7.4 General Treatments for Mental Health Conditions
Mental health conditions are commonly treated by an interprofessional team with a combination of treatments, such as psychotherapy, psychotropic medications, medical procedures, and nursing interventions and health teaching.[1]:
Psychotherapy
According to the American Psychological Association, psychotherapy refers to any psychological service provided by specially trained mental health professionals that primarily uses forms of communication and interaction to assess, diagnose, and treat dysfunctional emotional reactions, ways of thinking, and behavior patterns. Common psychotherapy treatments are discussed in more detail in the “Psychotherapy” section of this chapter.
Psychotropic Medications
Psychotropic medications are medications that affect the mind, emotions, and behavior. Specific classes of psychotropic medications are discussed in more detail in the “Psychotropic Medications” section of this chapter.
Medical Procedures
Specific medical procedures are performed to treat certain mental health conditions, such as electroconvulsive therapy (ECT) and transcranial magnetic stimulation.
Electroconvulsive Therapy
Electroconvulsive therapy (ECT) is a safe and effective medical treatment used for clients with severe major depression or other severe mental illnesses who have not responded to medications, psychotherapy, or other treatments. Nurses can help clients understand its use and dispel myths. ECT involves a brief electrical stimulation of the brain that causes a seizure while the client is under anesthesia. Decades of research have developed theories explaining the mechanism of action for ECT, such as the induced seizure stimulates neurons and neurotransmission, growth of neurons, brain volume, synapses, cerebral vasculature and blood flow, and changes to glucose metabolism.[2]
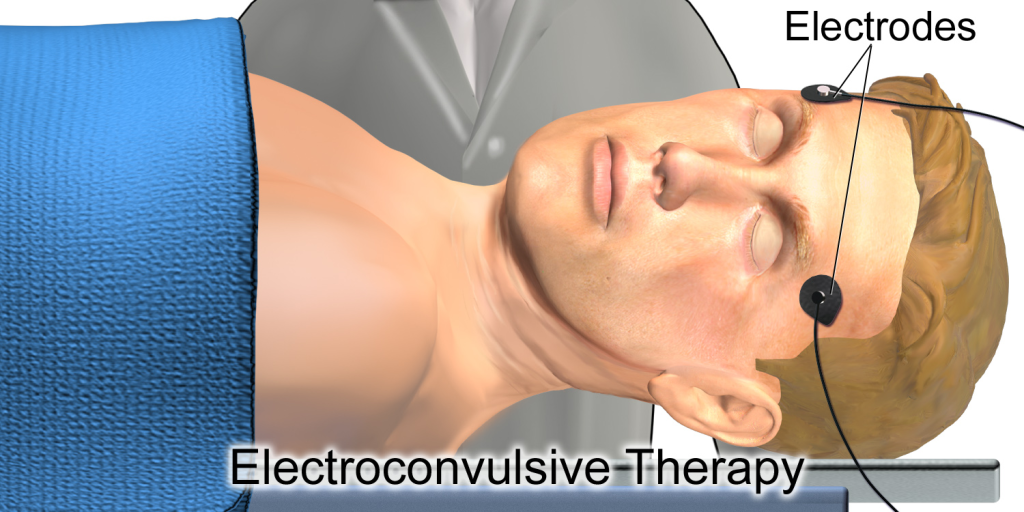
ECT treatments are managed by a team of trained medical professionals, including a psychiatrist, an anesthesiologist, and a nurse. See Figure 7.3[3] for an illustration showing ECT electrode placement.
A client must provide written informed consent before ECT is administered. In situations where a client is too ill to make decisions for themselves, the consent process is governed by state law (for example, a court-appointed guardian). A client typically receives multiple sessions of ECT, depending on the severity of symptoms and the response to treatment.
General anesthesia is provided during ECT, so presurgical preparation requires no food or water after midnight and only a sip of water with morning medications. An intravenous line is inserted, and electrode pads are placed on the head. At the time of each treatment, a client also receives a muscle relaxant. The client’s brain is stimulated with a brief controlled series of electrical pulses. This causes a seizure within the brain that lasts for approximately one minute. The client is asleep for the procedure and awakens after five to ten minutes, much as from minor surgery.
ECT treatment has been associated with some risks such as short-term memory loss and difficulty learning. Some people have trouble remembering events that occurred in the weeks before the treatment or earlier. In most cases, memory problems improve within a couple of months. Some clients may experience longer-lasting problems, including permanent gaps in memory.
Nursing actions regarding ECT include the following:
- Screening tools used pre- and post-ECT to evaluate side effects, including memory loss
- Medication administration
- Post-ECT care such as monitoring vital signs; changes in airway, breathing, and circulation; and implementing fall risk precautions post-anesthesia
Transcranial Magnetic Stimulation
Transcranial magnetic stimulation (TMS) is a noninvasive procedure that uses magnetic fields to stimulate nerve cells in the brain to improve symptoms of depression. TMS is typically used when other depression treatments haven’t been effective. Unlike electroconvulsive therapy (ECT), in which electrical stimulation is more generalized, TMS can be targeted to a specific site in the brain. A typical TMS session lasts 30 to 60 minutes and does not require anesthesia. During the procedure, an electromagnetic coil is held against the forehead near an area of the brain that is thought to be involved in mood regulation. Short electromagnetic pulses are administered through the coil. The magnetic pulses easily pass through the skull and cause small electrical currents that stimulate nerve cells in the targeted brain region. The magnetic field is about the same strength as that of a magnetic resonance imaging (MRI) scan. The person generally feels a slight knocking or tapping on the head as the pulses are administered. The muscles of the scalp, jaw, or face may contract or tingle during the procedure, and mild headaches or brief lightheadedness may result after the procedure. It is possible the procedure could cause a seizure, although this adverse effect is uncommon. Because the treatment is relatively new, long-term side effects are unknown.
Nursing Interventions
Nurses care for clients with mental health conditions in all health care settings. The top priority of nursing care is to keep the client, staff, and other clients in the environment safe. If the client has suicidal ideation, the nurse implements measures like modifying the environment and implementing a safety plan. Review information about suicidal ideation and safety interventions in the “Suicide Screening and Safety Interventions” section of this chapter. If a client, family member, or visitor demonstrates escalating agitation, the nurse implements de-escalation techniques and crisis intervention, if appropriate. Review verbal de-escalation techniques in the “Workplace Violence” section of the “Maladaptive Coping Behaviors” chapter. Review information about crisis and crisis intervention in the “Basic Concepts of Mental Health and Mental Illness” section in the “Mental Health Concepts” chapter. In some situations, severely agitated clients may require seclusion or behavioral restraints for safety. Review information about seclusion and restraints in the “Ethical and Legal Considerations of Mental Health Care” subsection of the “Basic Concepts of Mental Health and Mental Illness” section of the “Mental Health Concepts” chapter.
Another priority of nursing care is managing the physiological effects of mental health conditions such as nutritional or fluid imbalances, altered elimination, disrupted sleep, or self-care deficits. Specific nursing interventions related to physiological effects are discussed in the following sections of this chapter focused on mental health conditions.
The third priority of nursing care is to help clients and their family members effectively cope with the effects of mental health conditions and prevent relapse. Nurses implement a variety of interventions to facilitate effective coping:
- Nurses begin by building therapeutic relationships with clients and family members. Review information about “Therapeutic Relationship” in the “Basic Concepts of Mental Health and Mental Illness” section of the “Mental Health Concepts” chapter and therapeutic communication in the “Communicating With Patients” section of the “Communication” chapter of Open RN Nursing Fundamentals, 2e.
- Nurses are aware that individuals who have a history of trauma may have intense feelings triggered when engaging with the health care system that stimulate their “fight, flight, or freeze” stress response. This response can affect the client’s ability to interact with health professionals and may impact their ability to adhere to treatment plans. Nurses implement principles of trauma-informed care for all clients. Review the “Trauma-Informed Care” subsection in the “Basic Concepts of Mental Health and Mental Illness” section of the “Mental Health Concepts” chapter.
- Nurses monitor and document client appearance, mood, and behaviors, and notify the health care provider of changes in condition that may require additional treatment. Review information about performing a mental status examination and psychosocial assessment in the “General Assessments for Mental Health Conditions” section of this chapter.
- Nurses administer prescribed psychotropic medications, monitor for side effects, and evaluate therapeutic response. They teach clients and family members about routine monitoring, common side effects, and symptoms to promptly report to the health care provider. Specific information about classes of psychotropic medications is discussed in the “Psychotropic Medications” section of this chapter.
- Nurses provide health teaching to clients and their family members about the mental health condition, treatments, and positive coping strategies. Review information about positive coping strategies in the “Stress and Coping” and “Applying the Nursing Process and Clinical Judgment Model to Promote Healthy Coping” sections of the “Mental Health Concepts” chapter.
- Nurses consider the impact of a client’s diagnosis on their role performance and the effect on family dynamics. Review information about family dynamics and caregiver role strain in the “Family Dynamics” chapter.
- Nurses refer clients to mental health professionals, community resources, and specific support groups. Find information about online support groups on the National Alliance on Mental Illness website.
- Ernstmeyer, K., & Christman, E. (Eds.). (2022). Nursing: Mental health and community concepts. https://wtcs.pressbooks.pub/nursingmhcc/ ↵
- Singh, A., & Kar, S. K. (2017). How electroconvulsive therapy works: Understanding the neurobiological mechanisms. Clinical Psychopharmacology and Neuroscience, 15(3), 210–221. https://doi.org/10.9758/cpn.2017.15.3.210 ↵
- “Electroconvulsive_Therapy.png” by BruceBlaus is licensed under CC BY-SA 4.0 ↵
Refers to any psychological service provided by specially trained mental health professionals that primarily uses forms of communication and interaction to assess, diagnose, and treat dysfunctional emotional reactions, ways of thinking, and behavior patterns.
Drugs that treat mental health symptoms.
A safe and effective medical treatment used for clients with severe major depression or other severe mental illnesses who have not responded to medications, psychotherapy, or other treatments.
A noninvasive procedure that uses magnetic fields to stimulate nerve cells in the brain to improve symptoms of depression.

