8.7 Contraception
Contraception, commonly referred to as birth control, is the act of preventing pregnancy by using a behavior, medication, device, or procedure. Birth control methods are designed to prevent conception or interrupt the implantation and growth of a fertilized embryo. Conception may be prevented in a variety of ways, including behaviors (such as abstinence, abstinence during fertile periods, or withdrawal before ejaculation), hormonally disrupting the menstrual cycle (such as using oral contraceptive medications, injections, implants, and vaginal rings), physically blocking the passage of sperm or release or eggs (such as using condoms, diaphragms, vasectomy, or tubal ligation), or implantation of a device (such as an intrauterine device or implanted rods).[1],[2]
Under the Affordable Care Act, most health care plans are required to provide birth control at no cost to their subscribers. Many factors must be considered by women, men, and couples when selecting an appropriate contraceptive method, such as safety, effectiveness, availability, and affordability. Protection against sexually transmitted infection (STI) must also be considered. For example, although hormonal contraceptives and IUDs are highly effective at preventing pregnancy, they do not protect against STIs. Consistent and correct use of a latex or plastic condom reduces the risk of transmission of STIs.[3]
The following contraceptive methods are listed by the most effective methods to prevent pregnancy to the least effective[4],[5]:
- Abstinence
- Outercourse
- Etonogestrel implant
- Intrauterine device (IUD) – levonorgestrel or copper
- Tubal ligation
- Vasectomy
- Injectable progesterone
- Oral contraceptives (combined or progestin-only)
- Hormonal patch
- Hormonal vaginal contraceptive ring
- Lactational amenorrhea
- Diaphragm or cervical cap
- Sponge
- Male condom
- Female condom
- Spermicides
- Fertility awareness-based methods
- Withdrawal
- Emergency contraception pills
Additional information about these contraceptive methods is summarized in the following subsections. As always, when providing client care, use evidence-based resources to review current information.
Read additional information about contraceptives on the “Birth Control Methods” page from the Office of Women’s Health or the “Birth Control” page of the Planned Parenthood website.
Abstinence
Abstinence is defined as not having sexual intercourse. It is the only contraceptive method that is 100% effective, safe, and free. Anyone can be abstinent, no matter their age, gender, sexuality, or previous sexual experiences. People are abstinent off and on for reasons that may change over time, and some people are abstinent their entire lives. However, abstinence means different things to different people. For some people, abstinence means no sexual activity with another person. For other people, abstinence means not having vaginal sex, but they may participate in other sexual activities like oral or anal sex.[6]
Outercourse
Many couples want to be sexual with each other without having vaginal sex and risking pregnancy. Outercourse prevents pregnancy the same way abstinence does, by keeping sperm away from an egg. Using outercourse as birth control means participation in sexual activities that do not involve the opportunity for semen to enter the vagina. Examples of outercourse may include kissing, touching, masturbating, dry humping, or using sex toys to achieve sexual pleasure.[7]
Etonogestrel Implant
An etonogestrel implant is a tiny, thin rod about the size of a matchstick that is inserted into a woman’s arm by a health care provider. The implant releases progestin in the body that prevents pregnancy by thickening cervical mucus (preventing sperm from swimming to the egg) and preventing ovulation. It is 99% effective and lasts for three years. Based on a person’s health insurance coverage, the implant can cost from $0 to $2,200.[8]
Women should not use the etonogestrel implant if they are pregnant or think they may be pregnant; have or have had blood clots; have liver disease or a liver tumor; have unexplained vaginal bleeding; or have breast cancer or any other cancer.[9]
Women should contact their health care professional immediately if they are unable to palpate the implant. A rare complication of an implant is it can migrate to the lungs and become a pulmonary emboli.[10]
Common side effects that may cause women to discontinue therapy are weight gain, mood swings, headache, acne, and depressed mood.[11] Remind clients to use additional methods to protect against STIs.[12]
View a supplementary YouTube video[13] from Planned Parenthood on birth control implants: Effectiveness of the Birth Control Implant in Your Arm.
Intrauterine Device
An intrauterine device (IUD) is a tiny plastic device shaped like a “T” that is placed in a woman’s uterus. There are two types of IUDs, hormonal and copper. Hormonal IUDs release progestin that prevents pregnancy by thickening cervical mucus (preventing sperm from swimming to the egg) and preventing ovulation. Depending on the brand, they prevent pregnancy for three to eight years. Copper IUDs are wrapped in copper and prevent pregnancy for up to 12 years by preventing sperm passage.[14] IUDs are 99% effective and can be removed by a health care provider if the client decides they would like to become pregnant. Based on a person’s health insurance coverage, IUDs cost $0 – $1,200.[15] See Figure 8.20[16] for an image of a hormonal IUD.

Women should not get a hormonal IUD if they have certain STIs or pelvic infection, think they might be pregnant, have breast or uterine cancer, have cervical cancer that hasn’t been treated, or have had a previous pelvic infection after childbirth or an abortion in the past three months.[17]
Women shouldn’t get a copper IUD if they have a copper allergy, Wilson’s disease, or a bleeding disorder. Women with systemic lupus erythematosus (SLE) are also at higher risk for heavy bleeding.[18]
IUDs can cause cramps and spotting after insertion, but side effects usually resolve within three to six months. Some women stop menstruating while an IUD is in place. In fact, many people get hormonal IUDs to help with heavy or painful periods and treat similar symptoms of endometriosis or polycystic ovarian syndrome.[19]
Clients should return to their health care provider as directed, typically four to six weeks after placement, to verify placement. IUD strings are 3-4 centimeters long and can be checked monthly by the client to ensure the IUD is in place.[20]
View a supplementary YouTube video[21] from Planned Parenthood on IUDs: What is an IUD?
Tubal Ligation
Tubal ligation, also called sterilization and commonly referred to as “getting your tubes tied,” is a safe and effective surgical procedure that permanently prevents pregnancy. It is 99% effective and can cost up to $6,000 based on the person’s health insurance coverage.[22]
During tubal ligation, the surgeon makes a small incision under the umbilicus and inserts a catheter with a camera to find the Fallopian tubes. A small tool is placed through another small incision in the lower abdomen and heat, clips, or rings are used to seal the tubes shut or remove them altogether. When Fallopian tubes are blocked or removed, sperm can’t get to an egg and cause pregnancy, but women will still have menstrual cycles. Sterilization is permanent and women should only undergo the procedure if they are certain they do not want to become pregnant for the rest of their lives. Although it may be possible to reverse a tubal ligation procedure or use in vitro fertilization to get pregnant after sterilization, there are no guarantees for pregnancy.[23] See Figure 8.21[24] for surgical images of a tubal ligation with bands placed on a woman’s bilateral Fallopian tubes.
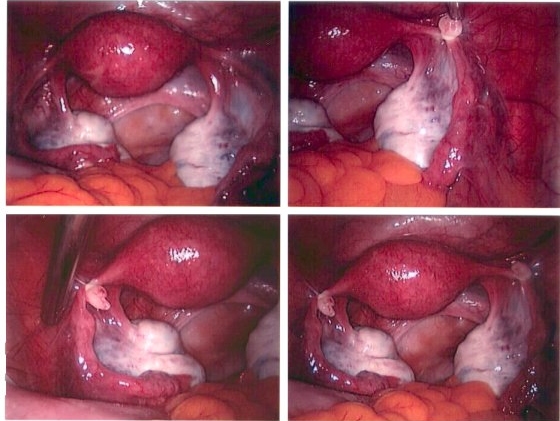
Tubal ligation procedures are very low-risk surgeries, but any kind of medical procedure can have complications. The risks of sterilization procedures include bleeding, side effects of general anesthesia, and infection, which is rare and can be treated with antibiotics. There is a very small chance that the Fallopian tubes can reconnect or become unblocked after tubal ligation. If a woman does become pregnant after tubal ligation, the pregnancy could develop in the Fallopian tube, called ectopic pregnancy, which can be life-threatening.[25]
Vasectomy
A vasectomy is a simple surgery done by a doctor in an office, hospital, or clinic. Because the vas deferens is easily accessible within the scrotum, surgical sterilization to interrupt sperm delivery can be performed by cutting and sealing a small section of these tubes so sperm can’t leave the body and cause pregnancy. This is a superficial procedure compared to tubal ligation, with fewer chances for complications.
There are two types of vasectomies, the incision method and the no-scalpel (no-cut) method. No-scalpel methods lower the risk of infection and other complications and generally take less time to heal. Vasectomies are 99% effective and cost up to $1,000 based on a person’s health insurance coverage.[26] See Figure 8.22[27] for an illustration of a vasectomy.
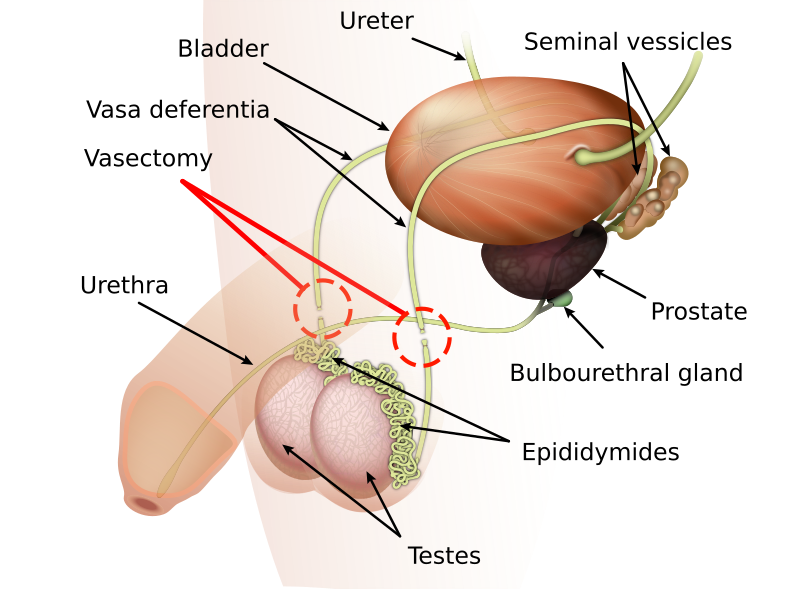
Starting at least two months after a vasectomy, the semen won’t contain any sperm, so it can’t cause pregnancy. Males must have their semen tested 8-16 weeks after the vasectomy to make sure there’s no sperm present in the semen. After a vasectomy, the semen will still look, feel, and taste the same, but there won’t be any sperm in it. Vasectomies don’t change the way having an orgasm or ejaculating feels, and they don’t impact the male’s hormone levels, sex drive, or ability to get an erection.[28]
Vasectomies are meant to be permanent. Although it is possible to reverse a vasectomy, pregnancy cannot be guaranteed after a vasectomy. Males should only get a vasectomy if they are certain they don’t want to be able to get someone pregnant for the rest of their life.[29]
Clients may have some discomfort, bruising, and/or swelling for a few days after their vasectomy. The following health teaching should be provided[30]:
- Wear snug underwear that prevents movement of testicles to help prevent discomfort.
- Use over-the-counter pain medication (like ibuprofen) to help with pain and swelling.
- Ice the genitals as needed on and off for the first 24 hours to help with pain and swelling.
- Don’t swim or take a bath for two days.
- Don’t do hard physical work or exercise for one week.
- Don’t have any kind of sex or masturbate for one week.
- Call your health care provider if you have a fever over 100° F, blood or pus coming from the incision site, or severe pain or swelling in the scrotum or testicles.
- Use alternative birth control until a negative sperm count is obtained.
Injection
A birth control injection (commonly known as Depo-Provera) is 96% effective if received once every 12 weeks. It contains the hormone progestin, which prevents pregnancy by thickening cervical mucus (preventing sperm from swimming to the egg) and preventing ovulation. Many people have lighter menstrual flow or stop menstruating after receiving injections for 12 months or more. The shot is temporary and can be stopped at any time if the client desires pregnancy, although it may take nine to ten months to get pregnant after stopping it. The injection can cost anywhere between $0 to $150, depending upon a person’s health insurance coverage.[31]
Most people experience changes in their periods the first year of receiving the shot, including bleeding more days than usual, spotting between periods, or no menstrual flow. Other possible side effects include nausea, weight gain, headaches, or sore breasts.[32]
People who use the hormonal birth control injection may have temporary bone thinning that increases the longer they use the shot. Bone density usually comes back after they stop using the birth control injection, unless they have already reached menopause. Clients should be educated to protect their bones by stopping smoking, getting regular weight-bearing exercise, and taking calcium supplements.[33]
Clients should notify their health care provider if they experience the following symptoms[34]:
- Severe depression
- Migraine with aura (i.e., severe headache preceded by bright, flashing lights)
- Pus, pain for many days, or bleeding from the injection site
- Very heavy vaginal bleeding or bleeding for more days than usual
- Yellowing of the skin or eyes
- Signs of deep vein thrombosis (like unilateral calf pain) or pulmonary embolism (sudden chest pain and shortness of breath)
Oral Contraceptives
Oral contraceptives are hormonal pills that come in a monthly pack. Clients take one pill every day. One pack costs $0 to $50/month, depending on the person’s health insurance coverage.[35] See Figure 8.23[36] for an image of a pack of birth control pills. Hormonal pills can be prescribed in various schedules. In one variation, the fourth week of pills does not contain hormones, and menstrual flow occurs during this week. In another schedule, a client can take daily hormonal pills for three months in a row and only have a menstrual flow four times a year.
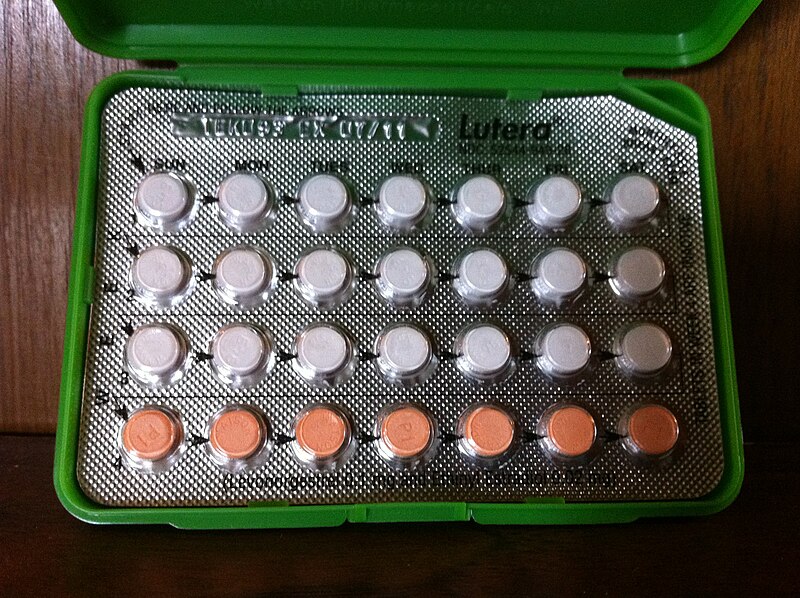
There are two kinds of birth control pills called combination pills (with estrogen and progestin) and progestin-only pills. If used perfectly, birth control pills are 99% effective, but in real life, people aren’t perfect, and it’s easy to forget or miss pills, so the pill is about 93% effective. Other factors can also decrease the effectiveness of birth control pills, including the following[37]:
- Vomiting or having diarrhea for more than 48 hours
- Antibiotic rifampin (other antibiotics don’t make the pill less effective)
- Antifungal griseofulvin (other antifungals don’t make the pill less effective)
- Certain HIV medicines
- Certain anti-seizure medicines (also used to treat psychiatric disorders like bipolar disorder)
- St. John’s Wort herb
If clients take any of these substances while on the pill, they should use condoms as a backup method or switch to a different method of birth control for long-time use. It takes some time for birth control pills to become effective. Depending on when they are started during the menstrual cycle and the kind of pill used, a backup birth control method (like condoms) should be used for up to seven days.[38]
The hormones in birth control pills can cause the following side effects that typically resolve in two to three months[39]:
- Headaches
- Nausea
- Sore breasts
- Changes in periods (early, late, or stopping altogether while on the pill)
- Spotting (bleeding between periods or brown discharge)
Some people use birth control pills because some of the side effects can be helpful to ameliorate symptoms. For example, the hormones in the pill can decrease painful, heavy, or irregular periods. In addition, the pill may ease cramps and the symptoms of premenstrual syndrome and usually make a woman’s period lighter and more regular.
The estrogen in combination pills can cause blood clots and increase the risk for myocardial infarction or cerebrovascular accident. People with the following conditions should avoid taking combination pills[40]:
- Smoking
- History of blood clots, an inherited blood-clotting disorder, or vein inflammation
- Breast cancer (estrogen can promote growth of some cancers)
- Myocardial infarction, cerebrovascular accident, angina, or other serious heart problems
- Migraine headaches with aura (seeing flashing, zigzag lines)
- Uncontrolled hypertension
- Uncontrolled diabetes
- Liver disease
Clients should immediately notify their health care provider or seek emergency assistance for the following symptoms[41]:
- Sudden back/jaw pain along with nausea, sweating, or trouble breathing
- Chest pain or discomfort
- Calf pain
- Dyspnea
- Severe abdominal pain
- Sudden, severe headache or headaches that are different, worse, or happen more often than usual
- Yellowing of the skin or eyes
View a supplementary YouTube video[42] on birth control pills from Planned Parenthood: How Does the Birth Control Pill Work and is It Safe to Use?
Read more information in the “Hormonal Contraceptives” section in the “Endocrine” chapter of Open RN Nursing Pharmacology, 2e.
Hormone Patch
The transdermal contraceptive patch is worn on certain parts of the body and is changed weekly. Similar to oral contraceptives, the patch releases estrogen and progestin to stop ovulation and thicken cervical mucus. The benefits, side effects, and contraindications are the same as combination oral contraceptives. The patch is 99% effective and costs $0 to $150/month, depending on the person’s health insurance coverage. Depending on the time of the menstrual cycle the first patch is started, backup birth control method (like condoms) may be needed the first seven days.[43]
Clients are taught the following strategies to manage their patches[44]:
- Store patches at room temperature and away from direct sunlight. Don’t store them in the refrigerator or freezer. Keep each patch sealed in its pouch until right before it is applied.
- Check the patch once a day to make sure it’s still sticking to the skin correctly.
- Don’t apply the patch in a place where it can be rubbed by tight clothes (like the waistband of pants or underwear).
- Make sure the skin where the patch will be placed is clean and dry. Don’t use lotion, oils, creams, powder, or makeup on the patch area.
- Apply the patch to the abdomen, buttocks, back, or upper outer arm.
- Hold the patch in place against the skin with the palm of your hand for ten seconds.
- Change the patch once a week for three weeks straight. On Week 4, take off the old patch and don’t wear a patch that week. This is when the client will get their period. After seven patch-free days, put on a new patch and start the cycle over. Each pack has three weekly patches in it, so three patches are used per month.
- When discarding the old patch, fold it in half so it sticks together, seal it in a plastic bag, and throw it in the trash. Make sure children or pets can’t get to it, and don’t flush it down the toilet to avoid environmental effects.
- The patch is made to stay in place while swimming, sweating, or in a jacuzzi, bathtub, shower, or sauna, but check the patch every day to make sure it’s sticking.
Hormonal Vaginal Contraceptive Ring
The vaginal contraceptive ring is a small, flexible ring placed inside the vagina and changed monthly. Similar to oral contraceptives, the ring releases estrogen and progestin to stop ovulation and thicken cervical mucus. The benefits, side effects, and contraindications are the same as oral combination contraceptives. The ring, commonly known as NuvaRing, is 93% effective and costs $0 to $200/month, depending on the person’s health insurance coverage.
Clients are taught the following strategies for managing their contraceptive vaginal rings:
- Store vaginal rings at room temperature and away from direct sunlight for up to four months. Keep rings that you won’t use within four months in the refrigerator.
- Keep rings away from children and pets.
- When the ring is in the vagina, don’t use any vaginal products with oil or silicone in them.
View a supplementary YouTube video[45] on the hormonal vaginal contraceptive ring from Planned Parenthood: What is the Birth Control Ring?
Lactational Amenorrhea
Women who exclusively breastfeed are not likely to ovulate or have periods the first six months after a baby is born. Exclusive breastfeeding means they nurse the baby at least every four hours during the day and every six hours at night and only feed their baby breast milk. Breastfeeding won’t prevent pregnancy if the baby is fed anything other than breast milk or if a breast pump is used instead of nursing. Furthermore, ovulation occurs before the first period, so it is possible for the client to not realize they are fertile and become pregnant.
Exclusive breastfeeding that is used as birth control is called the lactational amenorrhea method (LAM).[46] When performed perfectly, the LAM birth control method can be as effective as hormonal contraceptives for the six months after a baby is born. However, it is important for the client to understand that exclusive breastfeeding can only be used as birth control for the first six months of a baby’s life, or until their period returns. After that, breastfeeding is much less effective, especially as the baby begins to eat solid foods and sleeps longer at night.[47]
Read more about the benefits and risks of LAM in this open access article from Gynecology Endocrinology.[48]
Diaphragm or Cervical Cap
A diaphragm is a shallow, bendable cup made of soft silicone. Cervical caps are smaller than diaphragms and shaped like a sailor’s hat. Both devices are placed inside the vagina to cover the cervix and stop sperm from joining an egg. Both must be used with spermicide (a cream or gel that kills sperm) to be effective. The cervical cap can be left in longer than a diaphragm (up to two days), but diaphragms are slightly more effective at preventing pregnancy.[49] See Figure 8.24[50] for an illustration of diaphragm and spermicidal cream.

If used perfectly and placed over the cervix every time before having sex, the diaphragm is 94% effective. However, in real life diaphragms are about 83% effective because they are not used 100% perfectly, or they become dislodged during sex. For people who’ve never given birth, the cervical cap is 86% effective, and for people who have given birth, the cervical cap is 71% effective. Diaphragms and cervical caps cost anywhere from $0 to $90, depending on the person’s health insurance coverage.[51]
Clients are taught the following strategies to optimize the effectiveness of diaphragms and cervical caps[52]:
- Use the diaphragm or cervical cap every time you have vaginal sex.
- Use spermicide with your diaphragm or cervical cap.
- Insert the diaphragm or cervical cap two hours before you start having sex and before you’re aroused if possible.
- Make sure your diaphragm or cervical cap is covering your cervix.
- Use another method of birth control, along with your diaphragm, such as withdrawal or a condom.
- Leave your diaphragm or cervical cap in place for at least six hours after having sex.
If spermicide is used several times a day, it can irritate the vagina and increase the risk of getting HIV or other sexually transmitted infections. Some people who use diaphragms get recurrent urinary tract infections.[53]
Birth Control Sponge
The birth control sponge is a small, round sponge made from soft plastic that covers the cervix and contains spermicide to help prevent pregnancy. Each sponge has a fabric loop attached to it to make it easier to take out. The sponge can be used by itself or with condoms. Using the sponge plus a condom provides extra protection from pregnancy, as well as sexually transmitted infections.[54]
Women who have never given birth and always use the sponge perfectly every time they have sex can achieve a 91% effective rate. In real life, using the sponge perfectly can be hard, so the sponge is realistically 86% effective for women who’ve never given birth. Women who have given birth and always use the sponge perfectly every time they have sex can achieve about 80% effectiveness rate. Sponges can be purchased without a prescription at stores and cost $0 to $15.[55]
The sponge can be inserted up to 24 hours before sex, and once the sponge is in, it can be repeatedly used for up to 24 hours without replacing it. The sponge should be left in place for at least six hours after sex, but not for more than 30 hours total. Sponge users have a slightly higher risk of toxic shock syndrome, a rare but serious disease. Sponge users also have a higher risk of STIs because of vaginal irritation from the chemical Nonoxynol-9, which causes vaginal irritation and predisposes the body to infection.[56]
Side effects from spermicide are similar to those described under the “Diaphragm or Cervical Cap” subsection.
Male Condom
Male condoms are thin, stretchy pouches worn on the penis during sex to collect sperm and prevent it from entering the vagina. Latex and plastic condoms also provide protection from sexually transmitted infection (STI). If used perfectly every time before sexual activity, they are 87% effective. Condoms can be purchased without a prescription at drug stores and convenience stores for about $1 or $2 each.[57] See Figure 8.25[58] for an illustration of a male condom.
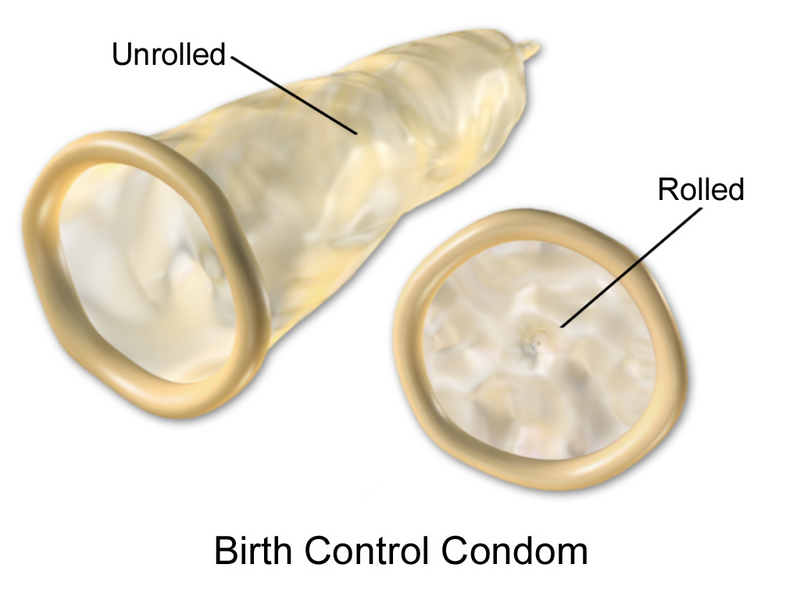
There are three types of condoms: latex, plastic, and lambskin. Latex condoms are made from rubber. Only water-based or silicone lubrication should be used with latex condoms because oil can damage latex condoms. Plastic/non latex condoms are made from plastics like polyurethane, nitrile, or polyisoprene and are safe for people with latex allergies. Water-based, silicone, and oil-based lubrication can be used with plastic condoms. Lambskin condoms are made from the lining of animal intestines (usually sheep) and are safe for people who are allergic or sensitive to latex. They only protect against pregnancy and do not protect against STIs. Any kind of lubrication, including oils, can be used with lambskin condoms.[59]
Nurses teach clients that using condoms every time they have oral, anal, or vaginal sex is the best way to reduce the risk of getting or spreading STIs. Condoms prevent contact with bodily fluids (like semen and vaginal fluids) that can carry infections. They also help protect against certain STIs like herpes and genital warts that are spread through skin-to-skin contact but are somewhat less effective because they don’t cover all the skin.[60]
Nurses teach clients how to apply a male condom with the following steps[61]:
- Check the expiration date printed on the wrapper or box. Open condoms carefully so you don’t damage them; don’t use your teeth or scissors.
- The rim of the condom should be on the outside so it looks like a little hat, and it will unroll easily. You can unroll it a little bit before putting it on to make sure it’s right-side out. If you accidentally put a condom on inside out, do NOT flip it around and reuse it — get a new one because sperm can be in pre-ejaculate.
- Pinch the tip of the condom and place it on the head of the penis and leave a little bit of space at the top to collect semen. If the male is uncircumcised, it might be more comfortable to pull the foreskin back before placing the condom on the tip of the penis and rolling it down.
- Roll the condom onto the penis when it is erect and before it touches your partner’s mouth or genital area. Apply it before any fluids that potentially contain sperm are on the penis. Unroll the condom down the shaft of your penis all the way to the base. Wear it the whole time you’re having sex.
- You can put a few drops of water-based or silicone lubricant inside the tip of the condom before you roll it on. You can also add more lubricant to the outside of the condom after it’s on the penis.
- After ejaculation, hold onto the rim of the condom as the penis is pulled out of your partner’s body. Do this before the penis goes soft, so the condom doesn’t get too loose and let semen out.
- Dispose of condoms in the trash. Don’t flush them down the toilet because they can clog pipes.
- Don’t reuse condoms. Roll on a new condom every time you have vaginal, oral, or anal sex. You should also use a new condom if you switch from one kind of sex to another (like anal to vaginal).
- If the erection is lost during sex, the condom should be removed. Reapply a new one when the penis becomes erect.
View a supplementary YouTube video[62] on male condoms by Planned Parenthood: What is a Condom and How is it Used?
Internal Condoms
Internal condoms (also called female condoms) provide similar protection from pregnancy and STIs as male condoms. Instead of going on the penis, internal condoms go inside the vagina for pregnancy prevention or into the vagina or anus for protection from STIs. They are made from nitrile, a type of soft plastic. Internal condoms are available without a prescription in stores and online and usually cost around $2 or $3.[63] See Figure 8.26[64] for an image of an internal condom.

Nurses teach clients how to use internal condoms with the following steps[65]:
- Check the expiration date on the package and then open it carefully.
- The internal condom comes already lubricated, but you can add more lubricant if needed.
- If you’re putting the condom in your anus, remove the inner ring. If you’re putting the condom in your vagina, leave the ring in.
- Relax and get into a comfortable position, such as standing with one foot on a chair, lying down, or squatting.
- If the internal condom is going in your vagina, squeeze together the sides of the inner ring at the closed end of the condom and slide it in like a tampon. Push the inner ring into your vagina as far as it can go, up to your cervix. If it’s going in your anus, push the condom in with your finger.
- Make sure the condom isn’t twisted.
- Hold the condom open as the penis or sex toy is going into the condom to make sure it doesn’t slip to the side between the condom and your vagina or anus.
- When removing the internal condom, if there’s semen in the condom, twist the outer ring (the part that’s hanging out) to keep the semen inside the pouch. Gently pull it out of your vagina or anus, being careful not to spill the semen if there is any.
- Dispose used condoms in the trash because they can clog the toilet.
- Internal condoms are not reusable. Use a new one every time you have sex.
View a supplementary YouTube video[66] on internal condoms by Planned Parenthood: What is a Female Condom (aka Internal Condom) and How Does it Work?
Fertility Awareness Methods
Fertility awareness methods (FAMs), also called natural family planning and the rhythm method, are ways to track the menstrual cycle and fertile days to prevent pregnancy. The days near ovulation are fertile days when pregnancy may occur, so people prevent pregnancy by abstinence or using another birth control method (like condoms) on fertile days.[67] The fertile window when a client can become pregnant is five days before ovulation up through the day after ovulation. Sperm can live in a woman’s body and fertilize an egg at any time for up to five days.[68]
Methods to track fertile days include the following[69],[70]:
- The Temperature Method: Basal body temperature is taken in the morning every day before getting out of bed. Women track the temperature trends for several months to get an idea of length of cycle and approximate ovulation timing. Body temperature drops slightly prior to ovulation and rises 0.4-0.8 degrees after. Because the temperature rise is so slight, clients need to use a sensitive basal body temperature thermometer to detect these changes. Most women ovulate within three days of the temperature spike. Clients are most likely to become pregnant two to three days before and up to 24 hours after the temperature spike. Women should understand activities that can affect temperature such as smoking, drinking alcohol, or sleeping poorly the night before, having a fever, or moving around prior to taking the temperature.
- The Cervical Mucus Method: Cervical mucus (vaginal discharge) is monitored every day. Cervical mucus changes prior to and during ovulation and is regulated by hormones of the menstrual cycle. Cervical mucus is absent for a few days after a menstrual period and then appears in the vagina as white or yellow, cloudy, and sticky. Just before ovulation, the cervical mucus becomes clear, stretchy, and slippery, the consistency of egg whites. This mucus lasts four days. A woman’s most fertile time is up to two days before the wetness begins until it becomes sticky and cloudy again. A woman then has a few dry days before menstruating. The cervical mucus method is less reliable for clients who are breastfeeding, using hormonal birth control or feminine hygiene products, have had cervical surgery, or have STI or vaginitis.
- The Calendar Method: The menstrual cycle is tracked on a calendar for 8-12 months to determine the length of the menstrual cycle (between 26 and 32 days long). Days 8-19 are fertile days, using the shortest cycle. The number of days per cycle may vary among women and from month-to-month in an individual, so fertile days are an estimate.
- Ovulation Calculator: Clients may use an ovulation calculator to estimate the day of ovulation in a cycle.
It is most effective to combine all these methods. When accurately and consistently used together, they are about 77%–98% effective.[71]
View a sample ovulation calendar from the Office on Women’s Health: Women’s Health Ovulation Calculator.
Withdrawal
Withdrawal (also called pulling out) is a way to prevent pregnancy by pulling the penis out of the vagina before ejaculation to keep semen away from the vagina. However, males can have sperm in pre-ejaculate fluids. Withdrawal works best with another method of birth control, like a condom. If performed accurately and consistently every time during sex, withdrawal can be up to 96% effective. The withdrawal method is not a good way to prevent pregnancy if the male experiences premature ejaculation. It also requires a great deal of self-control to be willing and able to stop having sex and remove your penis away from your partner’s vagina, right when you’re at the height of sexual pleasure, so the real-life effectiveness of the withdrawal method is about 78%.[72]
Emergency Contraception
Emergency contraception is not considered a routine method of birth control. Emergency contraception is used if no birth control was used during sex or if the birth control method failed, such as the breakage of a condom. Emergency contraception includes emergency contraceptive pills and insertion of a copper IUD.[73]
Women can take emergency contraceptive pills up to five days after unprotected sex to prevent pregnancy. Because sperm can live inside a woman’s body for up to five days after sex and waiting to fertilize an egg, emergency contraceptive pills work by temporarily stopping the ovary from releasing an egg. There are two types of morning-after pills in the United States[74]:
- A pill with ulipristal acetate that requires a prescription. There is only one brand of this medication in the U.S. and is called “Ella.”
- A pill with levonorgestrel, such as the brand name “Plan B One Step.” Levonorgestrel emergency contraceptive pills can be purchased without a prescription in many drugstores.
Emergency contraceptive pills have upper weight limits for effectiveness and cost about $50 each. Plan B may be slightly less effective in clients weighing greater than 155 pounds, and Ella is most effective in clients over 195 pounds.[75]
Women should not use emergency contraceptive pills as their routine method of birth control because they don’t work as well as other types of birth control like the IUD, implant, pill, shot, or ring. Taking the morning-after pill repeatedly is more expensive than using a regular method of birth control. Side effects like nausea and bleeding between periods may occur and are temporary. Emergency contraceptive pills do not have long-term side effects and won’t affect the ability to get pregnant in the future. They are not the same as mifepristone or misoprostol, pills used to terminate pregnancy. They will not work if the woman is already pregnant, and they won’t harm an existing pregnancy.[76]
View a supplementary YouTube video[77] about emergency contraception from Planned Parenthood: How Does the Morning After Pill / Emergency Contraception Work?
Unintended Pregnancy
Women experiencing an unintended pregnancy need therapeutic communication and information about their pregnancy options that include giving birth and raising the child, having a medical or surgical abortion, or giving birth and placing the infant for adoption. A medical or surgical abortion is the termination of a pregnancy before a fetus can survive outside the uterus. Adoption is the permanent and legal transfer of parental rights from a child’s biological parent(s) to adoptive parent(s). The decision to end a pregnancy by abortion is very personal. Nurses provide information about pregnancy options and encourage clients to discuss their feelings with a health care provider, counselor, family member, or friend to help weigh their options and make a decision.[78]
A medical abortion uses medications to terminate a pregnancy within 11 weeks of the woman’s last menstrual period. A combination of two prescription hormone medications is often used to cause the woman’s body to expel the fetus and placenta tissue. Mifepristone blocks progesterone, the hormone required to maintain pregnancy, and misoprostol causes uterine contractions to empty the uterus of the fetus and the placenta. Most women have moderate to heavy bleeding and cramping for several hours after taking the medications and may also have nausea, diarrhea, and vomiting from taking misoprostol. A medical abortion is 98% effective before Week 10 of gestation. By Week 11, it is only 87% effective, and an extra dose of misoprostol may be required that results in more intense cramping. Prior to 12 weeks’ gestation, an induced medical abortion can be managed at home if the woman has accurate information, medication, and access to a health care provider should adverse effects occur. It is important for the woman to follow-up with their health care provider to ensure the process was completed and all the tissue was expelled. A pregnancy test, ultrasound, or blood test may be used to determine if the medical abortion was effective.[79],[80]
An abortion by a surgical procedure involves dilating the cervix and placing a small suction tube into the uterus. Suction is used to remove the fetus and placental tissue from the uterus. After the procedure, medications may be prescribed to help the uterus contract to reduce bleeding, and antibiotics may be prescribed to prevent infection. Nurses encourage clients to make arrangements to prevent pregnancy, especially during the first month after the procedure.[81]
Women may consider having an abortion for several reasons, including the following[82]:
- A personal decision to not carry the pregnancy and give birth.
- The fetus has a severe birth defect or genetic problem.
- The pregnancy may be harmful to their health.
- The pregnancy resulted after a traumatic event such as rape or incest.
Read more about pregnancy options from Planned Parenthood: Pregnancy Options.
- Bansode, O. M. (2023). Contraception. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK536949/ ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Centers for Disease Control and Prevention. (2024). Contraception and birth control methods. https://www.cdc.gov/contraception/about/index.html ↵
- Bansode, O. M. (2023). Contraception. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK536949/ ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Organon. (n.d.). Meet Nexaplanon: The birth control implant that goes in your arm. https://www.nexplanon.com/ ↵
- Kareem, T., Frain, D., Raza, S., & Watson, N. A. (2025). Subdermal contraceptive implant migration to pulmonary artery branch. BMJ Case Reports, 18(1), e262771. https://doi.org/10.1136/bcr-2024-262771 ↵
- Nexaplanon. (n.d.). Meet Nexaplanon: The birth control implant that goes in your arm. https://www.nexplanon.com ↵
- Organon. (n.d.). Meet Nexaplanon: The birth control implant that goes in your arm. https://www.nexplanon.com/ ↵
- Planned Parenthood. (2019, July 19). Effectiveness of the birth control implant in your arm | Planned Parenthood video [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=47I3nlODVu8 ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- “31140095680_f5f20628b5_h” by Sarah Mirk is licensed under CC BY-NC 2.0 and “IUD.jpg” by Sarah Mirk is licensed under CC BY 2.0 ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Robinson, K. M. (2023). How to know if your IUD is out of place. WebMD. https://www.webmd.com/sex/birth-control/features/iud-out-of-place ↵
- Planned Parenthood. (2023, August 22). What is an IUD? | Planned Parenthood video [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=nrWel3SHf6s ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- “413638107_391ba41310_o” by Serolynne is licensed under CC BY-NC-ND 2.0 ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- “Vasectomy_diagram-en.svg” by K. D. Schroeder is licensed under a CC BY-SA 3.0 ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- “Package_of_Lutera_Birth_Control_Pills.jpg” by ParentingPatch is licensed under CC BY-SA 3.0 ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Planned Parenthood. (2016, January 4). How does the birth control pill work and is it safe to use? | Planned Parenthood video [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=jIolmLbBiw0 ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Planned Parenthood. (2023, August 22). What is the birth control ring? | Planned Parenthood video [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=QxQ_kIIMtKs ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Genazzani, A. R., Fidecicchi, T., Arduini, D., Giannini, A., & Simoncini, T. (2023). Hormonal and natural contraceptives: a review on efficacy and risks of different methods for an informed choice. Gynecological Endocrinology, 39(1), 1–13. https://doi.org/10.1080/09513590.2023.2247093 ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- “Birth_Control_Diaphragm.png” by BruceBlaus is licensed under CC BY-SA 4.0 ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- “Male_Condom.png” by BruceBlaus is licensed under CC BY-SA 4.0 ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Planned Parenthood. (2015, May 15). What is a condom and how is it used? | Planned Parenthood video [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=Eh5HK3F42IU ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- “Femidom1.jpg” by Villy Fink Isaksen is licensed under CC BY 3.0 ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Planned Parenthood. (2019, July 1). What is a female condom (aka internal condom) and how does it work? | Planned Parenthood video [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=P0gd7kUf1bo ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Office on Women’s Health. (2021). Trying to conceive. https://www.womenshealth.gov/pregnancy/you-get-pregnant/trying-conceive ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Office on Women’s Health. (2021). Trying to conceive. https://www.womenshealth.gov/pregnancy/you-get-pregnant/trying-conceive ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Planned Parenthood. (n.d.). Birth control. https://www.plannedparenthood.org/learn/birth-control ↵
- Centers for Disease Control and Prevention. (2024). Contraception and birth control methods. https://www.cdc.gov/contraception/about/index.html ↵
- Centers for Disease Control and Prevention. (2024). Contraception and birth control methods. https://www.cdc.gov/contraception/about/index.html ↵
- Villines, A. (2023). Is there a Plan B weight limit? https://www.medicalnewstoday.com/articles/plan-b-weight-limit#other-options ↵
- Centers for Disease Control and Prevention. (2024). Contraception and birth control methods. https://www.cdc.gov/contraception/about/index.html ↵
- Planned Parenthood. (2023, August 22). How does the morning after pill / Emergency contraception work? | Planned Parenthood video [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=ETjS_i2BwJQ ↵
- Planned Parenthood. (n.d.). Pregnancy options. https://www.plannedparenthood.org/learn/pregnancy/pregnancy-options ↵
- Planned Parenthood. (2024). The abortion pill. https://www.plannedparenthood.org/learn/abortion/the-abortion-pill ↵
- MedlinePlus [Internet]. (2023). Abortion - medication. https://medlineplus.gov/ency/article/007382.htm ↵
- MedlinePlus [Internet]. (2022). Abortion - procedure. https://medlineplus.gov/ency/article/002912.htm ↵
- MedlinePlus [Internet]. (2022). Abortion - procedure. https://medlineplus.gov/ency/article/002912.htm ↵
The moment when a sperm fertilizes an egg, leading to the formation of an embryo.
The choice to not engage in sexual activity, which is the only 100% effective method to prevent pregnancy and sexually transmitted infections (STIs).
Sexual activities that do not involve vaginal intercourse, which can help reduce the risk of pregnancy and STIs when no bodily fluids are exchanged.
A tiny, thin rod about the size of a matchstick that is inserted into a woman’s arm by a health care provider.
A tiny plastic device shaped like a “T” that is placed in a woman’s uterus.
Also called sterilization and commonly referred to as “getting your tubes tied,” is a safe and effective surgical procedure that permanently prevents pregnancy.
A surgical procedure that involves cutting or sealing the vas deferens to prevent sperm from reaching the semen, effectively sterilizing the male.
A flexible, small ring that is inserted into the vagina, releasing hormones (estrogen and progestin) to prevent ovulation and pregnancy.
Feeding an infant only breast milk, without any additional food or drink, which can delay the return of fertility in some women for up to six months after childbirth.
A natural contraceptive method based on exclusive breastfeeding, which temporarily suppresses ovulation and fertility due to the hormonal effects of lactation.
A shallow, dome-shaped barrier method made of silicone or latex that covers the cervix to block sperm from entering the uterus. Used with spermicide for increased effectiveness.
A barrier form of contraception made of silicone that is inserted into the vagina and fits over the cervix to prevent sperm from entering the uterus.
A chemical agent that kills or immobilizes sperm to prevent pregnancy.
Also known as female condoms, these are inserted into the vagina to prevent pregnancy and protect against STIs by acting as a barrier to sperm.
Techniques to track a woman’s menstrual cycle and identify fertile days to avoid or achieve pregnancy. These methods include monitoring basal body temperature, cervical mucus, and cycle length.
The legal process where a child is permanently placed with a parent or parents other than the biological ones, establishing legal rights and responsibilities.

