20.8 Exposure to Maternal Substance Use
Neonatal Abstinence Syndromes
Newborns of mothers who consumed substances while pregnant, such as tobacco, alcohol, opioids, marijuana, or other illicit drugs, can experience a variety of withdrawal symptoms after birth, referred to as neonatal abstinence syndrome (NAS). Newborns exposed to alcohol while in utero typically exhibit withdrawal symptoms at only 3 to 12 hours after birth, whereas withdrawal symptoms from other substances such as opioids, benzodiazepines, or tobacco typically begin within 24 to 36 hours after birth.[1]
Withdrawal signs often include irritability with an inability to be consoled, as well as disorganized feeding. Other signs are high-pitched crying, hyperactive reflexes, mild to moderate tremors in one or both hands or feet, increased muscle tone, myoclonic jerks (twitching/jerking) of their limbs or face, hyperthermia, frequent yawning, frequent sneezing, and respiratory distress. Disorganized feeding appears as excessive sucking or uncoordinated sucking, leading to frustration, projectile vomiting, and loose and watery stool. Newborns who experience withdrawal symptoms are at risk for seizures, respiratory distress, and failure to thrive. Table 20.8 lists the neurologic signs of withdrawal symptoms from various substances.
Table 20.8. Neurological Signs of Drug Withdrawal in Newborns[2]
| Maternal or Medical Substance | Neurologic Symptoms in Newborn |
|---|---|
| Nicotine | Increased Moro reflex, excessive high-pitched cry, tremors, sleep problems, hypertonia, seizures, fever, inconsolability |
| Alcohol | High-pitched cry, sleep problems, decreased suck reflex, poor coordination with feeding, hyperreflexia, inconsolability |
| Marijuana | Jitteriness and irritability |
| Opioids | Tremors, hyperreflexia, hypertonia, inconsolability, high-pitched cry, poor coordination with feeds, respiratory distress, sleep problems, diarrhea, sneezing, jaundice, seizures, death |
| Cocaine | Tremors, hyperreflexia, hypertonia, inconsolability, high-pitched cry, poor coordination with feeds, respiratory distress, sleep problems, diarrhea, sneezing, jaundice, seizures, death |
| Benzodiazepines | Tremors, hyperreflexia, hypertonia, inconsolability, high-pitched cry, poor coordination with feeds, respiratory distress, sleep problems, diarrhea, sneezing, jaundice, seizures, death |
If a newborn is exhibiting withdrawal symptoms, nurses can use standardized tools like the Finnegan Neonatal Abstinence Scoring Tool to determine how to manage care. Scoring on the tool helps nurses and health care providers evaluate the severity of withdrawal symptoms and the need for more intense intervention in the NICU. Agencies have slightly different protocols for managing infants with NAS. One example is the Finnegan Management Algorithm to manage the newborn’s withdrawal symptoms with medication to prevent complications. Treatment may include benzodiazepines, alpha adrenergics, or weaning off the opioid over time. Serial scores are then used to evaluate the infant’s progress.
View The Finnegan Neonatal Abstinence Scoring Tool for evaluating and monitoring neonates who are experiencing substance withdrawal, as well as a sample protocol for managing NAS.
View a supplementary YouTube video[3] on neonatal abstinence syndrome at Neonatal Abstinence Syndrome | Cincinnati Children’s.
Fetal Alcohol Spectrum Disorders
Fetal alcohol spectrum disorders (FASDs) are a group of conditions that can occur in an infant who was exposed to alcohol before birth. The developing fetus experiences higher concentrations of alcohol than the pregnant woman because the fetus metabolizes alcohol more slowly than an adult. The more alcohol that is ingested by the mother, the greater the risk to the fetus. Alcohol affects all the developing fetal tissues and interferes with oxygen delivery and nutritional intake. Effects can range from growth deficits to physical abnormalities, neurocognitive and behavioral deficits, and an increased vulnerability to mental health problems later in life.[4]
Many factors affect the developmental and health status of the infant with FASD, such as genetic susceptibility, the mother’s drinking pattern and the amount consumed, the timing of drinking in relation to fetal development stage, and the mother’s metabolism and tolerance of alcohol during the pregnancy. Recent research findings suggest that prenatal alcohol exposure may also affect the regulation of gene expression.[5]
FASD diagnoses are based on the symptoms displayed, such as the following[6]:
- Alcohol-related birth defects: A range of congenital and genetic birth defects caused by maternal alcohol consumption during pregnancy.
- Neurodevelopmental disorders associated with prenatal alcohol exposure: Behavioral and neurocognitive impairments caused by maternal alcohol consumption during pregnancy, such as mental health conditions, long- and short-term memory loss, impulse control, and impaired communication.
- Fetal alcohol syndrome: A severe presentation that includes both neurodevelopmental disorders and birth defects caused by maternal alcohol consumption during pregnancy. This diagnosis includes characteristic facial features and central nervous system deficits.
Signs of FASD in an infant include the following[7]:
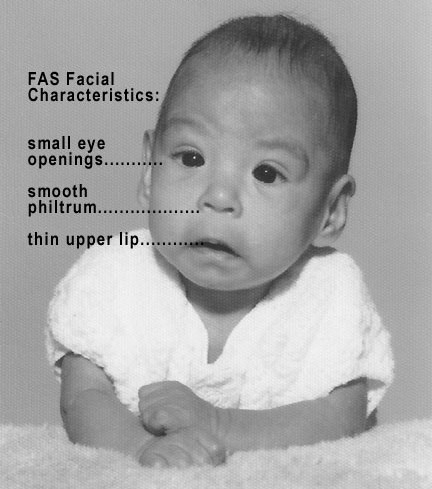
- Three specific facial abnormalities: Smooth philtrum (the area between nose and upper lip), thin upper lip, and small palpebral fissures (horizontal eye openings). See Figure 20.13[8] for an image of an infant with FASD.
- Growth deficit (lower than average length, weight, or both).
- Central nervous system (CNS) abnormalities.
There is no specific treatment for FASD, but the earlier it is diagnosed in an infant, the sooner that supportive services can be implemented. Physical and neurodevelopmental impairments resulting from FASD can be ongoing, requiring a lifetime of coordinated medical care and support. The goal of treatment is to reduce the effects of the syndrome. Every child presenting with FASD has their own personalized needs, such as optometry for vision care or a cardiologist consult for cardiovascular health. Early developmental services such as speech therapy, physical therapy, and occupational therapy can help promote basic gross motor, fine motor, and language skills and reduce the effects of FASD. Later in childhood, school supportive services can help with learning and possible behavioral issues.[9]
Nursing management includes preventing overstimulation because newborns with FASD can become easily agitated with difficulty self-soothing. Maintaining an environment that is calm and clustering cares help reduce physical stimulation. The nurse also provides health teaching to the birth parents, along with referrals to counseling, alcohol cessation programs, and support groups. Nurses may also assist with contacting social services if agency policy indicates consulting child protective services for newborns diagnosed with FASD. In many states, children born with FASD are automatically eligible for intervention services.[10]
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/details/books/maternal-newborn-nursing ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/details/books/maternal-newborn-nursing ↵
- Cincinnati Children's. (2017, March 3). Neonatal abstinence syndrome | Cincinnati Children's [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=yr-kLlwNexs ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/details/books/maternal-newborn-nursing ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/details/books/maternal-newborn-nursing ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/details/books/maternal-newborn-nursing ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/details/books/maternal-newborn-nursing ↵
- “Photo_of_baby_with_FAS” by Teresa Kellerman is licensed under CC BY-SA 3.0 ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/details/books/maternal-newborn-nursing ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/details/books/maternal-newborn-nursing ↵
A group of withdrawal symptoms experienced by newborns exposed to addictive substances, such as opioids, in utero.
A condition in which newborns exhibit difficulty with feeding, often due to neurological or sensory issues, leading to inconsistent sucking and swallowing.
A range of physical, behavioral, and cognitive disabilities in a child caused by alcohol exposure during pregnancy.

