18.18 Polycystic Ovary Syndrome
Polycystic ovary syndrome (PCOS) is a common endocrine disorder that causes women to not ovulate or to ovulate infrequently. PCOS is characterized by hormonal imbalances that cause reproductive, metabolic, and cardiovascular disorders with multiple symptoms that affect a woman’s health beyond their reproductive years. The cause of PCOS is not fully understood, but researchers have observed a pattern of elevated androgen levels and insulin resistance in people with the condition. Researchers are also investigating how genetics may contribute to developing this disease, as many people with PCOS have relatives with this disorder.[1]
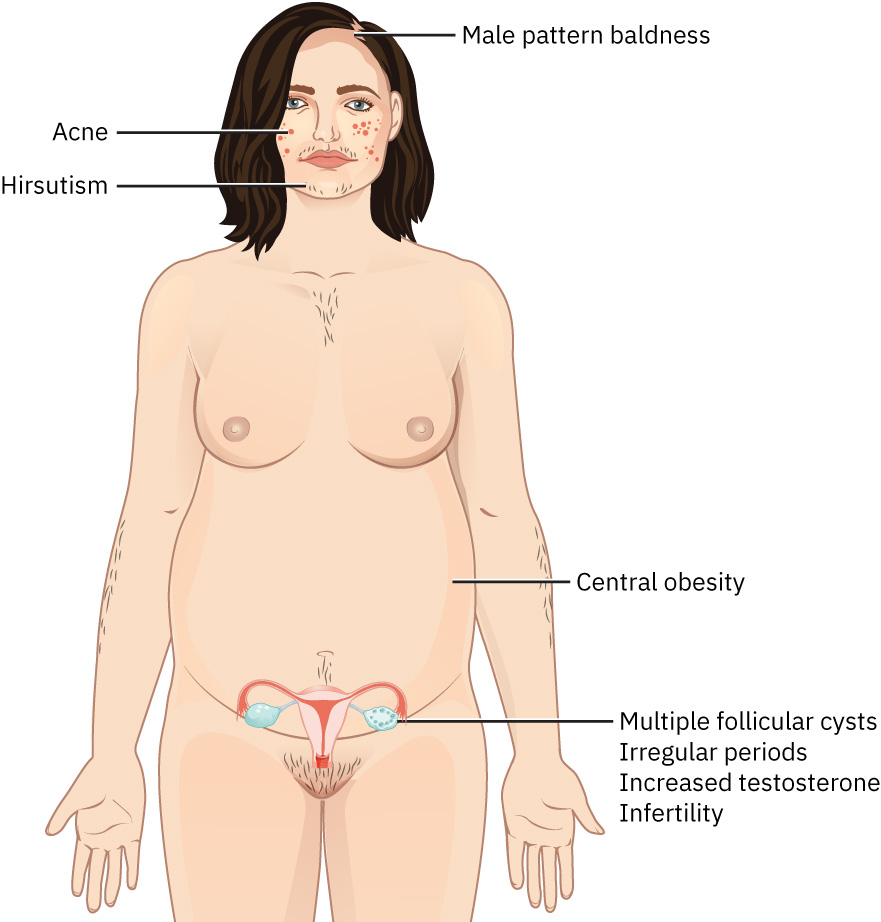
The symptoms of PCOS are diverse and vary significantly from person to person. Many people do not realize they have PCOS until they struggle to conceive. Other people have the full spectrum of clinical manifestations, which can include the following[2]:
- Irregular menstrual cycles
- Hyperandrogenism, causing hirsutism (a condition in which women develop excessive hair growth in areas where men typically grow hair, such as the face, chest, and back), acne, and alopecia (hair loss on the scalp)
- Multiple follicular cysts on the ovaries, as viewed on ultrasound
- Central obesity
- Infertility
See Figure 18.18[3] for an illustration of common signs of PCOS.
Women with PCOS are at risk for several serious complications, including the following[4]:
- Insulin resistance and diabetes
- Metabolic syndrome
- Hypertension
- High cholesterol and triglycerides
- Endometrial cancer due to excessive endometrial growth from irregular menstrual cycles
- Depression and anxiety
- Obstructive sleep apnea related to being overweight
- Cardiovascular disease
- Nonalcoholic fatty liver disease
Women with PCOS who become pregnant are at higher risk for complications such as gestational diabetes, preeclampsia, and preterm birth.[5]
Diagnosing PCOS involves a thorough assessment of a client’s medical history and clinical symptoms, as well as diagnostic testing. The diagnostic tool for PCOS is the Rotterdam criteria, which require the presence of two out of three of the following factors: menstrual irregularity, evidence of hyperandrogenism (by either clinical symptoms or laboratory testing), and polycystic ovaries visualized on ultrasound. To be diagnostic of PCOS, these symptoms must also occur without any other clinical cause. Blood tests can be used to rule out other diagnoses, including pregnancy, elevated prolactin levels, and abnormal levels of thyroid hormones and follicle-stimulating hormone. Testing of androgen levels, such as testosterone and dehydroepiandrosterone sulfate (DHEAS), may also aid in the diagnosis. After diagnosis of PCOS, clients may undergo additional testing for insulin resistance, diabetes, and cholesterol/triglyceride levels to determine if other complications are present.[6]
Medical treatment of PCOS focuses on alleviating symptoms, improving metabolic outcomes, and addressing reproductive concerns. Combined estrogen-progesterone oral contraceptives in the form of pills, patches, or the vaginal ring are frequently used to help regulate menstrual cycles, lower the risk of endometrial hyperplasia, and reduce hyperandrogenism. Aldosterone receptor antagonists, such as spironolactone, may be prescribed to help reduce symptoms of hyperandrogenism, such as hirsutism and acne. Weight loss is a common concern that may require prescription medications to reduce insulin resistance. Metformin, a biguanide, can be effective in improving cellular sensitivity to insulin and may help restore ovulation in women with abnormal menstrual cycles. Hair loss may be treated with medications such as minoxidil or hair replacement therapies.[7]
Nurses teach clients about PCOS and potential complications while also promoting lifestyle modifications for improving health and fertility outcomes. Regular physical activity and a healthy diet can help manage weight loss, reduce insulin resistance, and promote overall well-being, with even modest amounts of weight loss leading to improvements in menstrual regularity, hormonal profiles, and fertility. Clients may also elect to use hair removal therapies, such as depilatories, laser therapy, waxing or shaving, and electrolysis, to remove excess body hair associated with PCOS.[8]
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- “420f0d8bc7bb4eabbc0fbc91f80cec287b7fbd1b” by Rice University/Open Stax is licensed under CC BY 4.0. https://openstax.org/books/maternal-newborn-nursing/pages/6-1-functional-disorders ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
A condition that causes women to not ovulate or to ovulate irregularly.
A condition in which women develop excessive hair growth in areas where men typically grow hair, such as the face, chest, and back. It is often caused by elevated androgen levels, as seen in conditions like PCOS.
Hair loss on the scalp.

