16.11 Impetigo
Impetigo is a contagious bacterial infection in the superficial layers of the skin. There are two different types of impetigo called nonbullous and bullous. Nonbullous impetigo starts as a vesicle or a pustule that coalesces and ruptures, causing a characteristic honey-colored crust with an erythematous base. There are often multiple lesions on the face, and extremities and fever may be present. Bullous impetigo begins with small vesicles that become bullae. Bullae contain a clear or yellow fluid that eventually progresses to become purulent or dark. They do not have a honey-colored crust or erythema and tend to occur on the trunk and between the fingers.[1]
Impetigo as a whole is more likely to be seen in the two- to five-year-old age range, but it can occur in any age group. Bullous impetigo is more common in infants and toddlers under two years of age. Risk factors include living in climates that are hot and humid; living in close confinement with others; daycare attendance; poor hygiene; poor nutrition; immunosuppression; and the presence of skin breakdown due to insect bites, trauma, or scratching.[2]
Potential complications of impetigo include scarring, meningitis in newborns, acute post-streptococcal glomerulonephritis, sepsis, and staphylococcal scalded skin syndrome.[3] Staphylococcal scalded skin syndrome is discussed in a subsection of this chapter.
Read more information about acute post streptococcal glomerulonephritis in the “Glomerulonephritis” section of the “Renal and Urinary System Alterations” chapter of Open RN Health Alterations.
Pathophysiology
Impetigo occurs when the skin becomes infected. The most common cause is bacteria with Staphylococcus aureus being a primary culprit. Other bacteria that can lead to impetigo are Group A beta-hemolytic Streptococcus (GABHS) and methicillin-resistant Staphylococcus aureus (MRSA). Primary impetigo occurs when there is direct invasion of normal skin, and secondary impetigo occurs at the site of a previous open wound. Once inside the superficial layers of the skin, the bacteria multiply, resulting in inflammation and infection. The infection can then easily spread to other parts of the body.[4],[5]
Assessment (Recognize Cues)
Physical Exam
The two types of impetigo present differently. Nonbullous impetigo starts with a vesicle or pustule that eventually ruptures. Discharge from the lesion forms a crust that has a characteristic honey color that can be seen in Figure 16.16.[6] The base of the lesion is red. Lesions are most common on the face, extremities, or where skin breakdown previously occurred and rapidly spread to other areas due to self-contamination. Clients with nonbullous impetigo may also have a fever and enlarged lymph nodes.[7]

Bullous impetigo starts with small vesicles that progress to bullae (large blisters), as seen in Figure 16.17.[8] The bullae contain a fluid that can be clear, yellow, purulent, or dark. They will eventually rupture, but do not create a honey-colored crust. Bullous impetigo typically forms in areas with skin folds or the axilla and can also be present inside the mouth.[9]

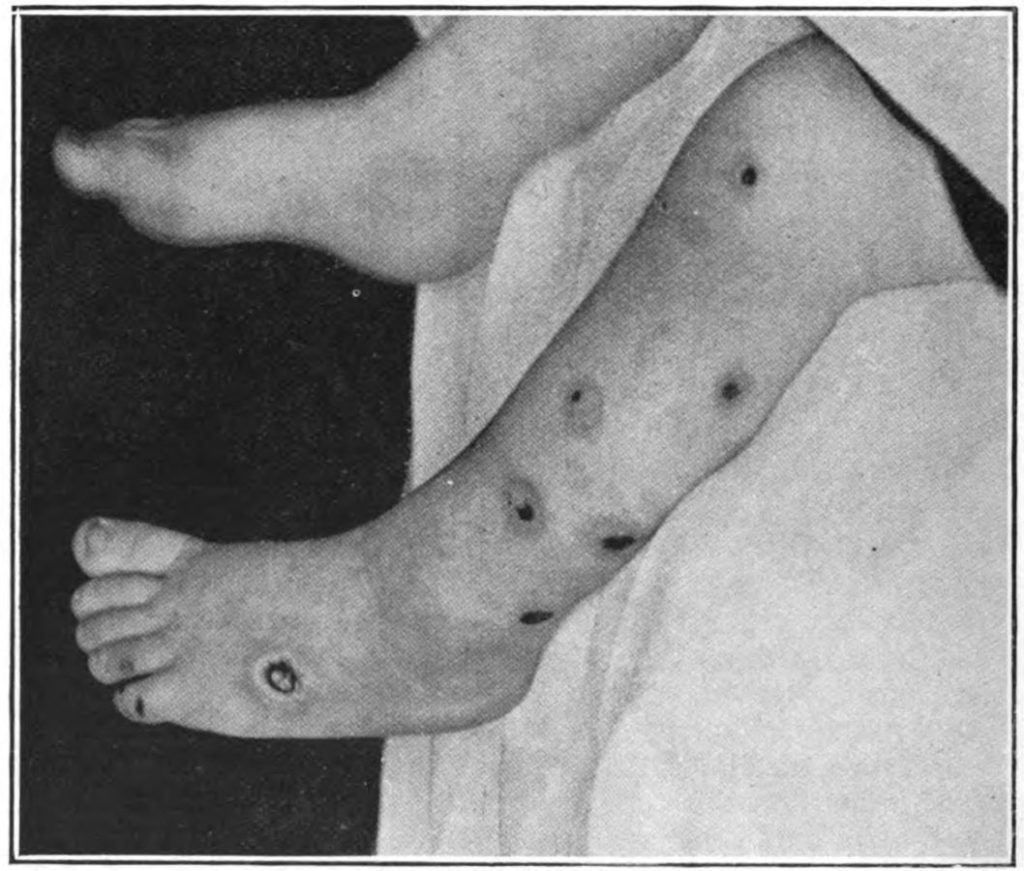
A subset of bullous impetigo is ecthyma. Ecthyma affects deeper layers of skin and leads to deep lesions as can be seen in Figure 16.18.[10] Lesions can produce crusts with varying colors such as honey-colored, brown, or black. Purulent exudate may also be present.[11]
Common Laboratory and Diagnostic Tests
Impetigo is diagnosed based on a physical exam and can be confirmed by obtaining a culture of the lesion to determine the causative bacteria. If impetigo is not responsive to treatment, a skin biopsy may be required.[12]
Diagnosis (Analyze Cues)
Nursing priorities for clients with impetigo include symptom management and the prevention of complications.
Nursing diagnoses for clients with impetigo are created based on the specific needs of the client, their signs and symptoms, and the etiology of the disorder. These nursing diagnoses guide the creation of client-specific care plans that encompass client outcomes and nursing interventions, as well the evaluation of those outcomes. These individualized care plans then serve as a guide for client treatment. Possible nursing diagnoses for clients with impetigo are as follows[13]:
- Impaired skin integrity r/t disease process
- Risk for infection r/t potential for self-contamination
- Hyperthermia r/t disease process
Outcome Identification (Generate Solutions)
Outcome identification encompasses the creation of short- and long-term goals for the client. These goals are used to create expected outcome statements that are based on the specific needs of the client. Expected outcomes should be specific, measurable, achievable, relevant, and timebound (SMART) within a set time frame based on the application of appropriate nursing interventions.
Sample expected outcomes for impetigo include the following:
- The client will exhibit intact skin with minimal scarring by the end of the disease course.
- The skin of the client will not exhibit signs of secondary infection during the course of the illness.
- The client will exhibit a temperature that is within normal limits for age within 24 hours of medical treatment.
Implementation (Take Action)
Medical Interventions
Impetigo is treated with topical and/or systemic antibiotics. Although impetigo often resolves without treatment, antibiotics help prevent spread to other areas of the body, shorten the duration of the disorder, and prevent the development of complications. Topical antibiotics are often sufficient for nonbullous impetigo, but crusts must first be removed with soap and water before applying the antibiotic. Systemic antibiotics are required for bullous impetigo, ecthyma, and widespread nonbullous impetigo. When impetigo recurs due to bacteria colonizing the nares, nasal mupirocin is typically prescribed as well.[14]
Nursing Interventions
Registered nurses develop interventions based on the expected outcomes of the client. Prior to implementation, the nurse must determine if all previously planned interventions are still suitable based on the current situation of the client. When caring for a client with impetigo, nursing interventions can be divided into nursing assessments, nursing actions, and client teaching, as described in the following subsections.[15],[16]
Nursing Assessments
- Assess the skin lesions and document type of lesion, exudate, and locations.
- Assess kidney function in cases caused by GABHS because acute poststreptococcal glomerulonephritis is a potential complication.
Nursing Actions
- Administer antibiotics per provider order, ensuring that scabs/crusts are removed prior to topical application to promote absorption of the medication.
- Ensure that the client has trimmed fingernails because long fingernails carry bacteria and promote the spread of infection.
Client Teaching
- Teach the client and their caregivers that good hygiene is essential during the course of impetigo. Hands should be washed frequently, as well as anything that may have come into contact with the lesions. Open lesions should be covered with a Band-Aid to prevent spread of infection. Lesions should not be touched or scratched.
- Teach the client and their caregivers that children with impetigo should avoid other children during active infection. Children may return to school or daycare after one to two days of antibiotic therapy.
- Educate the client and their family about the need to finish the entire course of antibiotics as prescribed to prevent infection recurrence and antibiotic resistance.
Review general nursing interventions related to caring for an ill child in the “Planning Care for the Ill Child” chapter.
Evaluation (Evaluate Outcomes)
Evaluation of client outcomes refers to the process of determining whether or not client outcomes were met by the indicated time frame. This is done by reevaluating the client as a whole and determining if their outcomes have been met, partially met, or not met. If the client outcomes were not met in their entirety, the care plan should be revised and reimplemented. Evaluation of outcomes should occur each time the nurse assesses the client, examines new laboratory or diagnostic data, or interacts with another member of the client’s interdisciplinary team.
- Nardi, N. M., & Schaefer, T. J. (2023). Impetigo. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK430974/ ↵
- Nardi, N. M., & Schaefer, T. J. (2023). Impetigo. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK430974/ ↵
- Nardi, N. M., & Schaefer, T .J. (2023). Impetigo. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK430974/ ↵
- Nardi, N. M., & Schaefer, T. J. (2023). Impetigo. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK430974/ ↵
- Cleveland Clinic. (2023). Impetigo. https://my.clevelandclinic.org/health/diseases/15134-impetigo ↵
- “Impetigo2020” by James Heilman, MD is licensed under CC BY-SA 4.0 ↵
- Nardi, N. M., & Schaefer, T. J. (2023). Impetigo. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK430974/ ↵
- “Impetigo_contagusum_,bulbous_impetigo_new_photo_for_diagnosis” by Masryyy is licensed under CC BY-SA 4.0 ↵
- Nardi, N. M., & Schaefer, T. J. (2023). Impetigo. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK430974/ ↵
- “An_introduction_to_dermatology_(1905)_ecthyma” by Norman Purvis Walker is in the Public Domain. ↵
- Nardi, N. M., & Schaefer, T. J. (2023). Impetigo. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK430974/ ↵
- Nardi, N. M., & Schaefer, T. J. (2023). Impetigo. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK430974/ ↵
- Curran, A. (2022). Impetigo nursing diagnosis and care plan. NurseStudy. https://nursestudy.net/impetigo-nursing-diagnosis/ ↵
- Nardi, N. M., & Schaefer, T. J. (2023). Impetigo. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK430974/ ↵
- Curran, A. (2022). Impetigo nursing diagnosis and care plan. NurseStudy. https://nursestudy.net/impetigo-nursing-diagnosis/ ↵
- Nardi, N. M., Schaefer, T. J., & Espil, M. O. (2023). Impetigo (Nursing). StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK568809/ ↵
A contagious condition in which there is an infection in the outermost layers of the skin.
A subset of bullous impetigo that affects the deeper layers of skin.

