7.17 Autism Spectrum Disorder
Autism spectrum disorder (ASD) is a neurodevelopmental disorder that significantly affects a person’s behavior and their ability to socially communicate and interact. It occurs in all ethnic, racial, and economic groups. Although autism can be diagnosed at any age, it is classified as a developmental disorder because symptoms generally appear in early childhood.[1] One out of 36 children in the United States has ASD with four times as many males than females. Autism is known as a “spectrum” disorder because of the wide variation in the type and severity of symptoms individuals may experience.[2]
ASD is diagnosed by a mental health professional based on behaviors classified under the following two categories[3]:
- Ongoing deficits in social communication and social interactions across multiple contexts
- Restricted, repetitive patterns of behaviors, interests, or activities
Symptoms are present in the early developmental stages but may not manifest until social demands exceed limited capacities. Symptoms cause significant impairment in social, occupational, or other areas of functioning. Severity is indicated by the level of support needs, ranging from “requiring support” to “requiring substantial support” to “requiring very substantial support.”[4]
Although people with ASD experience challenging symptoms, they may also have strengths, including the following[5]:
- Being able to learn things in detail and remember information for long periods of time
- Being strong visual and auditory learners
- Excelling in math, science, music, or art
Children with autism are more likely to experience comorbid conditions such as insomnia, ADHD, intellectual disability, anxiety, and depression than peers without autism. These conditions must also be treated to reduce their impact.[6] See Figure 7.11[7] for an image of a child depicting communication barriers related to ASD.

View a supplementary YouTube video[8] about ASD by the American Psychiatric Association: What is Autism? | APA.
Research suggests genetics are influenced by the environment to affect development in ways that can lead to ASD. Risk factors include the following:
- A sibling with ASD
- Older parents at birth
- Genetic conditions such as Down syndrome and Fragile X syndrome
- Very low birth weight
A common myth that has been refuted is that the measles, mumps, rubella (MMR) vaccine causes autism. This myth began due to falsified research that has since been retracted and the researcher’s license to practice medicine revoked when investigation showed the client data was falsified. Twenty-five research studies have refuted any connection between autism and the MMR vaccine or its components. This is an important topic during health teaching about vaccinations because some parents choose not to vaccinate due to the false belief it may cause autism.[9]
Assessment of ASD (Recognizing Cues)
The American Academy of Pediatrics recommends all children be screened for developmental milestones at well-child visits, with autism-specific screening performed at 18 and 24 months of age.[10] View an illustration of sample developmental milestones by age in Figure 7.12.[11]
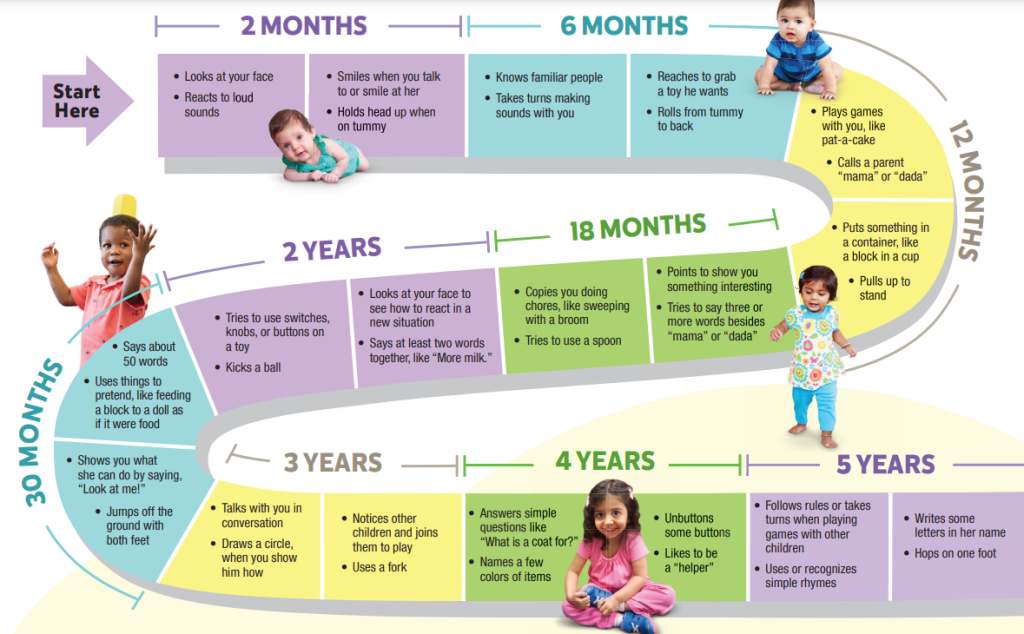
If developmental delays are identified, a health care provider assesses for ASD using information from parents about the child’s behavior and clinical observations using screening tools. If concerns about possible developmental delays are detected during well-child visits, comprehensive evaluations are performed by a health professional specializing in developmental disorders. If a child is diagnosed with a developmental disorder, they are identified as a child with special health care and educational needs, and chronic-condition management is initiated to promote optimal functioning.[12]
Read additional information about Clinical Screening Tools for ASD on the CDC website.
Nurses assess and document signs and behaviors related to an ASD diagnosis. Examples of impaired social communication and social interaction behaviors may include the following[13]:
- No back-and-forth conversation
- Reduced sharing of interests or emotions
- Failure to respond to social interactions
- Making little or inconsistent eye contact
- Lack of facial expressions and nonverbal communication
- Deficits in developing, maintaining, and understanding relationships, such as absence of interest in making friends or sharing imaginative play
Examples of restricted or repetitive patterns of behavior, interests, or activities may include the following[14]:
- Repetitive motor movements, use of objects, or speech (e.g., lining up toys, flipping objects, repeating words or phrases)
- Inflexible adherence to routines
- Insistence on sameness or ritualized patterns of verbal or nonverbal behavior (e.g. extreme distress at small changes, difficulties with transitions, need to eat same food every day)
- Highly restricted, fixated interests that are abnormal in intensity or focus (e.g., strong attachment or preoccupation with unusual objects)
- Hyper- or hyporeactivity to sensory input or unusual interest in sensory aspects of the environment (e.g., apparent indifference to pain/temperature, adverse response to specific sounds or textures, excessive smelling or touching of objects, visual fascination with lights or movement)
Treatment of ASD
Treatments for ASD seek to reduce symptoms that interfere with daily functioning and quality of life. ASD affects each person differently, resulting in different treatment needs. Although ASD is a lifelong disorder, treatments and services can improve a person’s symptoms and optimize their ability to function in their daily life. Treatment plans typically involve multiple interdisciplinary health care professionals with interventions customized to the individual. It is best to start treatment as early as possible to identify the child’s strengths and challenges and plan appropriate services. Research shows children who were diagnosed with ASD and treated early attained better health and well-being outcomes.[15]
Many categories of treatments are available, and some treatments involve more than one approach. Treatment categories include the following:
- Behavioral
- Developmental
- Educational
- Social-Relational
- Pharmacological
Behavioral Approaches
Behavioral approaches focus on changing an individual’s behaviors by promoting understanding of what happens before and after the behavior.
Developmental Approaches
Developmental approaches focus on improving specific developmental skills, such as language or physical skills. Developmental approaches are often combined with behavioral approaches. The most common developmental therapy for people with ASD is speech and language therapy. Speech and language therapy helps improve the client’s understanding and use of speech and language. Some people with ASD communicate verbally. Others with severe symptoms of ASD may communicate through the use of signs, gestures, pictures, or an electronic communication device.
Clients may also participate in occupational and physical therapy. Occupational therapy teaches skills to help clients live as independently as possible. Skills may include dressing, eating, bathing, and relating to other people. Occupational therapy can also include sensory integration therapy to help improve responses to sensory input that may be restrictive or overwhelming. Physical therapy may be used to help improve physical skills, such as fine movements of the fingers or larger movements of the trunk and body.
Educational Approaches
Educational treatments are provided in classroom settings. One type of educational approach incorporates consistency and visual learning. It provides teachers with ways to adjust the classroom structure to improve academic and other outcomes. For example, daily routines can be written and placed in clear sight, boundaries can be set around learning stations, and verbal instructions can be complemented with visual instructions or physical demonstrations.
A student with ASD has an individualized educational plan (IEP) at school created by an interdisciplinary team that determines strategies to best help the student learn. This team includes the child’s parents, case worker, and school staff. This team meets annually and as needed to make changes based on student needs.
Social-Relational Approaches
Social-relational treatments focus on improving social skills and building emotional bonds. For example, “social stories” provide simple descriptions of what to expect in a social situation. “Social skills groups” provide opportunities for people with ASD to practice social skills in a structured environment.
Pharmacological Approaches
There are no medications that cure ASD, but medications may be used to treat symptoms and functioning. For example, medications may be used to manage high energy levels, improve focus and attention problems, reduce irritability or aggression, and limit self-harming behavior, such as head banging or hand biting. Medication may be used to treat concurrent psychological and medical conditions, such as anxiety, depression, seizures, or sleep problems.
Nursing Interventions
Nurses assist clients with ASD and their families as they navigate the health care system to participate in treatments previously discussed.
Nurses are aware that parents and caregivers caring for children or family members with ASD often experience caregiver role strain and teach them about positive coping strategies. Read more about strategies for addressing caregiver role strain in the “Psychosocial Effect of Illness on Client and Family Health” section of the “Family Dynamics” chapter. Nurses teach parents and caregivers about using stress management and healthy coping strategies to manage their emotional responses when caring for a loved one with ASD. Stress management techniques include engaging in regular physical exercise, selecting healthy food choices, setting personal and professional boundaries, and maintaining a healthy social support network. Additional stress management strategies include the techniques of grounding, unhooking, acting on our values, being kind, and making room. Emotion-focused coping refers to strategies used to manage one’s emotional responses, such as participating in mindfulness, meditation, or yoga; using humor and jokes; seeking spiritual or religious pursuits; breathing exercises; and seeking social support.[16] Review additional information about these strategies in the “Stress and Coping” section of the “Mental Health Concepts” chapter.
Nurses refer parents and caregivers to national and local organizations that provide information, community resources, and virtual support groups regarding ASD. See examples of resources in the following box.
Examples of resources for caring for children with autism include the following[17]:
Center for Parent Information and Resources (by state)
- Ernstmeyer, K., & Christman, E. (Eds.). (2022). Nursing: Mental health and community concepts. https://wtcs.pressbooks.pub/nursingmhcc/ ↵
- Maenner, M. J., Warren, Z., & Williams, A. R., et al. (2023). Prevalence and characteristics of autism spectrum disorder among children aged 8 years - Autism and developmental disabilities monitoring network, 11 sites, United States, 2020. MMWR Surveillance Summary 2023, 72(2), 1-14. ↵
- American Psychiatric Association. (2022). Desk reference to the diagnostic criteria from DSM-5-TR (5th ed.). American Psychiatric Association Publishing. ↵
- American Psychiatric Association. (2022). Desk reference to the diagnostic criteria from DSM-5-TR (5th ed.). American Psychiatric Association Publishing. ↵
- U.S. Department of Health and Human Services. (n.d.). Autism spectrum disorder. National Institute of Mental Health. https://www.nimh.nih.gov/health/topics/autism-spectrum-disorders-asd ↵
- American Psychiatric Association. (2024). What is autism spectrum disorder? https://www.psychiatry.org/patients-families/autism/what-is-autism-spectrum-disorder ↵
- “5299266366_0b6c8ae172_o” by hepingting is licensed under CC BY-SA 2.0 ↵
- American Psychiatric Association. (2023, August 22). What is autism? | APA [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=MTW7H5UQ8Ts&t=95s ↵
- National Institute of Mental Health. (2024). Accelerating science to improve early autism screening. https://www.nimh.nih.gov/news/science-news/2024/accelerating-science-to-improve-early-autism-screening ↵
- U.S. Department of Health and Human Services. (n.d.). Autism spectrum disorder. National Institute of Mental Health. https://www.nimh.nih.gov/health/topics/autism-spectrum-disorders-asd ↵
- “Milestone Brochure: Track Your Child’s Developmental Milestones” in the “CDC Milestone Moments Brochure” PDF by the Centers of Disease Control and Prevention is in the Public Domain ↵
- Centers for Disease Control and Prevention. (n.d.). Clinical screening for autism spectrum disorder. https://www.cdc.gov/autism/hcp/diagnosis/screening.html ↵
- American Psychiatric Association. (2022). Desk reference to the diagnostic criteria from DSM-5-TR (5th ed.). American Psychiatric Association Publishing. ↵
- American Psychiatric Association. (2022). Desk reference to the diagnostic criteria from DSM-5-TR (5th ed.). American Psychiatric Association Publishing. ↵
- U.S. Department of Health and Human Services. (n.d.). Autism spectrum disorder. National Institute of Mental Health. https://www.nimh.nih.gov/health/topics/autism-spectrum-disorders-asd ↵
- World Health Organization. (2020). Doing what matters in times of stress. World Health Organization. https://www.who.int/publications/i/item/9789240003927 ↵
- American Psychiatric Association. (2024). What is autism spectrum disorder? https://www.psychiatry.org/patients-families/autism/what-is-autism-spectrum-disorder ↵
A neurodevelopmental disorder that significantly affect a person’s behavior and their ability to socially communicate and interact.

