6.2 Neglect & Abuse
Each state in the United States has its own definitions of child abuse and neglect that are based on standards set by federal law. Federal legislation defines child abuse and neglect as “Any recent act or failure to act on the part of a parent or caretaker which results in death, serious physical or emotional harm, sexual abuse or exploitation, or an act or failure to act, which presents an imminent risk of serious harm.”[1]
Child Neglect and Abuse
Neglect
Neglect is a situation in which a parent or caretaker fails, refuses, or is unable, for reasons other than poverty, to provide the necessary care, food, clothing, or medical or dental care, which seriously endangers the physical, mental, or emotional health of the child. Signs of child neglect include the following[2]:
- Exhibits poor hygiene or body odor
- Is inappropriately dressed for weather
- Demonstrates needed medical or dental care
- Is left alone unsupervised for long periods of time
- Appears malnourished
- Is constantly hungry or begs for or steals food
- Exhibits extreme willingness to please
- Is frequently absent from school
- Arrives early and stays late at school, play areas, or other people’s home
Abuse
Physical abuse is defined as injury inflicted on a child by means other than accidental. Physical injury includes, but is not limited to, lacerations, fractured bones, burns, internal injuries, severe or frequent bruising, or great bodily harm. Signs of physical abuse in children are as follows[3]:
- Bruises and/or welts on face, neck, chest, back, or soft muscle areas less prone to bruising by natural play or accidents (e.g., abdomen, breasts, under arm, inner thigh)
- Injuries in the shape of object (e.g., belt or cord)
- Unexplained burns on palms, soles of feet, or back; a line of demarcation from submerging in hot liquids (e.g., ankles, buttocks, wrists); burns in the shape of object (e.g., fork, cigarette)
- Fractures and injuries that do not fit the story of how an injury occurred
- Delay in seeking medical help
- Behavioral extremes (e.g., very aggressive or withdrawn and shy)
- Frightened to go home
- Frightened of parents
- Fearful of other adults
- Failure to thrive
Some injuries are not visible to observation, such as shaken baby syndrome (now known as abusive head trauma), a serious brain injury resulting from forcefully shaking an infant or toddler.
Sexual Abuse
Sexual abuse is defined as sexual intercourse or sexual touching of a child; sexual exploitation; human trafficking of a child; forced viewing of sexual activity; or permitting, allowing, or encouraging a child to engage in prostitution. In Wisconsin, no child younger than age 15 can consent to sexual contact or intercourse. Signs of sexual abuse in children may include the following[4]:
- Pain, swelling, or itching in genital area
- Bruises, bleeding, discharge in genital area
- Difficulty walking or sitting, frequent urination, or pain
- Stained or bloody underclothing
- Sexually transmitted diseases
- Refusal to take part in gym or other exercises
- Poor peer relationships
- Unusual interest in sex for age
- Drastic change in school achievement
- Runaway or delinquent behavior
- Regression to behaviors expected for a younger child
Emotional Abuse
Emotional abuse is defined as harm to a child’s psychological or intellectual functioning, which is exhibited by severe anxiety, depression, withdrawal, or aggression. Emotional damage may be demonstrated by substantial and observable changes in behavior, emotional response, or learning that is incompatible with the child’s age or stage of development. Signs of emotional abuse in children include the following[5]:
- Low self-esteem
- Self-denigration (belittling or disparaging oneself)
- Severe depression
- Unusual level of aggression
- Severe anxiety
- Extreme withdrawal
- Failure to learn
Child Protective Services
Child Protective Services are available in many states to provide services for children who have been abused or neglected.
Read more about Child Protective Services in your state. Access Wisconsin’s information at Child Protective Services.
Neglect and Abuse of Elders and Adults at Risk
Adults may also experience abuse or neglect. Elder abuse is defined as an intentional act or failure to act (neglect) that causes or creates a risk of harm to an adult age 60 or older.[6] Vulnerable adults who are at risk for abuse are referred to as adults at risk. Adults at risk have a physical or mental condition that impairs their ability to care for their own needs.[7] Older adults and adults at risk are potentially susceptible to abuse, neglect, or financial exploitation by caregivers or a person they trust.[8] A caregiver is a person who has taken responsibility for all or part of an individual’s care.
The following are types of abuse of elders and adults at risk[9]:
- Physical abuse: Physical abuse refers to illness, pain, injury, functional impairment, distress, or death as a result of the intentional use of physical force and includes acts such as hitting, kicking, pushing, slapping, and burning.
- Sexual abuse: Sexual abuse refers to forced or unwanted sexual interaction of any kind. This may include unwanted sexual contact or penetration or non-contact acts such as sexual harassment.
- Emotional abuse: Emotional abuse refers to verbal or nonverbal behaviors that inflict anguish, mental pain, fear, or distress, such as humiliation or disrespect, verbal and nonverbal threats, harassment, and geographic or interpersonal isolation.
- Neglect: Neglect is the failure to meet the person’s basic needs, including food, water, shelter, clothing, hygiene, and essential medical care.
- Financial abuse: Financial abuse is the illegal, unauthorized, or improper use of money, benefits, belongings, property, or assets for the benefit of someone other than the individual.
- Treatment without consent: Treatment without consent refers to the administration of medication or the performance of psychosurgery, electroconvulsive therapy, or experimental research on an individual who has not provided informed consent.
- Unreasonable confinement or restraint: Unreasonable confinement or restraint refers to the intentional and unnecessary confinement of an individual in a locked room, involuntary separation from their living area, use of physical restraints, or the provision of unnecessary or excessive medication. (This does not include the use of these methods or devices if they conform with state and federal standards governing restraint or seclusion.)
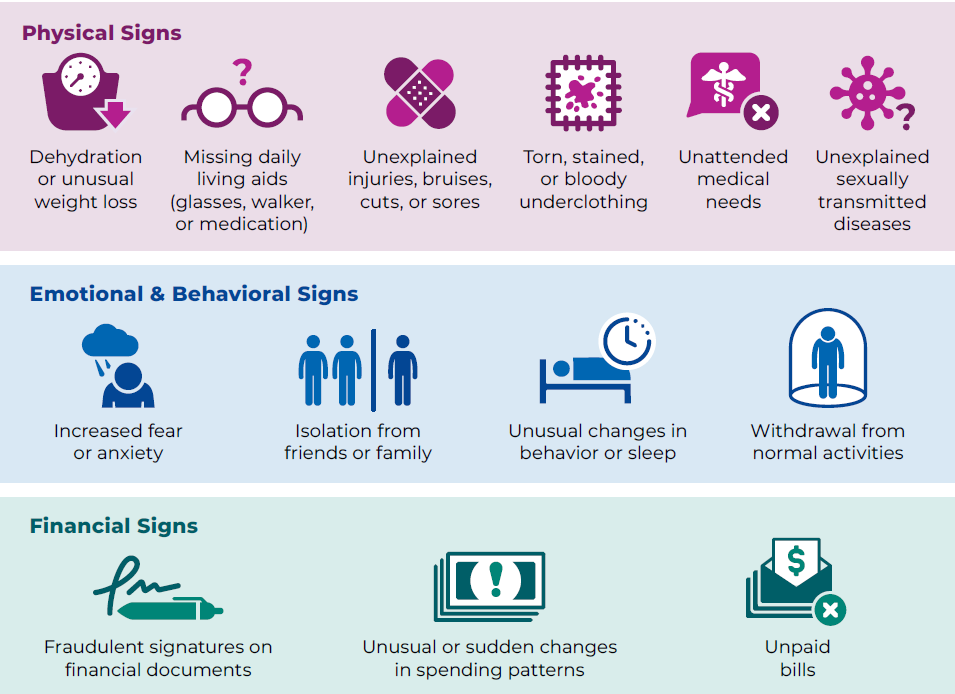
Nurses detect abuse and neglect of elders and adults at risk by noticing the following physical signs[10]:
- Malnutrition, dehydration, or unusual weight loss
- Evidence of self-neglect, including poor diet, poor hygiene, and unattended medical needs
- Sudden mental status changes unrelated to advancing dementia
- Uncontrolled pain despite pharmacological treatment
- Uncontrolled conditions such as hypertension, heart failure, asthma, or diabetes
- Inadequately explained bruises, lacerations, abrasions, fractures, or pressure injuries
- Trauma to genital area or unexplained sexually transmitted infections
Nurses may detect emotional abuse of elders and adults at risk by noticing the following signs[11]:
- Unusual changes in behavior or sleep
- Increased fear or anxiety
- Isolation from friends or family or withdrawal from normal activities
- Client discomfort in the presence of family member/caregiver
Nurses may detect financial abuse of elders and adults at risk by noticing the following signs[12]:
- Unpaid bills
- Fraudulent signatures on financial documents
- Unusual or sudden changes in spending patterns, will, or other financial documents
See Figure 6.1[13] for an infographic describing signs of elder abuse.
Adult Protective Services
Adult Protective Services are available in many states to provide aid to older adults and adults at risk who have been abused, neglected, or exploited. Adult Protective Services are services provided to an individual with a developmental disability, degenerative brain disorder, serious mental illness, or other incapacity to keep them safe from abuse, neglect, or financial exploitation; prevent them from experiencing deterioration; or stop them from inflicting harm on themself or another person.
Research local protective services in your state. Here is the information for the state of Wisconsin’s Adult Protective Services.
Mandatory Reporting
Nurses are mandated reporters who are required by law to report suspected abuse or neglect of children, adults at risk, and the elderly seen during the course of their professional duties. Nurses must be aware of the county or state agencies to whom they should report suspected abuse. For example, in Wisconsin, suspected child neglect or abuse is reported to Child Protective Services (CPS) or law enforcement. Suspected neglect or abuse of the adults at risk is reported to Adult Protective Services or law enforcement. Persons who are mandated to report but intentionally fail to report suspected child abuse or neglect, may be fined up to $1,000 or imprisoned for up to six months or both.[14]
What to Report
Mandatory reporters who suspect child or elder neglect or abuse should contact their county social/human services department, sheriff, or local police department immediately. When making a report, explain what happened or is happening to the child, vulnerable adult, or elderly person. Describe the nature of the abuse or neglect and be as specific as possible. Be prepared to give the name, date of birth (DOB), address, and telephone number of the victim, as well as the name of their parent or caregiver. If you do not know all of this information, report what you do know and explain all you know about the situation and family dynamics.[15]
When a report is filed, the receiving department will make a safety screening determination based on state statutes. If the report meets the criteria for alleged maltreatment, a social worker from the county department of social/human services will proceed with an investigation of the reported maltreatment and assess the situation to determine if any support or assistance is needed to protect the child or vulnerable adult.[16]
Find resources in your area for reporting suspected child abuse at ChildHelp National Child Abuse Hotline.
Reporting to Law Enforcement
Nurses must be aware of the state laws regarding additional mandatory reporting to law enforcement. Examples of what must be reported to law enforcement include child abuse, gunshot or stabbing wounds, suicidal ideation, and homicidal ideation.
Adults who are considered autonomous and competent and are suspected victims of domestic violence (also called intimate partner violence) are often an exception to mandatory reporting laws. Although state law typically requires health professionals to report clients with recent gunshot wounds or other injuries (including some types of burns) suspected to be caused as a result of a crime, other signs or symptoms of suspected domestic violence are not included under mandatory reporting. In fact, reporting suspected domestic violence without the consent of the victim can significantly place the victim (and their children) in danger if they don’t have a safety plan in place. Read more about intimate partner violence and safety plans in the following “Intimate Partner Violence” section.
Read more information about mandatory reporting of domestic violence in your state on the Mandatory Reporter Training website.
Online training on mandatory reporting is available on the Wisconsin Child Welfare Professional Development System website.
- Administration for Children & Families. (2024). Child maltreatment 2023. https://acf.gov/cb/report/child-maltreatment-2023 ↵
- Wisconsin Department of Children and Families. (n.d.). Understanding child abuse and neglect. https://dcf.wisconsin.gov/cps/signs ↵
- Wisconsin Department of Children and Families. (n.d.). Understanding child abuse and neglect. https://dcf.wisconsin.gov/cps/signs ↵
- Wisconsin Department of Children and Families. (n.d.). Understanding child abuse and neglect. https://dcf.wisconsin.gov/cps/signs ↵
- Wisconsin Department of Children and Families. (n.d.). Understanding child abuse and neglect. https://dcf.wisconsin.gov/cps/signs ↵
- Centers for Disease Control and Prevention. (n.d.). About abuse of older persons. https://www.cdc.gov/elder-abuse/about/ ↵
- Wisconsin Department of Health Services. (2024). Adult protective services. https://www.dhs.wisconsin.gov/aps/index.htm ↵
- Centers for Disease Control and Prevention. (n.d.). About abuse of older persons. https://www.cdc.gov/elder-abuse/about/ ↵
- Centers for Disease Control and Prevention. (n.d.). About abuse of older persons. https://www.cdc.gov/elder-abuse/about/ ↵
- National Center on Elder Abuse. (2024). What health care students need to know about elder abuse. [PDF]. https://pfs2.acl.gov/strapib/assets/NCEA_EA_Students_Need_To_Know_Health_Care_D02_8fddf7d4aa.pdf ↵
- National Center on Elder Abuse. (2024). What health care students need to know about elder abuse. [PDF]. https://pfs2.acl.gov/strapib/assets/NCEA_EA_Students_Need_To_Know_Health_Care_D02_8fddf7d4aa.pdf ↵
- National Center on Elder Abuse. (2024). What health care students need to know about elder abuse.[PDF]. https://pfs2.acl.gov/strapib/assets/NCEA_EA_Students_Need_To_Know_Health_Care_D02_8fddf7d4aa.pdf ↵
- “Signs of Elder Abuse” in “Signs of Elder Abuse PDF” by the U.S. Department of Health and Human Services, Administration for Community Living is in the Public Domain. ↵
- Wisconsin Department of Children and Families. (n.d.). Mandated child abuse and neglect reporters. https://dcf.wisconsin.gov/cps/mandatedreporters ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2022). Nursing: Mental health and community concepts. https://wtcs.pressbooks.pub/nursingmhcc/ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2022). Nursing: Mental health and community concepts. https://wtcs.pressbooks.pub/nursingmhcc/ ↵
A situation in which a parent or caretaker fails, refuses, or is unable, for reasons other than poverty, to provide the necessary care, food, clothing, or medical or dental care, which seriously endangers the physical, mental, or emotional health of the client.
Injury inflicted on a child by means other than accidental.
Sexual intercourse or sexual touching of a child; sexual exploitation; human trafficking of a child; forced viewing of sexual activity; or permitting, allowing, or encouraging a child to engage in prostitution.
Harm to a child’s psychological or intellectual functioning, which is exhibited by severe anxiety, depression, withdrawal, or aggression.
An intentional act or failure to act (neglect) that causes or creates a risk of harm to an adult age 60 or older.
Vulnerable adults who are at risk for abuse.
A person who has taken responsibility for all or part of an individual’s care.
The illegal, unauthorized, or improper use of money, benefits, belongings, property, or assets for the benefit of someone other than the individual.
The administration of medication or the performance of psychosurgery, electroconvulsive therapy, or experimental research on an individual who has not provided informed consent.
The intentional and unnecessary confinement of an individual in a locked room, involuntary separation from their living area, use of physical restraints, or the provision of unnecessary or excessive medication.
Required by law to report suspected abuse or neglect of children, adults at risk, and the elderly seen during the course of their professional duties.

