therapy should be implemented early for bedridden or postoperative patients to prevent or correct atelectasis. Patients who are at the greatest risk for postoperative atelectasis are patients who have had thoracic and upper abdominal surgeries or procedures and those with a history of mucus producing diseases. There are several devices that respiratory therapists can use to improve a patient’s pulmonary status. These hyperinflation devices can include incentive spirometry, Ezpap™/Versapap™, or intermittent positive pressure breathing (IPPB).
An important calculation that is necessary when performing hyperinflation is a patient’s ideal body weight (IBW). One way to calculate this is to utilize the formulas below:
Female: 105 + 5 (height in inches – 60)
Males: 106 + 6 (height in inches – 60)
Change the units from pounds to kilograms by dividing your answer by 2.2.
Example
To figure out the IBW of a 5’7” female, calculate and perform the order of algebraic operations: 105 + 5 (67 – 60) = 140
Divide that number by 2.2 = 63.63kg. IBW is always measured in kilograms.
Incentive Spirometry
An incentive spirometer is a medical device commonly prescribed after surgery to expand the lungs to keep alveoli open, reduce the buildup of fluid in the lungs, and prevent pneumonia. See Figure 1[1] for an image of a patient using an incentive spirometer. While sitting upright, if possible, the patient should exhale normally, place the mouthpiece in their mouth, and create a tight seal with their lips around it. They should breathe in slowly and as deeply as possible through the tubing with the goal of raising the piston to their prescribed level. The resistance indicator on the right side should be monitored to ensure they are not breathing in too quickly. The patient should attempt to hold their breath for as long as possible (at least 5 seconds) and then exhale and rest for a few seconds. Sustained maximal inhalation (SMI) should be achieved. Then, the patient should perform a breath hold at the point of SMI. Coughing is expected due to alveoli stretching to open more fully. Encourage the patient to expel any mucus produced and not swallow it. This technique should be repeated by the patient ten times every hour while awake.[2] The benefit of this therapy is dependent on the patient’s full effort.
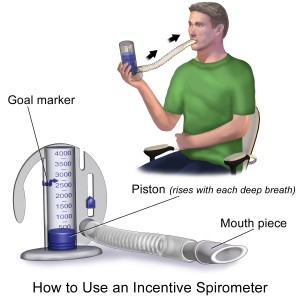
View the following supplementary YouTube video[3] demonstrating proper use of an incentive spirometer: How to Use an Incentive Spirometer – Nemours KidsHealth
PAP Therapy
PAP therapy includes several different devices. The Ezpap (see Figure 2[4]) and Versapap (see Figure 3[5]) are devices that are handheld and amplify an input flow of either air or oxygen approximately four times (Coanda effect), which allows positive pressure to be maintained throughout the patient’s breathing cycle. When ensuring an effective treatment, the respiratory therapist should make sure that there are no leaks coming from the patient. The patient should be appropriately coached and told to breathe through the mouthpiece with a tight seal. If the patient cannot keep a tight seal, the use of an Ambu mask is best to avoid leaks. Otherwise, a nose clip is suggested for patients who utilize the mouthpiece. This augmentation provides a larger flow and volume with less effort than an unsupported inspiration, and positive expiratory pressure (PEP) is provided on expiration. The prolonged exaltation time during this therapy enhances the effectiveness. Studies have shown that it is easier to tolerate than intermittent positive pressure breathing (IPPB) and has greater effect in reversing atelectasis than incentive spirometry. Thus, it can be used within physiotherapy to increase lung volume, clear secretions, and improve gaseous exchange.[6] When performing PAP therapy, we are looking for a therapeutic result of 10–20 cmH2O for exhalation and 2–5 cmH2O for inhalation. It should be noted that certain nebulizer devices can work in conjunction with these devices for a combined treatment.


View the following supplementary YouTube video[7] demonstrating how to set up an Ezpap device: EZPAP
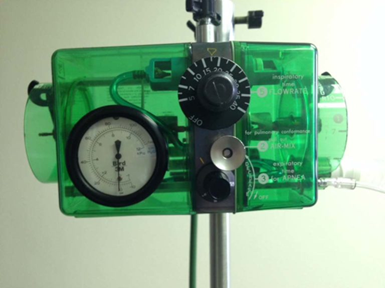
Intermittent Positive Pressure Breathing (IPPB)
Intermittent positive pressure breathing (IPPB) is a technique used to provide short-term or intermittent mechanical ventilation via mouthpiece or mask for the purpose of augmenting lung expansion. IPPB is usually not a therapy of choice in treating lung collapse, as there are other techniques that are less expensive and easier to administer; however, it can be effective when a patient needs a more aggressive lung expansion therapy and when PAP therapy is not effective. It is usually used when other therapies have failed, or a patient is not cooperating.[8]
The clinician asks the patient to breathe in on the IPPB circuit, and the machine gives some positive pressure support, followed by airway pressure returning to atmospheric pressure with passive expiration. The Bird Mark 7 IPPB machine (see Figure 4[9]) is a pressure-cycled device convenient to use for providing IPPB as an adjunct to hyperinflation therapy in the spontaneously breathing patient. The respiratory therapist can the set flow to help reach targeted pressures to help ensure a longer inspiratory time, which aids in lung expansion. IPPB may be applied to intubated and nonintubated patients.
- “Incentive Spirometer.png” by BruceBlaus is licensed under CC BY-SA 4.0 ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Nursing fundamentals 2E. Open RN | WisTech Open. https://wtcs.pressbooks.pub/nursingfundamentals/ ↵
- Nemours. (2018, January 16). How to Use an Incentive Spirometer - Nemours KidsHealth [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=Rmxfznw8Grk ↵
- “23-0747.jpeg” by unknown author is used on the basis of Fair Use. ↵
- “VersaPAP®-Device-3.jpg” by unknown author is used on the basis of Fair Use. ↵
- Elliott, S. (2011). A study to investigate the clinical use and outcomes of EZPAP positive pressure device. Thorax, 66(A96). https://thorax.bmj.com/content/66/Suppl_4/A96.1 ↵
- WorkWeb. (2020, January 28). EXPAP [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=X5taRLl8zTg ↵
- Physiopedia. (2022). Intermittent positive pressure breathing. https://www.physio-pedia.com/Intermittent_positive_pressure_breathing ↵
- “Bird_Mark_8_Medical_respirator1.JPG” by Stefan Bellini is licensed under CC0 ↵

