16.22 Other Pediatric Disorders
A brief overview of other common pediatric disorders are discussed in the following subsections.
Acne Vulgaris
The content in this section is adapted from StatPearls.[1]
Acne vulgaris, commonly known as acne, is a common chronic skin condition in adolescents that can affect clients of any age. Acne is also more common in adolescent males and in urban populations. Females may experience acne flare-ups associated with menstruation.
Acne is a result of androgens and the presence of the bacteria Cutibacterium acnes. Androgens can bind to oil-producing glands, causing increased production of oil and subsequent acne formation. The excess oil provides an excellent medium for the growth of bacteria such as C. acnes. The presence of bacteria triggers inflammation and the immune response, leading to pustules, papules, and nodules associated with acne.
Risk factors for developing acne include certain medications (lithium, steroids, and seizure medications), excessive sunlight exposure, genetics, the use of oil-based makeup, and increased stress levels.
Acne mostly occurs on the face, but it may also be present on the arms, trunk, neck, or buttocks. When present, it ranges greatly in severity and is graded along a continuum. Acne can consist of comedones that can be open or closed. An open comedone is also known as a blackhead, whereas a closed comedone is also known as a whitehead. If it becomes more severe, acne can form small inflamed papules or pustules. Many pustules can lead to the formation of nodules or cysts. As acne heals, it may cause scarring or hyperpigmentation. See Figure 16.30[2] for an image of a male client with acne on their forehead.

Acne is a clinical diagnosis. Further testing may be performed if acne is associated with abnormal androgen levels or other medical conditions.
Acne treatment depends on the severity, as well as the psychological state of the client. Mild cases are treated with topical medications such as antibiotics, salicylic acid, or retinoids. More severe cases of acne are treated with a combination of topical and oral medications. Oral medications consist of antibiotics, isotretinoin, spironolactone, or oral contraceptives for female clients. Medications suppress acne formation but do not cure acne, so follow-up treatment may be needed. Clients with severe acne should be referred to a dermatologist.
In addition to teaching about medications, nurses also teach about proper skin care. The client should use gentle skin cleansers and avoid acne-producing skin products, as well as picking at their acne lesions.
Amblyopia
The content in this subsection is adapted from StatPearls and Cleveland Clinic.[3],[4]
Amblyopia, commonly known as a lazy eye, is a disorder caused by abnormal development of the eyes. It usually only affects one eye, but both eyes can be affected. Amblyopia can be caused by uncorrected hyperopia or myopia, visual deprivation, strabismus, or when eyes have a significant difference in visual acuity. Other risk factors are premature birth; family history; or maternal use of tobacco, alcohol, or drugs during pregnancy.
The pathophysiology of amblyopia is dependent on the specific causes of the disorder. For example, if untreated refractive errors cause a significant difference in visual acuity between eyes, the brain begins to ignore the weaker eye and eye muscles cause it to wander out of its normal position. Amblyopia can also cause decreased vision in the affected eye. Children with amblyopia may be observed squinting or shutting one eye, tilting their head to the side, or favoring one side of their body. If not treated early, the client may have vision damage that is irreversible.
Amblyopia is diagnosed clinically, but further testing may be done to determine the specific cause of the disorder or rule out underlying conditions.
Amblyopia treatment is determined by the initial cause of the disorder. Potential treatments are the corrective lenses, an eye patch, medications, or surgical procedures. An eye patch may be placed on the unaffected eye to encourage use and strengthening of the affected eye. Atropine eye drops may be prescribed for the unaffected eye, causing blurry vision in the unaffected eye, which encourages the brain to use the affected eye.
Blepharitis
The content in this section is adapted from StatPearls.[5]
Blepharitis is an acute or chronic inflammation of the margins of the eyelid. The cause of blepharitis depends on whether it is an acute or chronic case. Acute cases due to an infectious cause are considered ulcerative blepharitis. Common infectious causes are staphylococcal bacteria, herpes simplex virus, or varicella-zoster virus. Acute nonulcerative blepharitis is usually caused by an allergic reaction. Chronic cases of blepharitis can be linked to infection, seborrheic dermatitis, rosacea, hormone imbalances, or overproduction of oil by the meibomian glands.
Blepharitis is more common in the adult population, but it can affect pediatric clients. Symptoms are typically worse in the morning and can be intermittent. Both eyes are generally affected. Common signs and symptoms of blepharitis are as follows:
- Itchy, burning eyes
- Eyelid crusting
- Tearing
- Blurred vision
- A reported sensation of a foreign body in the eye
See Figure 16.31[6] for an image of eyelid crusting due to blepharitis.
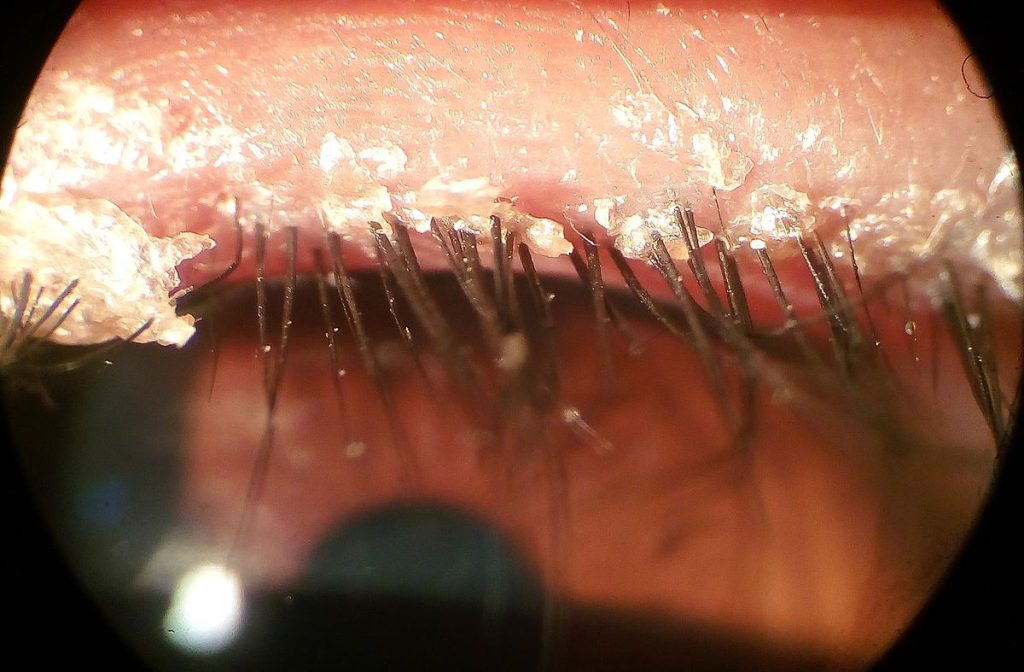
Other signs and symptoms are specific to the type of blepharitis. For example, clients with anterior blepharitis often have edematous and reddened eyelids, loss of eyelashes, loss of eyelash pigmentation, and abnormal eyelash direction. In posterior blepharitis, the meibomian glands will be covered in oil and have thick secretions. The glands may also be dilated or obstructed.
Potential complications of blepharitis consist of scarring of the eyelids, formation of a hordeolum or chalazion, corneal ulcerations, chronic inflammation of the conjunctiva, and vision loss.
Blepharitis is a clinical diagnosis. However, biopsies are performed in cases of treatment failure to rule out cancerous causes.
Treatment of blepharitis consists of eyelid hygiene. Warm compresses are applied to the eyes to loosen secretions, and the eyelids should be washed with diluted baby shampoo. Eyelid massage can also be beneficial in those with blepharitis due to meibomian gland malfunction. Additionally, eye makeup should be avoided. Clients with chronic blepharitis must maintain this eyelid hygiene routine for life to prevent flare-ups.
Topical antibiotics may be prescribed for acute bacterial blepharitis and some cases of chronic blepharitis. Topical steroids may also be prescribed to reduce symptoms. Clients who do not obtain relief with these treatments should be referred to an ophthalmologist. A variety of new treatments are being researched that involve heat or light therapy to treat blepharitis.
Cellulitis
The content in this subsection is adapted from StatPearls.[7]
Cellulitis is a common acute bacterial infection of the dermis and subcutaneous layers of the skin. Cellulitis can occur anywhere on the body but is typically seen on the lower extremities. Cellulitis is commonly caused by Streptococcus pyogenes and Staphylococcus aureus, but it can be linked to other bacteria as well. Risk factors for the development of cellulitis include the presence of any breaks in the skin, as well as coexisting medical conditions of diabetes, peripheral vascular disease, or lymphedema.
When a break occurs in the skin, bacterial pathogens can enter, triggering an immune response with the release of cytokines and neutrophils in the afflicted area and causing characteristic symptoms. If the causative bacteria produces toxins, the resulting cellulitis will be more severe.
Characteristic symptoms of cellulitis include a poorly defined area of skin that is red, warm, swollen, and tender to the touch. See Figure 16.32[8] for an image of a client with cellulitis of the lower leg. Swelling can also lead to the formation of fluid-filled blisters in the affected area. Clients may also exhibit malaise, fever, or fatigue. Potential complications include abscess formation, enlarged lymph nodes, bacteremia, sepsis, endocarditis, and osteomyelitis.

Cellulitis is a clinical diagnosis that can be made when two of the four hallmark signs are present, including warmth, redness, swelling, and pain. While assessing the client, the nurse should attempt to ascertain the source of the infection by looking for open areas. Blood cultures may be performed for clients who are immunodeficient, were bitten by an animal, were injured during water exposure, or are experiencing signs of a widespread infection.
Treatment of cellulitis consists of antibiotics. Clients with mild cases can be treated with oral antibiotics, but more severe cases require hospitalization and intravenous antibiotics. Hospitalization is recommended for clients with signs of systemic infection, those who have not improved with oral antibiotics, immunocompromised clients, or cellulitis that is rapidly spreading. The afflicted area should be outlined with a permanent marker so staff can monitor for continued spread. Elevating the affected limb can reduce edema.
Cerebral Palsy
The content in this section is adapted from the CDC.[9]
Cerebral palsy (CP) is a group of disorders that affects the ability to move and maintain balance and posture. CP is the most common motor disability in childhood. Cerebral means having to do with the brain, and palsy means weakness or problems with using the muscles. CP is caused by abnormal brain development or damage to the developing brain that affects the ability to control muscles.
Symptoms of CP vary from person to person. A person with severe CP might require the use of special equipment to walk or might not be able to walk at all and need lifelong care. A person with mild CP, on the other hand, might walk a little awkwardly, but otherwise not require specialized care. Doctors classify CP according to the main type of movement disorder involved. Depending on which areas of the brain are affected, one or more of the following movement disorders can occur:
- Spasticity: Stiff muscles
- Dyskinesia: Uncontrollable movements
- Ataxia: Poor balance and coordination
There is no cure for CP, but treatment can improve the quality of life for people who have the condition. After CP is diagnosed, a team of health professionals works with the child and family to develop a plan to help the child reach their optimal potential. Common treatments include medications; surgery; braces; and physical, occupational, and speech therapy.
Chalazion
The content in this subsection is adapted from StatPearls and Cleveland Clinic.[10],[11]
A chalazion is a noninfectious, inflammatory lesion of the meibomian or Zeis glands of the eye. A chalazion forms when one of these oil-producing glands becomes blocked. Once the gland is blocked, oil cannot drain, and the gland becomes swollen and inflamed. When the meibomian gland is affected, it is considered a deep chalazion, and if the Zeis gland is affected, it is considered a superficial chalazion. Chalazia are a common condition in adults and can also be seen in children.
A chalazion commonly presents as a unilateral, non-reddened, pain-free swelling of the eyelid. The lesion is usually solitary and on the upper eyelid. See Figure 16.33[12] for an image of a chalazion. Sometimes vision issues or corneal abrasions can occur with a larger chalazion. There is the potential for the chalazion to become infected, leading to pain. Infection can also progress to cellulitis.

Chalazia are diagnosed clinically. When examining the client, their eyelid should be everted to assess for an internal chalazion. Because chalazia tend to recur, the client should also be assessed for a history of similar lesions. If the diagnosis is unclear or if the chalazion continues to recur, a biopsy of the lesion may be recommended to rule out a cancerous etiology.
Treatment of chalazia consists of warm compresses and eyelid massage. The client should be referred to an ophthalmologist if the chalazion does not heal within a month because surgical management may be necessary. Antibiotics are generally not prescribed, as this is not an infectious condition. Steroids may be injected directly into the lesion by a health care provider, but only if there is no infection present. Clients and their parents/caretakers can be educated that regular cleaning of the eyelids is thought to help prevent the development of chalazia.
Cognitive Impairment
The content in this subsection is adapted from StatPearls.[13]
A client with cognitive impairment has deficits in intellectual functioning, as well as adaptive behavior. Intellectual functioning consists of problem-solving skills, as well as the ability to learn, reason, and communicate. Adaptive behavior refers to social skills, the ability to grasp concepts such as time and finance, and practical skills or the ability to use tools and complete activities of daily living (ADLs).
The causes of cognitive impairment are varied, but most pediatric cases are caused by genetics or environmental exposure. Examples of genetic conditions causing cognitive impairment are phenylketonuria or Fragile X syndrome. Examples of environmental exposures that can lead to intellectual impairment are fetal exposure to alcohol, drugs, or certain viruses.
When assessing a pediatric client with a potential cognitive impairment, it is essential to first rule out neurological, vision, or hearing disorders that could mimic an intellectual impairment. Although the signs of symptoms of intellectual impairment vary widely based on the specific disorder, common signs and symptoms include the following:
- Difficulty completing ADLs
- Poor impulse control
- Poor communication or delay in language skills
- Difficulty in school performance
- Delays in motor skills or motor dysfunction
Cognitive impairment can be diagnosed by the administration of an IQ test by a trained professional. An IQ of 70 or below is suggestive of an intellectual impairment. However, the diagnosis must also take the client’s adaptive functioning into account. This can be done with standardized testing tools that measure the ability of the client to function independently and socially. Further testing may be done to ascertain the specific etiology of the client’s intellectual impairment.
Treatment for intellectual impairment varies widely but consists of educational support for the client and their family, behavioral therapy, family therapy, and vocational training. Medications may be prescribed for clients with aggressive behaviors, depression, involuntary movements, or comorbidities.
Color Blindness
The content in this section is adapted from the American Academy of Ophthalmology.[14]
Color blindness, also known as color deficiency, is when colors are seen abnormally. Color blindness is usually a genetic condition that is present at birth in which cones in the retina are completely or partially absent. Color blindness can also be acquired from trauma to the eye and is also associated with specific disorders such as alcoholism and diabetes.
Symptoms can range in severity and include the following:
- Issues with seeing colors or color brightness
- Inability to distinguish between similar shades of colors such as red and green or blue and yellow
- Difficulty learning colors in children
In a healthy retina, light is detected by rods and cones. Rods help distinguish between light and dark, whereas cones are used for color vision. There are three types of cones that allow for the detection of color, including red, green and blue. When cones are not present or do not work appropriately, color blindness can result.
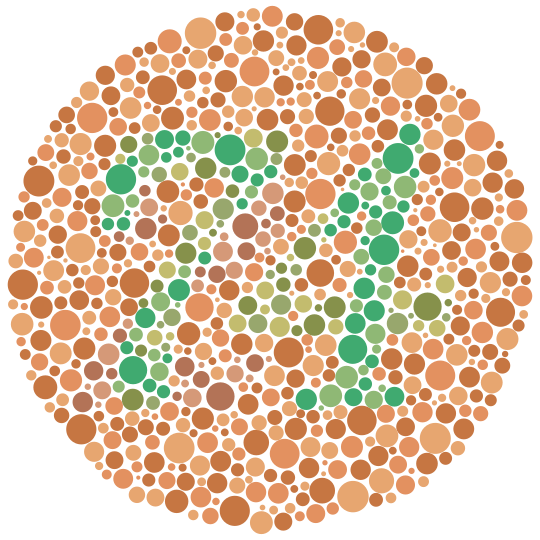
Color blindness can be diagnosed by a test where clients are shown patterns consisting of dots in a variety of colors. Clients with color blindness are unable to decipher the number or shape that is present in the dots. See Figure 16.34[15] for an example of this type of test.
Congenital color blindness cannot be cured. However, special lenses are available to help the client distinguish colors. If color blindness is an acquired condition, treating the underlying condition may improve color vision.
Community-Acquired MRSA
The content in this section is adapted from StatPearls and Cedar Sinai.[16],[17]
Methicillin-resistant Staphylococcus aureus (MRSA) is bacteria that is resistant to commonly used antibiotics. MRSA infection can be subdivided into two categories called hospital-associated MRSA (HA-MRSA) or community-acquired MRSA (CA-MRSA). The focus of this subsection will be CA-MRSA, which has been on the rise in recent years. Clients at risk for contracting CA-MRSA are those with breaks in the skin due to injury, tattoos, or piercings; those who have close contact with others who are colonized or infected with MRSA; and those who share equipment or supplies that are not cleaned effectively between uses. CA-MRSA is also commonly seen in clients who live or work in close quarters such as athletic teams, military barracks, or prisons.
The skin and nose of many individuals may be colonized with MRSA, but this is not the same as an active infection. People who are colonized with MRSA often do not have any signs or symptoms unless MRSA finds its way into an open wound or they become immunocompromised.
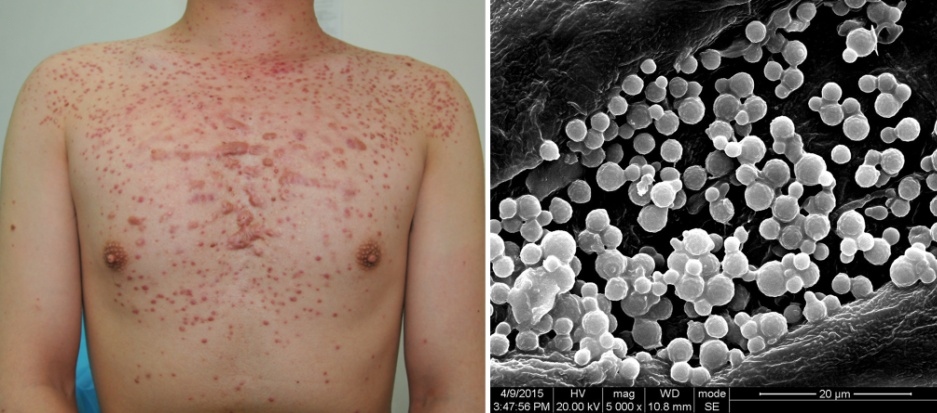
Clients with active MRSA infection can experience a wide variety of symptoms. CA-MRSA commonly causes infections of the skin and soft tissue. Examples of skin and soft tissue infections caused by CA-MRSA are cellulitis, necrotizing fasciitis, and ulcers in the feet of diabetic clients. CA-MRSA can also cause small pimple-like lumps or even larger abscesses that drain pus. See Figure 16.35[18] for an image of an abscess caused by MRSA.

CA-MRSA can also spread via the blood or by direct invasion and lead to more serious issues. For instance, CA-MRSA can spread to the bones and lead to osteomyelitis or spread to the lungs and cause pneumonia.
CA-MRSA can be diagnosed by culturing bodily fluids such as wound exudate, blood, sputum, or urine. If cultures are inconclusive, a PCR test can also be performed to detect MRSA. Additionally, swabs of the nares can undergo PCR testing to determine if someone is colonized with MRSA. Other diagnostics may be done based on the specific site of infection.
Treatment of CA-MRSA consists of antibiotics with the specific antibiotic based on what type of infection is present, the resistance profile of the bacteria, and the status of the client. A health care provider who specializes in infectious diseases may be consulted. In some cases, where the infection is localized to a small pimple or abscess, the lesion may be drained, and antibiotics may not be prescribed. In severe cases, hospitalized clients should have contact transmission-based precautions implemented to prevent the spread of infection.
Clients and their parents/caretakers should be educated on ways to prevent CA-MRSA, including good hand hygiene and respiratory etiquette, keeping open wounds covered, not sharing personal items such as towels, and taking a shower after team sports.
Congenital Heart Defects
Content in this subsection is adopted from StatPearls and Nurse Together.[19],[20],[21],[22]
A congenital heart defect is a structural defect of the heart that is present at birth. These heart defects range in severity and may or may not require surgical interventions. The exact cause for each type of congenital heart defect is unknown, but some risk factors have been recognized. Maternal rubella and diabetes have been shown to increase the risk of congenital heart defects, as well as smoking and alcohol use during pregnancy. Certain medications can also increase the risk, such as angiotensin-converting enzyme inhibitors, statins, and isotretinoin. Congenital heart defects also have a genetic link.
There are a variety of congenital heart defects but some of the more common are listed here:
- Atrial septal defect (ASD) occurs when there is a hole between the two atria of the heart.
- Ventral septal defect (VSD) is when there is a hole between the two ventricles of the heart.
- Patent ductus arteriosus (PDA) is failure of the ductus arteriosus to close at birth.
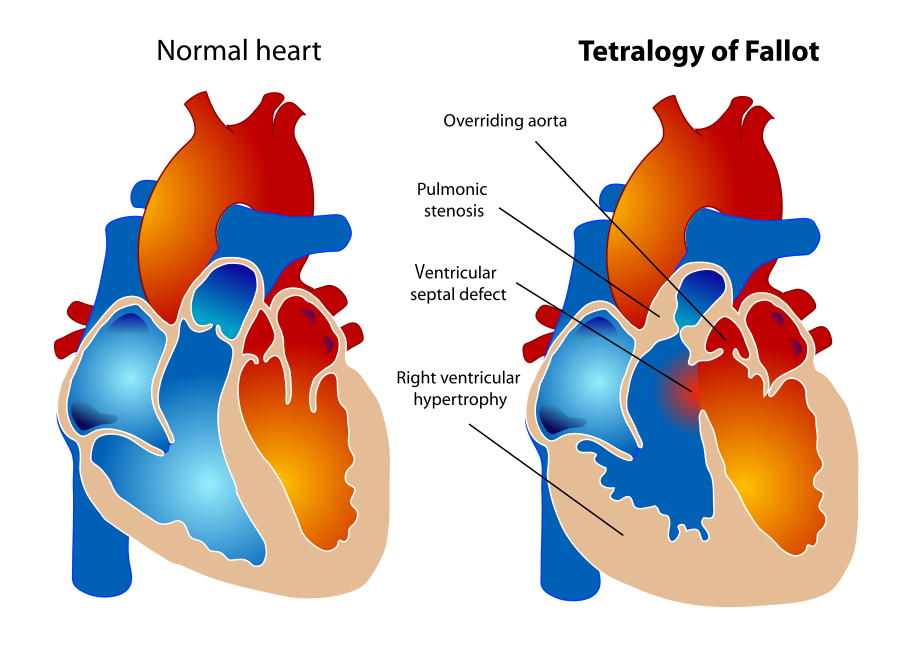
- Tetralogy of Fallot (TOF) is a combination of four different congenital heart defects in which there is a ventral septal defect, hypertrophy of the right ventricle, narrowing of the pulmonic valve, and a displaced aorta. See Figure 16.36[23] for an image of a healthy heart compared to a client with TOF.
Potential complications of a congenital heart defect include heart failure, endocarditis, cardiac dysrhythmias, impaired growth and development, stroke, and mental health disorders such as anxiety and depression.
Common symptoms of congenital heart defects in infants are cyanosis; increased respiratory rate; edema in the legs, abdomen, or around the eyes; and shortness of breath. Shortness of breath impacts feeding, which can lead to poor weight gain. Signs and symptoms in older pediatric clients consist of fainting during physical activity; becoming tired or short of breath with physical activity; and edema of the feet, ankles, and hands. Some pediatric clients with congenital heart defects may also have a murmur. Pediatric clients may naturally assume a squatting position when feeling short of breath to increase pulmonary blood flow.
Tet spells can occur in clients with TOF and are characterized by worsening cyanosis, increased respiratory rate, increase in respiratory depth, syncope, and cardiac arrest. Tet spells can be triggered by crying, feeding, or agitation.
Diagnostic testing for congenital heart disease may include pulse oximetry, electrocardiogram, echocardiogram, chest X-ray, cardiac MRI, or a cardiac catheterization.
Treatment for a congenital heart defect varies widely based on the specific defect and its severity. Some mild defects do not require treatment. Treatment for severe defects can consist of cardiac medications, procedures, or surgeries. With some congenital heart defects, particularly TOF, client positioning can be used to help manage symptoms. The client can be placed on their left side with their knees brought to their chest to help increase pulmonary blood flow.
Lifestyle modifications are recommended based on the type of congenital heart defect. For example, physical activity or participation in sports may need to be limited. Additionally, due to the increased risk of endocarditis with some congenital heart defects, prophylactic antibiotics may be required before dental work or invasive medical procedures. Nurses can also recommend support groups to help the client and their families cope with their diagnosis.
Congenital heart defects and their treatments are discussed in greater detail in the “Congenital Heart Defects” chapter.
Cytomegalovirus
The content in this subsection is adapted from StatPearls.[24]
Cytomegalovirus (CMV) is a virus in the herpes family of viruses. When infected with CMV, clients can have a wide range of symptoms, ranging from being asymptomatic to death. CMV infection is of particular concern for those who are immunocompromised or pregnant.
CMV can be spread from blood or organ transplants, via breast milk from mother to fetus, or from close contact with an infected individual. Once infected, a primary infection results, but the client may or may not have symptoms. Similar to other viruses in the herpes family, CMV remains latent in the body after initial infection, and reactivation can occur at a later date during a period of immunosuppression.
Signs and symptoms of CMV vary widely. A common presentation in otherwise healthy clients is mononucleosis, an elevated temperature, a rash, and elevated white blood cell counts. In clients who are immunocompromised, CMV infection tends to be severe and afflict multiple organs, leading to liver failure, inflammation of the colon or lungs, and encephalitis. Clients with a history of organ transplant tend to have recurrences of CMV. When CMV is spread from mother to fetus, the child can experience deafness, developmental delays, or death.
CMV virus can be detected via PCR testing, but this testing is typically only performed for clients with immunodeficiency.
Clients who have few symptoms related to CMV infection typically only require supportive care. However, clients with severe cases or who are immunocompromised are prescribed antiviral medications. Although most clients with CMV have a good prognosis, they may experience fatigue for many months after the initial infection.
Duchenne’s Muscular Dystrophy
The content in this subsection is adapted from StatPearls.[25]
Duchenne’s muscular dystrophy (DMD) is a severe form of muscular dystrophy with most clients dying in their twenties due to complications. It is caused by a mutation in the dystrophin gene, which leads to progressive muscle breakdown and weakness. This genetic mutation is usually inherited but can also be caused by a new mutation. DMD is more common in males than females.
With DMD, muscle tissue continuously dies and regenerates. With time, this muscle tissue is replaced with connective and fatty tissues instead, leading to the signs and symptoms associated with this disease. However, dystrophin is also present in brain and eye tissue, so the central nervous system can be affected, along with the musculoskeletal system.
DMD is a progressive disorder, but signs are not usually present in the first few years after birth. Between two and three years of age, muscle weakness and difficulty walking may be noted. Children may be unable to run or climb stairs, will walk on their toes, and fall frequently, which increases their risk for fractures. Muscle weakness is more noticeable in the lower limbs and will eventually progress to a point where a wheelchair is required for mobility. Abnormal vertebral curvatures such as scoliosis or lordosis can also develop, with scoliosis potentially impairing the client’s lung function. Other signs and symptoms include the following:
- Decreased growth and short stature
- Contractures
- Calf enlargement with thigh muscle wasting
- Enlargement of the tongue and forearm muscles
- Weakness of muscles associated with swallowing, leading to aspiration
- Bladder and bowel incontinence
- Intellectual impairment
- Cardiomyopathy and arrhythmias
- Decreased or absent reflexes
Clients with DMD demonstrate elevated levels of creatinine kinase prior to the development of signs and symptoms. Other enzymes related to muscles may also be elevated. Muscle biopsies will show muscle cell death and replacement of muscle with connective and adipose tissues. In clients with suspected DMD, a gene analysis may be performed with results indicating dystrophin levels less than 5% of normal. An electrocardiogram and echocardiogram may be completed to detect the presence of cardiomyopathy or arrhythmias.
There is no cure for DMD. Gene therapy medication is available, but its efficacy is questionable, and its cost is high. Treatment consists of glucocorticoid administration and preventing complications. Glucocorticoids slow the degeneration of muscle tissue and the development of complications but are not curative. However, long-term use of glucocorticoids places the client at risk for osteoporosis, so calcium and vitamin D supplementation are also necessary. To prevent heart failure and slow the progression of cardiomyopathy, ACE inhibitors and beta-blockers are prescribed. Therapy and exercise can also be used to prevent contractures and muscle atrophy. Surgery may be needed for severe contractures and/or scoliosis.
Epistaxis
The content in this subsection is adapted from StatPearls.[26]
Epistaxis, commonly known as a nosebleed, is a common condition in children, particularly between the age ranges of two to ten years old. Epistaxis results when a blood vessel in the nose ruptures. Rupture can occur for a variety of reasons. It can occur spontaneously or be caused by trauma, allergies, dry air, medications such as NSAIDS, or due to other medical conditions. Epistaxis can be subdivided into anterior and posterior bleeds, with anterior being the most common, as the tissue in this area is very fragile.
When assessing a client with a nosebleed, it is important to inquire about the frequency of their nosebleeds, determine which nare is bleeding, and ask if any particular event caused the nosebleed. The nurse should also assess for hemoptysis (i.e., coughing up blood). This results from posterior epistaxis in which blood pours into the throat and puts the client at risk for airway compromise or aspiration of blood into the lungs.
Anterior epistaxis can usually be identified visually, but a nasal endoscope may be necessary to identify a posterior bleed. Lab work may include a complete blood count to assess for anemia or coagulation studies to look for bleeding tendencies. If the bleeding is severe, a type and screen may be performed in anticipation of a blood transfusion.
Epistaxis treatment depends on the cause, source, and severity of the bleed. Anterior nosebleeds can be treated with direct pressure to the area by pinching the nose or applying a nasal clip. See Figure 16.37[27] for an image of a nasal clip. If pressure does not successfully stop the bleed, vasoconstricting topical medications may be prescribed. Bleeding vessels can also be cauterized with silver nitrate, or the affected nare can be packed with dressings or a nasal tampon or balloon. For posterior nosebleeds, posterior nasal packing can be performed, but it requires an experienced provider, as intubation may also be required. Hospital admission is required with posterior nasal packing due to the risk of cardiac arrhythmias. If packing is not successful for a posterior bleed, the client may require embolization or a surgical procedure to stop the bleed.

When packing is placed for a nosebleed, it needs to stay in place for three to five days. The client is prescribed an antibiotic to prevent toxic shock syndrome. Nasal saline is also prescribed to keep the packing moist. Packing should be removed by an ear, nose, and throat provider or the client’s primary provider.
To prevent future nosebleeds, nurses teach clients and parents/caregivers to keep the nasal mucosa moist with topical saline and avoid nose blowing or picking, hot foods, and strenuous activity.
Erythema Infectiosum
The content of this subsection is adapted from StatPearls.[28]
Erythema infectiosum, also known as fifth disease, is a common viral illness that is caused by parvovirus B19. It mostly affects children ages 5 to 15 years old in the spring and summer seasons. Adults, as well as pregnant clients, can also contract fifth disease. Pregnant clients and clients with sickle cell disease often experience complications associated with this disease.
Most clients contract fifth disease through inhalation of respiratory droplets that are infected with parvovirus B19. However, the virus can also be spread through blood transfusions, blood exposure, and from mother to fetus. Once in the body, the virus has an affinity for immature red blood cells and alters their production.
Initial symptoms of fifth disease are fever, malaise, muscle aches, GI upset, and headache. Eventually, a characteristic rash develops that is red and covers the cheeks, giving the appearance that the client has been slapped in the face. See Figure 16.38[29] for an image of an infant with the classic fifth disease rash on their cheeks. Once the rash appears, the client is no longer infectious. A few days later, a maculopapular rash appears on the trunk and extremities but does not affect the palms of hands or soles of the feet. A maculopapular rash is made up of macules and papules. The rash of fifth disease is usually not itchy but may be worsened by sun or heat exposure.

Some clients also experience joint aches and stiffness, but this is more common in adults. Clients who are pregnant, immunocompromised, or have sickle cell anemia or other chronic blood disorders may also exhibit signs of severe anemia due to the effect of parvovirus B19 on red blood cells. Pregnant clients who are less than 20 weeks’ gestation are at risk for fetal demise.
Fifth disease is diagnosed clinically, and diagnostic testing is not routinely performed. However, antibody testing for parvovirus B19 may be used to confirm the infection or determine immune status for pregnant women.
Treatment for fifth disease consists of supportive care. Acetaminophen and NSAIDs can be administered to manage fever, headache, and joint/muscle aches. For clients with severe anemia due to fifth disease, blood transfusions and close monitoring of hemoglobin and hematocrit levels may be required. Pregnant clients require close follow-up to monitor for fetal complications. Nurses teach clients and their parents/caregivers about good hand hygiene and respiratory etiquette to prevent the spread of infection to others.
Failure to Thrive
The content in this subsection is adapted from StatPearls.[30]
Failure to thrive (FTT) refers to the inability to appropriately gain weight or persistent weight loss in pediatric clients. More specifically, clients are diagnosed with this disorder if they are less than the fifth percentile of weight or demonstrate a decline in their weight percentile on a standardized growth chart. FTT puts the client at risk for malnutrition, which can lead to delays in growth and development. FTT can occur in all ages but is most commonly seen in children under two years of age. Risk factors for FTT are being premature, having a low birth weight, or being diagnosed with a chronic illness or developmental delay.
FTT can be caused by an underlying medical disorder, decreased food intake, or a combination of the two. Insufficient caloric intake is the most common cause and can be linked to feeding difficulties, lack of parental awareness regarding proper nutritional intake, lack of resources available to secure food, or caregiver neglect or abuse. Other clients may have medical conditions that lead to malabsorption of nutrients or require increased intake of calories. Regardless of the specific cause of FTT, caloric intake is inadequate for weight gain and growth.
When assessing a client with FTT, poor weight gain and a thin build will be noted. FTT and the resulting malnutrition can also lead to loss of body mass, weakness, electrolyte disturbances, vitamin deficiencies, weakened immune system, and frequent infections.
To ascertain the specific cause of FTT, many aspects of the client’s health history and physical assessment must be evaluated. For instance, the provider must assess the client’s feeding history, as well as stool and urine output. The client should also be assessed for chronic health conditions that are known to be associated with FTT, such as chronic heart, lung, and gastrointestinal issues or food allergies.
To diagnose FTT, the health care provider examines the client’s weight trends over time and compares the weights to the expected weight for their age. The Semi-Objective Failure to Thrive Tool (SOFTT) can also be used to guide diagnosis. Further testing may be needed depending on the client’s initial presentation and whether there is a concern for an underlying medical condition.
Treatment for FTT consists of increasing caloric intake and treating underlying pathologies. The client’s daily energy and caloric requirements are calculated, and nutritional supplements are often prescribed. Formula-fed infants can be fed more calorically dense formula, and pediatric clients eating solid foods should be offered foods high in fat such as heavy whipping cream, peanut butter, and avocado. Nonnutritive or empty calorie foods such as juice should be limited. Clients with severe malnutrition must be monitored for refeeding syndrome when proper caloric intake is resumed.
Nurses teach clients and parents/caregivers about healthy diets and provide information about community resources for experiencing food insecurity. Further treatment options may be necessary depending on the specific cause and severity of the client’s FTT. For example, total parenteral nutrition or enteral feedings may be needed. Regardless of the cause of FTT, the client’s weight gain is closely monitored and referrals to a nutritionist may be warranted.
Folliculitis
The content in this subsection is adapted from StatPearls.[31]
Folliculitis is an infection of the hair follicle, usually due to bacterial infection but can also be caused by a viral or fungal infection. The most common cause of bacterial folliculitis is Staphylococcus aureus, but it can also be caused by Pseudomonas aeruginosa from contaminated pool or hot tub water. It can also be caused by inflammation due to an ingrown hair or by the use of certain medications (lithium or cyclosporine). Clients at risk for developing folliculitis are those who are obese, have diabetes, use antibiotics long-term, or are immunocompromised.
Folliculitis begins when the hair follicle is invaded by a pathogen causing infection. Invasion can occur due to something as simple as the client scratching their skin. Folliculitis is characterized by the formation of pustules or reddened papules on the skin. The appearance of the skin lesions varies based on the causative organism. Potential complications of folliculitis are abscess formation or the development of cellulitis. See Figure 16.39[32] for an image of folliculitis caused by a fungal infection.
Folliculitis is diagnosed clinically. A biopsy of a lesion may be performed to determine the cause of folliculitis or rule out other causes. Cell scrapings from the affected area can also be examined under a microscope to determine if the folliculitis is fungal in origin.
Although some cases of bacterial folliculitis will resolve on their own, severe cases require topical antibiotics. If topical antibiotics are ineffective, oral antibiotics may be prescribed. A referral to a dermatologist is recommended if treatment fails. Fungal and viral cases are treated with antifungal and antiviral medications. Good skin care is also essential, not only to help with healing, but also to prevent folliculitis from recurring. Nurses teach clients to not scratch or shave affected areas and to apply warm compresses to the lesions.
Hand, Foot, and Mouth Disease
The content in this subsection is adapted from StatPearls.[33]
Hand, foot, and mouth disease (HFMD) is a viral illness that commonly affects pediatric clients under seven years of age. Adults can contract this illness as well, but it is much less common. Most cases of HFMD are caused by Coxsackievirus A type 16, but can be caused by other Coxsackievirus subtypes, as well as enterovirus. Cases of HFMD are more common in spring and summer months, and outbreaks tend to occur in daycares, camps, or among family units.
The causative virus of HFMD can be ingested via the gastrointestinal or respiratory tracts, and symptoms appear within three to six days of infection. Depending on the causative virus, symptoms may vary. For instance, when HFMD is caused by enterovirus, symptoms related to central nervous system dysfunction are common. Once ingested, the virus replicates in the intestines and pharynx and then spreads to lymph nodes and organs.
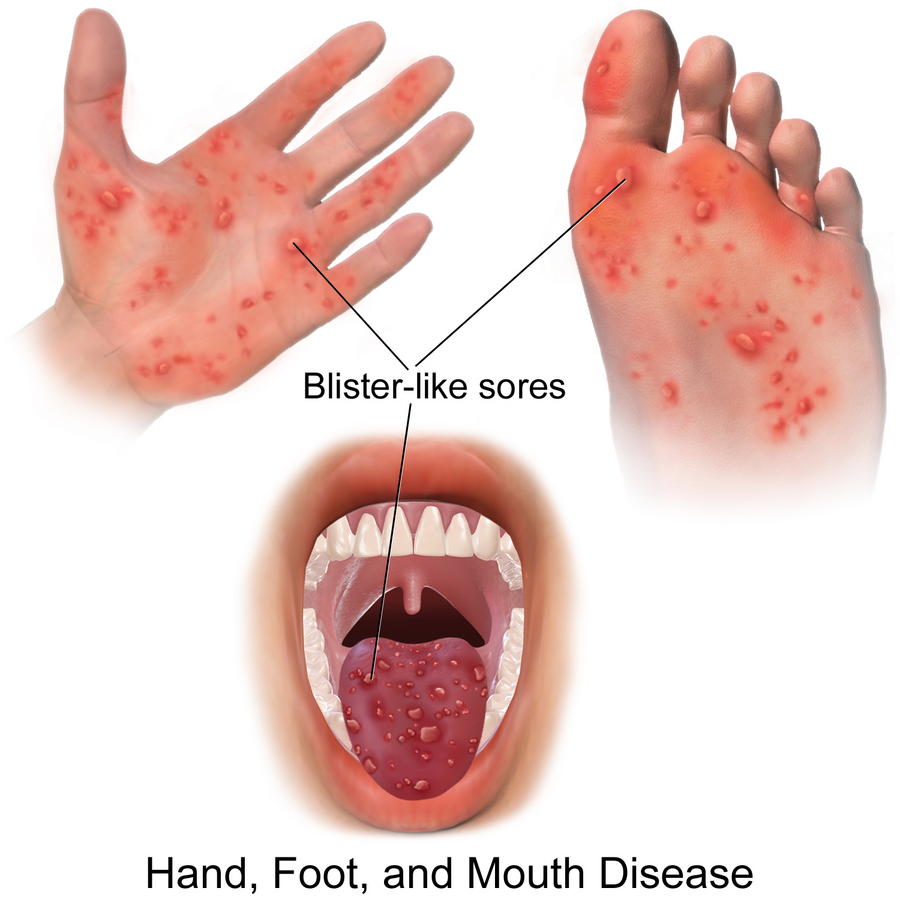
HFMD symptoms start with fever, malaise, and throat or mouth pain due to the presence of an oral rash. The rash may also be present on the hands, feet, buttocks, and extremities. Mouth and throat pain can also lead to dehydration due to poor intake. The rash can vary in appearance, but the lesions eventually rupture and form ulcers. Generally, the lesions do not hurt and are not itchy. See Figure 16.40[34] for an illustration showing the lesions of HFMD.
Although HFMD is diagnosed clinically, the presence of the virus can also be found in stool samples. Examining skin scrapings from lesions under a microscope can also help distinguish HFMD from other viral exanthems. Swabs from lesions may also undergo PCR testing to determine the causative virus.
Treatment of HFMD consists of supportive care. NSAIDs and acetaminophen can be used to manage fever and pain. Liquid forms of ibuprofen and diphenhydramine can be mixed together and used for gargling to help coat ulcers in the mouth. The client should also receive adequate fluid intake and be encouraged to wash their hands to prevent the spread of infection.
Hordeolum
The content in this subsection is adapted from StatPearls.[35]
A hordeolum, commonly known as a stye, is an acute bacterial infection involving the upper or lower eyelid. Most cases are caused by the bacteria Staphylococcus aureus. Clients of any age can be affected by a hordeolum, but there is an increased risk for development in clients with seborrheic dermatitis, diabetes, and increased lipid levels.
A stye occurs when one of the glands of the eyelid becomes infected with S. aureus, leading to inflammation. Infection of the Zeis or Moll glands produces a stye on the eyelash line and is considered an external hordeolum. Infection of the meibomian glands deeper in the eyelid is considered an internal hordeolum. Meibomian glands and Zeis glands are oil-producing glands of the eye, whereas Moll glands are a type of sweat gland.
A hordeolum causes unilateral swelling, redness, pain, and burning of the eyelid. With an external hordeolum, the stye appears as a pustule, and symptoms are more localized. Exudate may be present. See Figure 16.41[36] for an image of an external hordeolum. Internal hordeolum causes diffuse redness and tenderness due to the larger size of the sebaceous glands. A pustule can form with an internal hordeolum, but it cannot be seen unless the eyelid is everted.

Diagnosis is made clinically without diagnostic testing unless cellulitis is suspected.
The treatment is the same for internal or external hordeolum. Warm compresses should be applied four times a day for 15 minutes at a time. Erythromycin ointment may be prescribed for the affected eye. Gentle massage can be performed to encourage expression of exudate. Very large hordeola may require an ophthalmology referral for an incision and drainage.
Hyperopia
The content in this subsection is adapted from StatPearls and Cleveland Clinic.[37],[38]
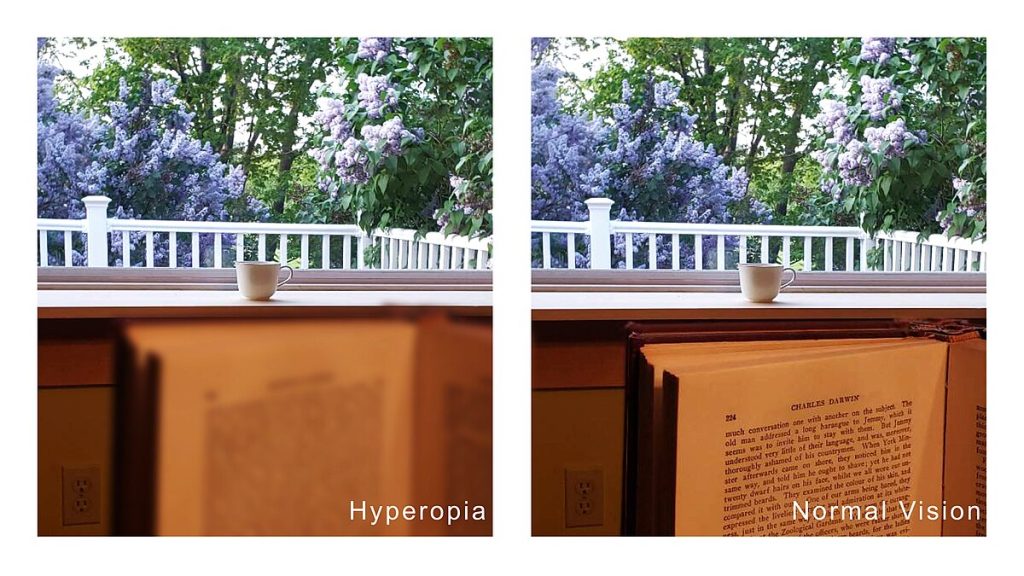
Hyperopia, commonly known as farsightedness, is a disorder of the eye in which nearby objects appear blurry, as shown in Figure 16.42.[39] It is a common condition in children and adults. Risk factors for this condition are older age, diabetes, trauma to the eye, family history, and maternal cigarette smoking during pregnancy.
As with myopia, the pathophysiology of hyperopia also depends on the specific type. The most common type of hyperopia is axial hyperopia, in which the axial length is shorter than normal, which alters the ability of the eye to focus. Signs and symptoms of hyperopia are as follows:
- Blurred vision when looking at close-up objects
- Reading difficulties or squinting in order to read
- Eye rubbing in young children, which may lead to recurrent conjunctivitis or hordeolum
- Inward eye deviation in very young children
- Eyestrain
Potential complications of severe hyperopia in children are amblyopia or strabismus.
Hyperopia is diagnosed with visual acuity tests and more specialized eye examinations completed by an optometrist. Hyperopia is managed nonsurgically with the use of glasses or contact lenses. A variety of surgical options are also available.
Juvenile Idiopathic Arthritis
The content in this subsection is adapted from StatPearls.[40]
Juvenile idiopathic arthritis (JIA) is the most common form of chronic inflammatory arthritis affecting pediatric clients. There are seven distinct subtypes, and they all affect children under the age of 16. The exact cause of JIA is unknown, but it may involve environmental components and an irregular immune response. Potential environmental risk factors include exposure to certain antibiotics, viruses, or bacteria, or being born by cesarean section. Genetic factors may also play a role in the development of this condition. Most types of JIA are more common in female clients than males.
The pathophysiology of JIA is complex and varies among subtypes but involves an imbalance of the cells of the immune system, resulting in inflammation and damage of the joints.
There is a wide variability in the signs and symptoms seen with JIA. Some may have signs and symptoms that resolve without treatment, while others have severe cases leading to joint destruction. Common signs and symptoms of JIA are swelling of soft tissues, pain, inflammation of the synovial membrane, increases in fluid surrounding joints, and bone weakening. Potential complications are unequal limb lengths and contractures of the joints.
There is no specific test that can diagnose a client with JIA. However, a diagnosis of JIA should be considered in pediatric clients who have had arthritis symptoms for over six weeks. Laboratory tests such as inflammatory markers may be elevated in JIA, but these tests are nonspecific. Imaging may be done to help confirm a diagnosis, as well as to determine if joint damage is present, but changes may not be seen in early stages of this disease. Specific subtypes of JIA have guidelines in place to determine which subtype is present.
JIA can be managed with medications that target inflammation and/or the immune system. Most treatment starts with NSAIDs, but more potent medications are available if required. Physical therapy and exercise should also be encouraged to maximize range of motion of the afflicted joints.
Molluscum Contagiosum
The content in this subsection is adapted from StatPearls.[41]
Molluscum contagiosum, commonly known as water warts, is a skin condition caused by the molluscum contagiosum virus. There are four different subtypes, but MCV-1 is the most common subtype and is primarily seen in children in the age range of two to five. The causative virus is spread from direct contact (skin to skin), indirect contact (inanimate objects such as towels, toys, or razors), or from mother to fetus. This disorder can occur anywhere but is more frequent in humid and warm climates. Other risk factors are immunodeficiency, sexual activity, and atopic dermatitis.
Once infected with the virus, symptoms can appear as soon as two weeks or as long as six months. The virus infects the keratin-producing cells of the epidermis and inhibits the body’s normal immune defenses. This leads to the presence of persistent lesions on the skin.
The lesions formed by molluscum contagiosum infection are round, firm, dome-like in shape, and range from white to pink to purple in color. See Figure 16.43[42] for an image of mollusca lesions. In children, these lesions do not appear on the soles of the feet or palms of the hands but rather on the face, trunk, arms, legs, and axilla. Sometimes a cheese-like exudate can be expressed from the center of the lesions. The lesions may also be painful or itchy. When the lesions are scratched or removed, they tend to bleed. Potential complications of this disorder are cellulitis, abscess formation, or inflammation of the conjunctiva with eyelid lesions.

Molluscum contagiosum is diagnosed clinically. Cells from the lesions can be examined under a microscope or dermascope to help confirm a diagnosis.
Although molluscum contagiosum can resolve on its own in six to twelve months, many clients seek treatment. Treatment can consist of physically removing the mollusca, but this can be painful and lead to scarring. Other treatment options consist of topical and oral medications. Topical medications must be applied to every lesion to be effective. Nurses teach clients to cover the infected areas to prevent spread of infection to others.
Myopia
The content in this section is adapted from StatPearls and Mayo Clinic.[43],[44]
Myopia, commonly referred to as nearsightedness, is the inability to see far away objects clearly. It is the most common eye disorder seen in pediatric clients and can affect any gender or race but is most common in Asians. Another risk factor for developing myopia is excessive screen time.
The pathophysiology of myopia depends on the specific type. The most commonly seen type is axial myopia. This is when the axial length, or the length from the cornea to the retina, is increased and alters the ability of the eye to focus.
Although older children can clearly articulate their inability to clearly see things at a distance, signs and symptoms of myopia in young children consist of the following:
- Frequent headaches
- Holding objects closely to the face
- Mistakes when taking notes at school
- Unable to see the television unless sitting within three feet
- Squinting
Myopia can be categorized as mild, moderate, or severe. It is diagnosed by optometrists with visual acuity tests and specialized eye examinations.
Myopia is managed nonsurgically with the use of glasses or contact lenses. Surgical options are also available.
Periorbital Cellulitis
The content in this subsection is adapted from StatPearls.[45]
Periorbital cellulitis is a specific type of cellulitis that occurs around the soft tissue of the eye. Periorbital cellulitis can occur due to trauma that results in infection or as a result of a sinus infection that spreads to the periorbital region. Common causes of bacterial infection are Staphylococcus aureus, Streptococcus pneumoniae, or Streptococcus pyogenes, although there are a variety of other bacterial and fungal causes. This disorder can occur in any age group, but it is most common in pediatric clients.
The pathophysiology of periorbital cellulitis depends on its etiology. In periorbital cellulitis caused by sinusitis, bacteria can easily spread from the sinuses to the periorbital region via the venous system or direct spread through tissues. Direct infection with bacteria can also occur in the case of trauma or an insect bite. Despite the etiology, the resulting infectious response is the same.
Presenting signs and symptoms are redness and swelling around the eye, as well as swelling of the eyelid. See Figure 16.44[46] for an image of an infant with periorbital cellulitis. In cases of orbital cellulitis where the infection has spread to the deeper tissues of the eye, the client will have decreased eye movement or the inability to move the eye; reduced vision; fever; pain; and red, swollen eyelids. Other potential complications of periorbital cellulitis are abscess formation or meningitis.

Periorbital cellulitis is diagnosed clinically. A CT scan may be performed to distinguish between periorbital and orbital cellulitis or to determine the presence of other complications.
Treatment consists of antibiotics, either oral or intravenous, depending on the severity of the condition, and referral to an ophthalmologist. Clients who are over one year old and have mild symptoms can be treated at home with oral antibiotics. Clients with severe cases, those who are younger than one year of age, or those who do not improve with oral antibiotics will require hospitalization. Severe cases or those with abscess formation will require surgical management for drainage.
Pinworm
The content in this section is adapted from StatPearls.[47]
Pinworm is a parasitic worm infestation by Enterobius vermicularis. It is colloquially referred to as pinworm due to the tail of the worms having a pin-like shape. See Figure 16.45[48] for an image of the tail of a pinworm. Risk factors for contracting pinworm are living in crowded quarters, hot climates, contact with other infected individuals, poor hygiene, and eating after coming into contact with infected objects without performing hand hygiene.
![]”Evermicularis_SC_posterior” by Division of Parasitic Diseases and Malaria (DPDM) of the Centers for Disease Control and Prevention is in the Public Domain. Photo showing a closeup of the pointed tail of a pinworm](https://wtcs.pressbooks.pub/app/uploads/sites/48/2024/10/Evermicularis_SC_posterior.jpg)
Pinworm infestation occurs by direct contact with infected individuals or objects, such as bedding, clothing, or furniture, and the subsequent ingestion or inhalation of pinworm eggs. The eggs travel to the small intestine and develop into adult worms. At night, the female adult worms move to the anal area to lay eggs, which causes intense perianal itching. Itching the anal area can then cause contamination of the hands with eggs, spreading eggs to anything that is touched.
The most commonly seen symptom of pinworms is itching of the perineal area, along with perianal redness. Because the itching most commonly occurs at night, sleep disturbances can also occur. Other symptoms that have been reported are diarrhea, urinary tract infections in females, visible worms in the perineal area, and abdominal pain. Potential complications are secondary bacterial infections due to scratching and appendicitis due to pinworms blocking the appendix lumen.
Pinworm infection is diagnosed by applying tape or another adhesive material to the perianal region and then examining the tape under the microscope for the presence of eggs or adult worms. Pinworms are not typically expelled in the stool, so fecal testing is not beneficial.
Treatment of pinworms consists of anti-parasitic medications. It is recommended to treat everyone in the household to prevent recurrence, even if they have no symptoms. Nurses teach clients and their parents/caregivers about the importance of good hygiene and regular handwashing to prevent the spread of infection. Infested objects such as blankets, clothing, and towels should be washed in hot, soapy water.
Poisoning
This content is adapted from Cleveland Clinic and Harvard Health Publishing.[49],[50]
Poisoning occurs when a client is exposed to a harmful agent. Children are more susceptible to poisoning when compared to adults. Examples of potentially poisonous agents are as follows:
- Carbon monoxide
- Lead or other heavy metals
- Plants such as poison hemlock
- Venom from animals
- Contaminated food
- Medications that are taken incorrectly
- Alcohol
- Nicotine
- Household cleaning products
- Pesticides
Signs and symptoms of poisoning depend on the type and amount of the toxic substance, the route of exposure, and how soon the client receives treatment. Poisoning may affect the entire body or only the area that was exposed to the toxin. Symptoms may start immediately after the exposure or be delayed. Potential symptoms include the following:
- Changes in temperature or heart rate
- Nausea, vomiting, diarrhea, or stomach pain
- Headache
- Eye irritation or vision changes
- Coughing or coughing up blood
- Chest pain
- Burning in the eyes, nose, or throat
- Fainting or dizziness
- Difficulty breathing
- Skin rash, burning, redness or pain
If poisoning is suspected, the client or their parent/caregiver should call 911 or poison control for emergency first aid. For example, if someone gets a poisonous substance in their eyes, the eyes should immediately be rinsed under lukewarm water for 15 to 20 minutes. Skin that comes into contact with a poison should also be rinsed with lukewarm water for 15 minutes, and any clothing with poison on it should be removed. For inhaled poisons, the affected client should be brought outside for fresh air. When a poisonous substance is taken by mouth, whatever has not been swallowed should be spit out, but vomiting should not be induced. In severe cases, hospitalization may be required. In the hospital, the client may receive intravenous fluids, antidote medications, chelation therapy, or other supportive care. In some cases, the client may be given activated charcoal and/or have a nasogastric tube inserted with suction applied to prevent further absorption of poisonous substances.
Most types of poisonings can be prevented. Some tips for preventing poisonings are the following:
- Ensure the home has a carbon monoxide detector.
- Keep cleaning solutions in their original packages and away from children. Cleaning solutions should never be mixed.
- Keep medications away from children.
- Take medications as prescribed by your provider.
- Consult the health care provider about the use of over-the-counter drugs, especially in children.
- Avoid contact with unfamiliar plants and animals.
- Ensure proper food safety.
Poliomyelitis
This subsection is adapted from StatPearls.[51]
Poliomyelitis, commonly known as polio, is an infectious disorder caused by poliovirus that can cause paralysis. With the advent of vaccination, polio has mostly been eliminated, but it is still seen in underdeveloped countries with unsanitary conditions and poor access to health care. Clients who are immunocompromised and receive a live formulation of the polio vaccine are also at risk for contracting a form of polio.
Poliovirus spreads mostly through the fecal-oral route, but there have also been cases of oral-oral spread of the virus. Once infected with the virus, it begins to replicate in lymphatic tissues of the mouth, throat, and gastrointestinal tract. From here, the virus can spread to the central nervous system and cause paralysis.
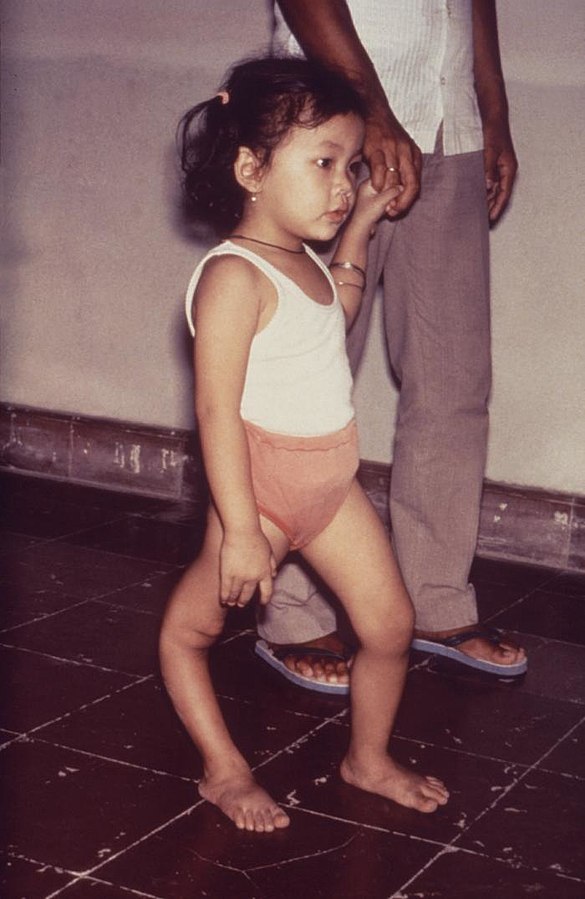
Although poliomyelitis can cause paralysis, the majority of cases are nonparalytic and present with flu-like symptoms. Only about 5% of clients with poliomyelitis actually have true motor paralysis. Flu-like symptoms that may appear with polio are headache, muscle aches, malaise, nausea, sore throat, and stiffness of the neck. When the poliovirus spreads to the spinal cord, clients will develop muscle spasm and paralysis. Often this paralysis affects one side of the body and predominately the lower limbs. Although clients can recover from paralysis due to poliomyelitis, a large portion of clients are left with residual disabilities. See Figure 16.46[52] for an image of a child with a leg deformity as a result of polio.
A potential complication of poliovirus is paralysis of the respiratory muscles, leading to respiratory failure. Post-polio syndrome can also occur years after the initial infection. This syndrome consists of muscle weakness (which can be progressive), muscle pain, difficulty breathing, difficulty swallowing, and fatigue.
Poliovirus can be detected by PCR testing.
Treatment for polio consists of supportive care that manages initial symptoms. Fever and pain can be treated with acetaminophen or ibuprofen. Splints and/or orthotics are used to support paralyzed extremities and prevent contractures of the joints or other deformities. Any joint contractures that do develop can be managed surgically to provide maximum mobility for the client. Exercise is also recommended to strengthen weakened muscles.
Poliomyelitis is preventable with the administration of the inactivated polio vaccine (IPV).
For more information on the IPV vaccine, visit the Centers for Disease Control and Prevention web page.
Reye’s Syndrome
The content in this subsection is adapted from StatPearls.[53]
Reye’s syndrome is a very rare but serious pediatric illness that is associated with the use of aspirin or aspirin-containing products by those experiencing viral illness. Viral conditions that have been linked to Reye’s syndrome are influenza A or B, as well as varicella. Risk factors for developing Reye’s syndrome are pediatric clients ages of 5 to 15 years old or those with congenital metabolism defects. Less than two cases per year have been reported since 1994, but this number may be inaccurate due to the lack of mandated reporting.
The pathophysiology of Reye’s syndrome is not well-understood, but it is thought to involve cellular damage that is triggered by aspirin use in conjunction with the presence of a viral illness. Ultimately, this leads to edema in the brain and increased intracranial pressure.
The initial symptom of Reye’s syndrome is continual vomiting followed by lethargy and delirium. The client may also exhibit inappropriate reflexes, as well as increased respiratory rate and heart rates. Eventually, the condition can progress to seizures, paralysis, coma, respiratory arrest, and/or death.
There is no specific test to diagnose Reye’s syndrome, so it is made clinically. Clients often have associated lab abnormalities, including increased ammonia levels that correlate with changes in their mental status, as well as elevated liver enzymes, amylase, and lipase levels. Blood coagulation studies may be abnormal, and bicarbonate levels may be decreased. Due to the presence of neurological signs and symptoms, a lumbar puncture may be performed and the cerebral spinal fluid analyzed. During Reye’s syndrome, the leukocyte count of the cerebral spinal fluid is less than eight.
Treatment for Reye’s syndrome consists of supportive care and close monitoring in the intensive care unit due to the severity of the disorder. The client may require central line placement, as well as intubation and mechanical ventilation. Additional treatments may also be warranted based on the client situation. For example, high ammonia levels may be treated with sodium polystyrene sulfate or hemodialysis performed for severely elevated levels. If the client has signs of increased intracranial pressure, the head of the bed should be elevated at 30 degrees, diuretics are administered, and the client may require sedation.
Due to the high mortality rate of Reye’s syndrome, prevention is key. Parents and caregivers should be educated on avoiding giving aspirin or aspirin-containing products to children, as well as the signs and symptoms of Reye’s syndrome.
Staphylococcal Scalded Skin Syndrome
The content in this subsection is adapted from StatPearls.[54]
Staphylococcal scalded skin syndrome (SSSS) is an infection caused by strains of Staphylococcus bacteria that produce toxins. SSSS most commonly appears after an infection of the upper respiratory tract, conjunctiva, umbilical stump, or ears. Some individuals are nasal carriers of this bacterial strain and can spread it to others. Most cases of SSSS occur in pediatric clients under two years of age, but it can occur in adults as well. Outbreaks of this disorder are usually linked to daycares or nurseries.
When infected with a toxin-producing strain of Staphylococcus, toxins target the epidermis of the skin, causing exfoliation (peeling). This skin loss can be localized, or toxins can spread via the circulation and affect the entire body. The loss of skin leads to reduced body temperature, fluid volume loss, and the potential for secondary infection.
Initial symptoms of SSSS are elevated temperature, malaise, and irritability, followed by the development of a red, painful rash. Fluid-containing blisters form, and the skin will start to peel off. The blisters usually start locally and spread diffusely, but mucous membranes remain unaffected. Hypotension and symptoms of shock may also be present. Although most children heal well, there is the potential for scarring. Other potential complications of SSSS are sepsis and renal failure. See Figure 16.47[55] for an image of skin peeling caused by SSSS.

Laboratory testing includes a complete blood count to assess for signs of sepsis and electrolyte monitoring if dehydration is present. Cultures of blood and fluid from the blisters can be taken but are often negative. Biopsy of the lesions can help confirm the diagnosis and rule out other conditions with similar presentations. Chest X-rays may be taken to determine if the lungs are the initial source of infection. A dermatologist should also be consulted if the diagnosis is unclear.
Treatment consists of oral or intravenous antibiotics depending on the severity of the disease. Intravenous fluids are prescribed for clients with sepsis or dehydration. Dressings are applied to the afflicted areas to encourage healing and reduce heat loss. Admission to a burn unit may be required for severe cases. Supportive care is used to manage temperature and nutritional status. Nurses ensure contact transmission-based precautions and strict hand hygiene to prevent the spread of the infection to others.
Strabismus
The content in this subsection is adapted from StatPearls and Cleveland Clinic.[56],[57]
Strabismus, commonly known as crossed eyes, is a disorder in which the eyes are not properly aligned, leading to them looking in different directions. Infantile strabismus is diagnosed before six months of age but diagnoses after this are considered to be acquired strabismus. Strabismus is caused by neuromuscular abnormalities or the eye muscle itself. Risk factors for the development of strabismus are a family history, untreated refractive errors, stroke, head trauma, brain tumors, Down syndrome, or cerebral palsy.
Eye movement involves coordination between the muscles of the eye, cranial nerves, and the brain. When there is an issue with one of these components, strabismus can result. However, the exact pathophysiology of strabismus is not well-understood.
There are a variety of types of strabismus, so signs and symptoms can vary. The eye may point inward, outward, up, or down as seen in Figure 16.48.[58] It may happen constantly or intermittently. It may always affect the same eye, or it can alternate between eyes. Other signs and symptoms are double vision, headaches, eye strain, reading difficulties, closing one eye to look at objects, and head tilting. Symptoms often appear by the age of three years. If strabismus is not treated appropriately, amblyopia can occur.

Strabismus is diagnosed by eye examination by a health care provider when assessing the ability of the eyes to focus and move. Visual acuity testing may also be performed.
Treatment of strabismus depends on the underlying cause. Treatment modalities may consist of corrective lenses, eye exercises, or surgery on the eye muscles. If eye muscles are overactive, eye medications may be given to weaken the eye muscle. Eye patches may be recommended if amblyopia is present.
Sunburn
The content in this subsection is adapted from StatPearls.[59]
Sunburn is an acute inflammatory response of the skin to ultraviolet ray exposure. This exposure can be from the sun or from tanning beds. Sunburn severity can vary widely depending on certain risk factors. Multiple medications, such as certain antibiotics or NSAIDs, can increase the risk of sunburn. The risk for sunburn also increases with a clear sky, higher altitudes, equator proximity, exposure to sunlight during the 10 a.m.-4 p.m. time frame, and lack of preventative measures. Clients with paler skin are also more prone to sunburn due to reduced melanin.
When the skin is exposed to ultraviolet rays, cell DNA is damaged. In an attempt to repair the damaged DNA, inflammatory markers are released, and pain receptors are activated. This leads to the classic sunburn symptoms of painful and reddened skin. In addition to red and painful skin, the sunburned area may also feel warm to the touch. In severe episodes of sunburn, blisters can form, and the client can experience nausea, chills, and an elevated temperature. See Figure 16.49[60] for an image of blistering due to sunburn. As the sunburn heals, the skin may peel. Those with very light skin may eventually develop sunspots in these areas.

Sunburn is diagnosed clinically and can usually be managed at home. Pain can be reduced with the use of NSAIDs, and hydration should be encouraged. Cold compresses, aloe vera, or lotion can be applied to the skin to help with pain and to increase moisture. Blisters should be washed with soap and water and covered with gauze if open. Clients with severe sunburn may require admission to a burn unit, intravenous fluids, electrolytes, and analgesics.
Due to the increased risk of skin cancer with each occurrence of sunburn, prevention is key. Nurses teach clients that sunburn can be prevented by avoiding sun exposure, especially during the hours of 10 a.m. and 4 p.m. Tanning beds should also be avoided. Other preventative measures include the use of protective clothing, staying in the shade, and using sunscreen. Sunscreen should be water resistant and at least SPF 30. Sunscreen should be applied 15 to 30 minutes prior to sun exposure and reapplied every two hours to remain effective. Infants younger than six months of age should not be exposed to direct sunlight if possible. Clients who have had multiple severe sunburns or a history of skin cancer should see a dermatologist yearly for a skin examination.
Tetanus
The content in this subsection is adapted from StatPearls and the CDC.[61]
Tetanus is an infection caused by the bacterium Clostridium tetani, which can be found in soil, dust, or the feces of animals. This bacterium is more commonly found in areas with hot and wet climates. People at risk for contracting tetanus are those who are unvaccinated, immunosuppressed, do not receive booster vaccines, or use intravenous drugs. Infants at risk for neonatal tetanus include those who are born to an unvaccinated mother, are delivered at home deliveries, have their umbilical cord cut with a nonsterile technique, or have an infectious substance contact their umbilical stump. Tetanus can occur at any age but is most commonly seen in infants and young clients. Due to the advent of vaccination, the prevalence of tetanus infection has decreased worldwide.
Tetanus infection can occur in a variety of ways, but spores from C. tetani commonly enter the body through an open wound. Once in the wound, the bacteria multiply and release toxins that damage surrounding tissue and also affect muscles and nerves. These toxins do not remain local and eventually spread to the central nervous system.
Due to the effect of the toxin on muscles and nerves, common clinical manifestations are muscle spasms and lockjaw (spasms affecting the neck and jaw that make it hard to swallow or open the mouth). Spasms usually start in the face and progress to the rest of the body and can be strong enough to tear muscles or fracture bones. Other associated symptoms are pain, drooling, fecal and urinary incontinence, and spasms leading to respiratory dysfunction. Once the disorder progresses to the central nervous system, the client can experience altered blood pressure and heart rate, sweating, and fever.
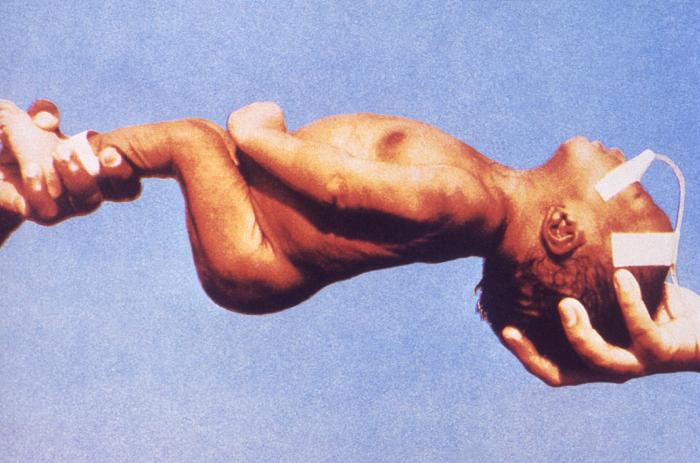
When infants suffer from neonatal tetanus, they are irritable, rigid, and feed poorly. See Figure 16.50[62] for an image of an infant who is rigid from tetanus. Severe muscle contractions can also be triggered if the infant is touched. Long-term developmental issues can also result.
Potential complications of tetanus are aspiration pneumonia, laryngospasm, secondary bacterial infections of the original wound, respiratory failure, cardiac arrest, and death.
Tetanus is diagnosed clinically and cannot be confirmed with laboratory testing. There is a chance that C. tetani can be cultured from a wound where it gained entry to the body, but this rarely occurs. Diagnosis can also be aided by the use of the spatula test. With this test, the provider touches the posterior wall of the pharynx with a soft instrument. The test is considered positive if the client’s jaw contracts involuntarily instead of exhibiting the gag reflex.
Tetanus is treated by administration of human tetanus immunoglobulin (HTIG) to help rid the body of toxins and reduce the severity and length of the disease. The initial wound should be debrided and antibiotics administered. Antispasmodics, such as baclofen, can also be used to manage muscle rigidity. Benzodiazepines can be used to decrease anxiety and relax the client’s muscles to prevent respiratory issues. Magnesium can be prescribed to prevent muscle spasms and manage temperature and blood pressure alterations caused by toxin spread to the central nervous system. Clients with severe cases may require admission to the intensive care unit for intubation or tracheostomy and mechanical ventilation.
Ultimately, tetanus is preventable with the administration of a vaccine. Usually, this is given in combination with vaccines for diphtheria and pertussis as part of routine series of vaccines (DTap or Tdap). However, prophylactic doses can also be given if the client has been potentially exposed to C. tetani.
Read more information about the DTap or Tdap vaccines on the Centers for Disease Control and Prevention web page.
Viral Exanthem Rash
The content in this subsection is adapted from Cleveland Clinic.[63]
A viral exanthem rash is an extensive rash that is accompanied by a viral infection. These rashes occur due to an immune response to the viral infection, skin damage from the virus, or reaction to toxins produced by the virus. Exanthem rashes may occur with these viral infections:
- Varicella
- Coronavirus
- Fifth disease
- Hand, foot, and mouth disease
- Measles
- Rubella
- Roseola
- Mononucleosis
A viral exanthem rash may be itchy and is associated with viral symptoms such as fever, malaise, body aches, headache, or upper respiratory symptoms. Excessive scratching of rashes may cause scarring and/or secondary bacterial infections.
Treatment for viral exanthems depends on the causative virus but mainly consists of supportive care. Acetaminophen or NSAIDs may be recommended for fever or body aches, and calamine lotion or hydrocortisone cream may help with itching. Cold compresses can also be applied to the affected area for 15-30 minutes a few times a day. Proper vaccination is also essential to prevent many illnesses that can lead to a viral exanthem rash.
- Sutaria, A. H., Masood, S., Saleh, H. M., et al. (2023) Acne vulgaris. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK459173/ ↵
- “Akne-jugend” by Ellywa is in the Public Domain. ↵
- Blair, K., Cibis, G., Zeppieri, M., et al. (2024). Amblyopia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK430890/ ↵
- Cleveland Clinic. (2023). Lazy eye (Amblyopia). https://my.clevelandclinic.org/health/diseases/10707-amblyopia-lazy-eye ↵
- Eberhardt, M., & Rammohan, G. (2023). Blepharitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK459305/ ↵
- “Anterior_Blepharitis” by Imrankabirhossain is licensed under CC BY-SA 4.0 ↵
- Brown, B. D., & Hood Watson, K. L. (2023). Cellulitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK549770/ ↵
- “44699141152_eff8dff408_k” by John Campbell is in the Public Domain. ↵
- Centers for Disease Control and Prevention. (2023). What is cerebral palsy? https://www.cdc.gov/ncbddd/cp/facts.html ↵
- Cleveland Clinic. (2024). Chalazion. https://my.clevelandclinic.org/health/diseases/17657-chalazion ↵
- Jordan, G. A., & Beier, K. (2023). Chalazion. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK499889/ ↵
- “8423448539_ab349b599e_o” by Community Eye Health is licensed under CC BY-NC 2.0 ↵
- Lee, K., Cascella, M., & Marwaha, R. (2023). Intellectual disability. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK547654/ ↵
- Turbert, D. (2022). What is color blindness? American Academy of Ophthalmology. https://www.aao.org/eye-health/diseases/what-is-color-blindness ↵
- “Ishihara_9” a derivative work by Pbrks is in the Public Domain. ↵
- Siddiqui, A. H., & Koiala, J. (2023). Methicillin-resistant staphylococcus aureus. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK482221/ ↵
- Cedars Sinai. (n.d.). Community-acquired MRSA. https://www.cedars-sinai.org/health-library/diseases-and-conditions/c/community-acquired-mrsa.html ↵
- “Cutaneous_abscess_MRSA_staphylococcus_aureus_7826_lores” by CDC/ Bruno Coignard, M.D.; Jeff Hageman, M.H.S. is in the Public Domain. ↵
- Mayo Clinic. (2024). Congenital heart defects in children. https://www.mayoclinic.org/diseases-conditions/congenital-heart-defects-children/symptoms-causes/syc-20350074 ↵
- Diaz-Frias, J., Horenstein, M. S., & Guillaume, M. (2024). Tetralogy of Fallot. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK513288/ ↵
- Gillam-Krakauer, M., & Mahajan, K. (2023). Patent ductus arteriosus. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK430758/ ↵
- Salvador, K., & Wagner, M. (2024) Tetrology of Fallot: Nursing diagnoses and care plans. NurseTogether. https://www.nursetogether.com/tetralogy-of-fallot-nursing-diagnosis-care-plan/ ↵
- “Tetralogy_of_Fallot” by Mariana Ruiz LadyofHats is in the Public Domain. ↵
- Venugopal, V., & Pavlakis, S. (2023). Duchenne muscular dystrophy. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK482346/ ↵
- Venugopal, V., & Pavlakis, S. (2023). Duchenne muscular dystrophy. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK482346/ ↵
- Tabassom, A., & Dahlstrom, J. J. (2022). Epistaxis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK435997/ ↵
- “NasalPressureL.jpg” by Doc James is licensed under CC BY-SA 4.0 ↵
- Kostolansky, S., & Waymack, J. R. (2023). Erythema infectiosum. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK513309/ ↵
- “Slapped_cheek_Erythema_Infectiosum” by Gzzz is licensed under CC BY-SA 4.0. ↵
- Smith, A. E., Shah, M., & Badireddy, M. (2023). Failure to thrive. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK459287/ ↵
- Winters, R. D., & Mitchell, M. (2023). Folliculitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK547754/ ↵
- “Pityrosporum_folliculitis_2” by Ran Yuping et al. is licensed under CC BY-SA 3.0 ↵
- Guerra, A. M., Orille, E., & Waseem, M. (2024). Hand, foot, and mouth disease. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK431082/ ↵
- “Hand_Foot_%26_Mouth_Disease” by BruceBlaus is licensed under CC BY-SA 4.0 ↵
- Willmann, D., Guier, C., & Patel, B. C. (2023). Hordeolum (Stye). StatPearls. https://www.statpearls.com/point-of-care/29591 ↵
- “Stye02” by Andre Riemann is in the Public Domain. ↵
- Cleveland Clinic. (2023). Hyperopia (Farsightedness). https://my.clevelandclinic.org/health/diseases/hyperopia-farsightedness ↵
- Majumdar, S., & Tripathy, K. (2023). Hyperopia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK560716 ↵
- “Hyperopia_comparison” by David Jueng is licensed under CC BY-SA 4.0 ↵
- Thatayatikom, A., Modica, R., & De Leucio, A. (2024) Juvenile idiopathic arthritis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK554605/ ↵
- Badri, T., & Gandhi, G. R. (2023). Molluscum contagiosum. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK441898/ ↵
- “Molluscaklein” by Evan Herk is licensed under CC BY-SA 3.0 ↵
- Subudhi, P., & Agarwal, P. (2023). Myopia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK580529/ ↵
- Mayo Clinic. (2024). Nearsightedness. https://www.mayoclinic.org/diseases-conditions/nearsightedness/diagnosis-treatment/drc-20375561 ↵
- Bae, C., & Bourget, D. (2023). Periorbital cellulitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK470408/ ↵
- “53453738969_072c84ecca_k” by Community Eye Health is licensed under CC BY-NC-SA 2.0 ↵
- Rawla, P., & Sharma, S. (2024). Enterobius vermicularis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK536974/ ↵
- “Evermicularis_SC_posterior” by Division of Parasitic Diseases and Malaria (DPDM) of the Centers for Disease Control and Prevention is in the Public Domain. ↵
- Cleveland Clinic. (2024). Poisoning. https://my.clevelandclinic.org/health/diseases/poison ↵
- McCarthy, C. (2019). How to prevent poisonings in children. Harvard Health Publishing. https://www.health.harvard.edu/blog/how-to-prevent-poisonings-in-children-and-what-to-do-if-they-happen-2019031916230 ↵
- Wolbert, J. G., Rajnik, M., & Higginbotham, K. (2024). Poliomyelitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK558944/ ↵
- “Polio_sequelle” by Centers for Disease Control and Prevention is in the Public Domain. ↵
- Chapman, J., & Arnold, J. K. (2023). Reye syndrome. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK526101/ ↵
- Ross, A., & Shoff, H. W. (2024). Staphylococcal scalded skin syndrome. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK448135/ ↵
- “OSC_Microbio_21_02_SSSS” by CNX OpenStax is licensed under CC BY 4.0 ↵
- Kanukollu, V. M., & Sood, G. (2023). Strabismus. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK560782/ ↵
- Cleveland Clinic. (2023). Strabismus (Eye misalignment). https://my.clevelandclinic.org/health/diseases/strabismus-eye-misalignment ↵
- “Depiction_of_a_person_suffering_from_Strabismus_or_crossed-eyes” by https://www.myupchar.com/en is licensed under CC BY-SA 4.0 ↵
- Guerra, K. C., & Crane, J. S. (2023). Sunburn. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK534837/ ↵
- “Sunburn_blisters” by Axelv is licensed under CC BY-SA 3.0 ↵
- Bae, C., & Bourget, D. (2023). Tetanus. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK459217/ ↵
- “Neonatal_tetanus_6374” by unknown author at Centers for Disease Control and Prevention is in the Public Domain. ↵
- Cleveland Clinic. (2022). Viral exanthem rash. https://my.clevelandclinic.org/health/diseases/22510-viral-exanthem-rash ↵
Commonly known as acne; a common chronic skin condition in adolescents that can affect clients of any age. Acne is a result of androgens and the presence of the bacteria Cutibacterium acnes.
Skin lesions that are associated with acne; open comedones are known as blackheads, and closed comedones are known as whiteheads.
A lazy or wandering eye.
Inflammation of the eyelid.
A bacterial infection of the skin, including the dermis and subcutaneous layer.
A group of disorders that affects the ability to move and maintain balance and posture.
A noninfectious, inflammatory lesion of either the meibomian or Zeis glands of the eye.
Deficits in intellectual functioning and adaptive behavior.
When colors are seen abnormally, also known as color deficiency.
An infection caused by methicillin-resistant Staphylococcus aureus that is acquired during hospitalization.
An infection caused by methicillin-resistant Staphylococcus aureus that develops in a non-hospitalized client.
A structural defect of the heart that is present at birth.
A congenital heart defect in which there is a hole between the two atria of the heart.
A congenital heart defect in which there is a hole between the two ventricles of the heart.
A congenital heart defect in which the ductus arteriosus fails to close at birth.
A combination of four different congenital heart defects in which there is a ventral septal defect, hypertrophy of the right ventricle, narrowing of the pulmonic valve, and a displaced aorta.
Occur in those with Tetralogy of Fallot and consist of worsening cyanosis, increasing respiratory rate, increase in respiratory depth, syncope, and even cardiac arrest.
A virus in the herpes family of viruses; has a wide range of symptoms leading from asymptomatic to death.
A severe form of muscular dystrophy that leads to progressive muscle breakdown and weakness.
A nosebleed.
Also known as fifth disease; a common viral illness caused by parvovirus B19.
A rash that is made up of macules and papules.
The inability to gain weight appropriately or persistent weight loss.
An infection of the hair follicle, usually due to bacterial infection.
A viral illness that commonly affects pediatric clients under seven years of age.
A bacterial infection involving the upper or lower eyelid; also known as a stye.
Oil-producing glands deep within the eyelids.
Oil-producing glands of the eye.
A type of sweat gland within the eye.
A disorder of the eye in which up close objects are blurry; also known as farsightedness.
The most common form of chronic inflammatory arthritis affecting pediatric clients; its cause is unknown.
A skin condition caused by the molluscum contagiosum virus; also known as water warts.
The inability to see far away objects clearly; also referred to as nearsightedness.
A specific type of cellulitis that occurs around the soft tissue of the eye.
A parasitic worm infestation by Enterobius vermicularis.
Exposure to a harmful agent.
An infectious disorder caused by poliovirus that can lead to paralysis; commonly referred to as polio.
A very rare but serious pediatric illness that is associated with the use of aspirin or aspirin-containing products by those experiencing viral illness.
An infection caused by strains of Staphylococcus bacteria that produce toxins.
Peeling of the skin.
A disorder in which the eyes are not properly aligned, leading to them looking in different directions; more commonly known as crossed eyes.
An acute inflammatory response of the skin to ultraviolet ray exposure.
An infection caused by the bacterium Clostridium tetani, which can be found in soil, dust or the feces of animals.
Spasms affecting the neck and jaw that make it hard to swallow or open the mouth.
An extensive rash that is accompanied by a viral infection.

