15.7 Pharyngitis, Tonsillitis, & Adenoiditis
Pharyngitis refers to inflammation of the pharynx or throat, and tonsillitis refers to inflammation of the tonsils. Although there is a distinction between the two disorders, they can coexist. When both the throat and tonsils are inflamed, it is referred to as pharyngotonsillitis. Both disorders are commonly referred to as a “sore throat” and have similar pathophysiologies, signs and symptoms, and treatment. At times, adenoiditis, or inflammation of the adenoids, also occurs with pharyngitis and/or tonsillitis.
Pharyngitis and tonsillitis are typically caused by bacterial or viral infections. However, pharyngitis can also be caused by allergies, acid reflux, or cancer. Common viral causes of pharyngitis and tonsillitis are rhinovirus, coronavirus, and adenovirus. Although there are a variety of bacteria that can lead to pharyngitis or tonsillitis, the most common is Group A beta-hemolytic streptococcus (GABHS), also called GBS. This is also known as “strep throat” and is common in school-aged children. Adenoiditis can be caused by an infectious process, allergies, or acid reflux.[1],[2],[3],[4],[5]
Pathophysiology
In both pharyngitis and tonsillitis, the causative bacteria or virus directly invades the mucosal tissue. The infectious agent multiplies and leads to inflammation and edema. Some viral causes, such as rhinovirus, can also cause additional irritation due to an increase in nasal secretions. Sometimes, an initial viral infection can later develop into a secondary bacterial infection.[6],[7]
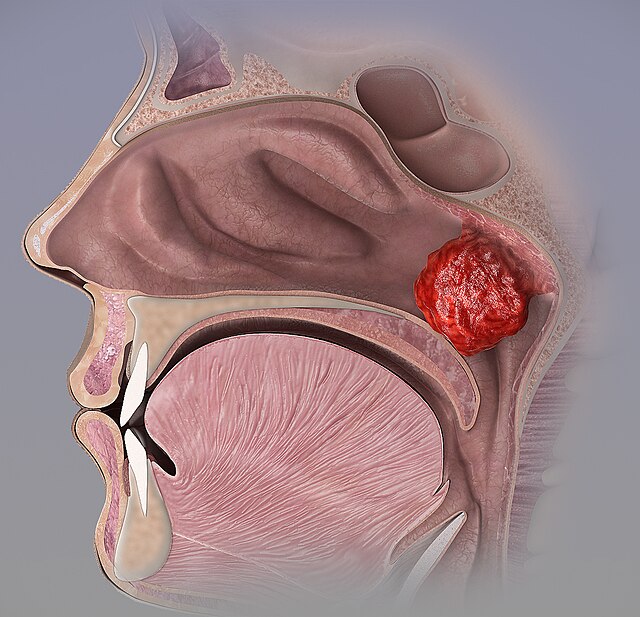
Acute adenoiditis occurs when bacteria multiply and spread to the adenoid tissue, often following a URI. This leads to excessive development of exudate and the resulting symptoms. If the adenoids become chronically inflamed, they can increase in size and lead to further issues.[8] See Figure 15.4[9] for an image of hypertrophied adenoids blocking the nasal passage.
Assessment (Recognize Cues)
Physical Exam
Clients with pharyngitis and/or tonsillitis can present with the following:
- Sore throat
- Fever
- Exudate on the tonsils
- Red and swollen tonsils
- Difficult or painful swallowing
- Enlarged and painful cervical lymph nodes
- Throat redness
- Ear pain
See Figure 15.5[10] for an image of tonsillitis with exudate. Symptoms can also vary based on whether pharyngitis is caused by a virus or bacteria. With viral infections, associated symptoms such as coughing, runny nose, headache, rash, and conjunctivitis (inflammation of the conjunctiva or outer lining of the eye) often occur. Bacterial causes have a faster onset of symptoms and are not associated with viral symptoms, such as a cough or runny nose. Pharyngitis caused by GABHS may also cause edema of the uvula and petechiae on the roof of the mouth.

Clients with adenoiditis can have the following symptoms[11]:
- Excessive nasal drainage
- Post-nasal drip
- Snoring
- Increased temperature
- Bad breath
- Difficulty breathing through the nose, leading to mouth breathing
Potential complications of pharyngitis and tonsillitis include spread of the infection to nearby structures, leading to epiglottitis, an ear infection, sinusitis, infection of the mastoid bone, and abscess formation. Potential complications of untreated adenoiditis are obstructive sleep apnea due to hypertrophy, otitis media with effusion, hearing loss, and speech issues.[12]
When pharyngitis and/or tonsillitis caused by GABHS is not treated, scarlet fever, post-streptococcal glomerulonephritis, or pediatric autoimmune neuropsychiatric disorders (PANDAS) can develop. Scarlet fever is an inflammatory disease that causes inflammation of the joints and the valves of the heart. Classic symptoms of scarlet fever are a bright red rash that covers most of the body and a high fever. Scarlet fever is further discussed in the “Other Respiratory Disorders” section. Post-streptococcal glomerulonephritis refers to inflammation of the glomeruli of the kidneys, leading to edema, increased blood pressure, and alterations in kidney function. PANDAS is triggered by an autoimmune reaction when the antibodies produced by a child’s immune system attack the brain and cause symptoms of tic disorder or obsessive-compulsive disorder.[13],[14],[15],[16],[17]
Read more information about “Glomerulonephritis” in the “Renal and Urinary System Alterations” chapter of Open RN Health Alterations.
Read more information about PANDAS and “Obsessive-Compulsive Disorder” in the “Mental Health Conditions” chapter.
Common Laboratory and Diagnostic Tests
To determine if laboratory testing is needed for a client with a sore throat, health care providers may use Centor criteria to establish a level of suspicion for a bacterial cause. Centor criteria assign point values to various criteria such as age, tonsillar swelling or exudates, tender cervical lymph nodes, fever, and lack of cough as described in Table 15.7. When adding the points assigned from the Centor criteria, the higher the point value, the more likely the infection is to be caused by strep bacteria. A score of 0-1 indicates that further testing and antibiotics are not needed, but a score of 2-3 means that a rapid antigen test or throat culture should be performed for GABHS. Additionally, the health care provider should also assess for known exposure to strep throat within the past two weeks to aid in diagnosis. However, the Infectious Disease Society of America recommends testing all clients who present with pharyngitis for a bacteria cause unless a clear viral cause can be determined. When the decision is made to test for GABHS, rapid antigen tests can be performed with quick results, but false negative results can occur. For pediatric clients, a negative test is followed with a throat culture.[18],[19],[20] See Figure 15.6[21] for an image of a client’s tonsils being swabbed for a culture specimen.
Table 15.7. Centor Criteria
| Centor Criteria | Points |
|---|---|
| Age 3-14 years | 1 |
| Tonsillar swelling or exudates | 1 |
| Tender/swollen anterior cervical lymph nodes | 1 |
| Temperature > 38° C or 100.4°F | 1 |
| Absence of cough | 1 |
| Scoring: 2 or more points requires GABHS testing |
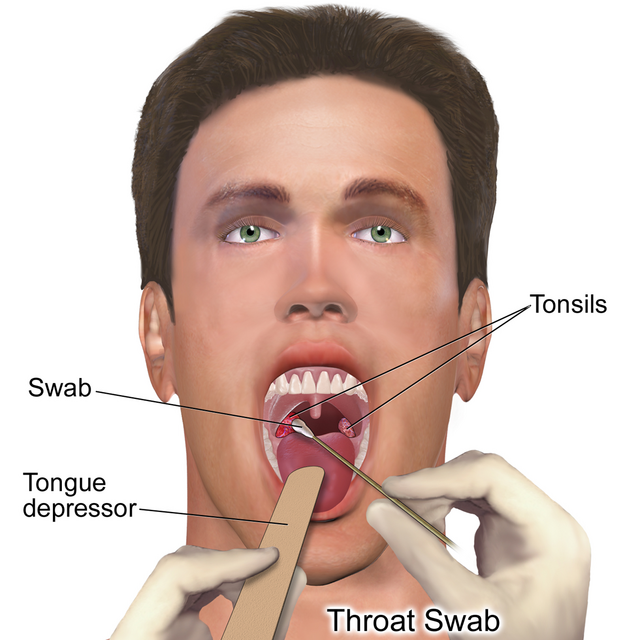
Figure 15.6 Swabbing Tonsils for Culture Specimen
Diagnostic imaging and additional lab work may be ordered if complications are suspected, such as respiratory compromise or abscess formation. Imaging may also be performed to assess for enlarged adenoids.[22],[23],[24]
Diagnosis (Analyze Cues)
Nursing priorities for clients with pharyngitis and/or tonsillitis include symptom management, the prevention of complications, and controlling the spread of illness.
Nursing diagnoses for clients with pharyngitis and/or tonsillitis are created based on the specific needs of the client, their signs and symptoms, and the etiology of the disorder. These nursing diagnoses guide the creation of client-specific care plans that encompass client outcomes and nursing interventions, as well the evaluation of those outcomes. These individualized care plans then serve as a guide for client treatment.
Possible nursing diagnoses for clients with pharyngitis and tonsillitis are as follows[25],[26]:
- Acute pain r/t inflammation of the throat and/or tonsils
- Hyperthermia r/t disease process
- Risk for ineffective airway clearance r/t inflammation of the throat and/or tonsils
- Risk for deficient fluid volume r/t poor oral intake
Outcome Identification (Generate Solutions)
Outcome identification encompasses the creation of short- and long-term goals for the client. These goals are used to create expected outcome statements that are based on the specific needs of the client. Expected outcomes should be specific, measurable, and realistic. These outcomes should be achievable within a set time frame based on the application of appropriate nursing interventions.
Sample expected outcomes for some of the above nursing diagnoses are listed below:
- The client will exhibit a reduction in pain using a numeric scale, such as FACES or FLACC, within one hour.
- The client will exhibit a temperature that is within normal limits for age within 24 hours.
- The client will exhibit a patent airway and no signs of respiratory distress during the course of the illness.
- The client will exhibit blood pressure and heart rate within normal limits for age, moist mucous membranes, urine output appropriate for their age, and non-sunken fontanels for infant clients during the course of the illness.
Implementation (Take Action)
Medical Interventions
Medical treatment for pharyngitis and tonsillitis is based on the causative factor of the disorder. When caused by a bacterial infection such as GABHS, antibiotics are required. However, antibiotic therapy is ineffective if the causative organisms are viral or fungal. Antibiotics will not only treat the bacterial infection but also shorten the duration of the illness and prevent the development of scarlet fever and other complications. The client is no longer considered to be infectious when they have been on antibiotic therapy for 24 hours. It is important for the client or their parents/caregivers to understand that the client must finish the antibiotic treatment as prescribed and not stop when feeling better or no longer infectious. Failure to complete an antibiotic regimen as prescribed places the client at risk for recurrence of infection and development of antibiotic-resistant infections.
Regardless of whether the infection is bacterial or viral, steroids may be prescribed to decrease the severity of symptoms, but their use is controversial. Supportive care such as the use of over-the-counter pain relievers (acetaminophen or ibuprofen) and saltwater gargles can also be used. Additionally, throat lozenges or throat sprays that contain benzocaine or lidocaine can be used in older children to relieve pain by numbing the throat. Adequate hydration is essential, and the client should remain on a liquid diet until pain improves.
For clients with recurrent tonsillitis (five or more episodes over the span of a year), a tonsillectomy, or surgical removal of the tonsils, may be warranted. Depending on the client situation, the adenoids may or may not also be removed during this surgery. In those with recurrent tonsillitis, tonsil removal has been shown to reduce school absences, sore throats, and further infections. See the following box for information post-tonsillectomy care.
Tonsillectomy Care[27],[28],[29],[30],[31]
Preoperative Tonsillectomy Health Teaching
- A tonsillectomy will be performed under general anesthesia.
- The client should be NPO at midnight before surgery to prevent aspiration.
- Ten to fourteen days of recovery time may be needed. Postoperative issues that may occur are pain, nausea, vomiting, mild fever, bad breath, swelling, and a feeling that something is stuck in the throat. Pediatric clients may experience anxiety or sleep problems. Strenuous activities should be avoided in the initial days after surgery.
- A tonsillectomy is generally an outpatient procedure, but an overnight stay may be required if complications develop.
Postoperative Tonsillectomy Teaching/Care
- Position the client in a prone or side-lying position to prevent the aspiration of blood or saliva.
- Keep suction equipment at the bedside in the event that clots form at the surgical site and block the client’s airway.
- Encourage the client to perform deep breathing exercises to prevent the risk of post-surgical pneumonia.
- Administer medications, such as pain relievers, antibiotics, or IV fluids, per provider order.
- Monitor for excessive swallowing or bright red blood coming from the nose or mouth, as these could indicate bleeding from the surgical site.
- Provide clear and cold fluids in small amounts, but avoid red, purple, and brown colors because they can be misinterpreted as blood if vomiting occurs. Soft foods are started per provider order, typically after postoperative Day 1.
- Avoid the use of straws or sharp objects such as forks, as they can potentially damage the surgical site and lead to bleeding.
- Discourage throat clearing, nose blowing, and coughing because they can cause surgical site bleeding.
- Administer antiemetics as prescribed to prevent vomiting because it can lead to surgical site bleeding.
- Monitor for postoperative complications such as bleeding, a high fever, signs of dehydration, or difficulty breathing.
Nursing Interventions
Registered nurses plan interventions based on the expected outcomes of the client. Prior to implementation, the nurse must determine if all previously planned interventions are still suitable based on the current situation of the client.
When caring for a client with pharyngitis or tonsillitis, nursing interventions can be divided into nursing assessments, nursing actions, and client teaching as described in the following subsections.[32],[33],[34],[35]
Nursing Assessments
- Assess the client for signs of poor oxygenation such as increased respiratory rate, increased heart rate, confusion, pallor, or irritability. Poor oxygenation can occur due to respiratory compromise as a result of swelling in the tonsils or throat.
- Assess pain using an age-appropriate scale like FACES or FLACC to determine the need for analgesics.
- Assess the client’s intake and output and vital signs to determine if a fluid volume deficit exists due to poor oral intake.
- If GABHS is the causative factor, monitor for signs of potential complications such as scarlet fever, glomerulonephritis, and PANDAS.
- Assess for signs of clinical deterioration, progression of illness, or development of complications.
Nursing Actions
- Encourage the client to increase fluids to prevent the throat from becoming dry. A dry throat will make swallowing more difficult.
- Encourage the client to avoid dairy products such as milk, ice cream, and pudding, as they can leave a coating on the throat, which leads to coughing in an attempt to clear the throat. Foods that are coarse, spicy, or hot should also be avoided as they can increase pain.
- Encourage the application of ice to the neck or the intake of popsicles, as they will decrease swelling and pain.
- Encourage the use of over-the-counter medications such as acetaminophen or ibuprofen to relieve pain.
- Encourage adequate rest to allow the body to heal.
- Promote the use of a humidifier, as more moisture in the air can help reduce discomfort.
Client Teaching
- Educate the client and their caregivers about proper handwashing and respiratory etiquette to help prevent the spread of infection to others.
- Educate the client and their caregivers that pharyngitis and tonsillitis can be caused by either viruses or bacteria and only bacterial infections require the use of antibiotics.
- Educate the client and their caregivers on the importance of completing the entire course of antibiotics if prescribed. This prevents not only antibiotic resistance but also helps prevent the development of complications such as scarlet fever.
- If warranted, educate the client and their caregivers about tonsillectomy care.
Review general nursing interventions that relate to caring for an ill child in the “Planning Care for the Ill Child” chapter.
Evaluation (Evaluate Outcomes)
Evaluation of client outcomes refers to the process of determining whether or not client outcomes were met by the indicated time frame. This is done by reevaluating the client as a whole and determining if their outcomes have been met, partially met, or not met. If the client outcomes were not met in their entirety, the care plan should be revised and reimplemented. Evaluation of outcomes should occur each time the nurse assesses the client, examines new laboratory or diagnostic data, or interacts with another member of the client’s interdisciplinary team.
- Johns Hopkins Medicine. (n.d.). Pharyngitis and tonsillitis. https://www.hopkinsmedicine.org/health/conditions-and-diseases/pharyngitis-and-tonsillitis ↵
- Anderson, J., & Paterek, E. (2023). Tonsillitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK544342/ ↵
- Wolford, R. W., Goyal, A., Belgam Syed, S. Y., et al. (2023). Pharyngitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK519550/ ↵
- Ashurst, J. V., & Edgerley-Gibb, L. (2023). Streptococcal pharyngitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK525997/ ↵
- Bowers, I., & Shermetaro, C. (2023). Adenoiditis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK536931/ ↵
- Johns Hopkins Medicine. (n.d.). Pharyngitis and tonsillitis. https://www.hopkinsmedicine.org/health/conditions-and-diseases/pharyngitis-and-tonsillitis ↵
- Anderson, J., & Paterek, E. (2023). Tonsillitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK544342/ ↵
- Bowers, I., & Shermetaro, C. (2023). Adenoiditis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK536931/ ↵
- “Adenoid_hypertrophy” by www.scientificanimations.com is licensed under CC BY-SA 4.0 ↵
- “Tonsillitis_Img” by Nick Berman is licensed under CC BY-SA 4.0 ↵
- Bowers, I., & Shermetaro, C. (2023). Adenoiditis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK536931/ ↵
- Bowers, I., & Shermetaro, C. (2023). Adenoiditis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK536931/ ↵
- Anderson, J., & Paterek, E. (2023). Tonsillitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK544342/ ↵
- Wolford, R. W., Goyal, A., Belgam Syed, S. Y., et al. (2023). Pharyngitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK519550/ ↵
- Ashurst, J. V., & Edgerley-Gibb, L. (2023). Streptococcal pharyngitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK525997/ ↵
- Mayo Clinic. (2022). Scarlet fever. https://www.mayoclinic.org/diseases-conditions/scarlet-fever/symptoms-causes/syc-20377406 ↵
- National Institute of Mental Health. (2019). PANDAS: Questions and answers. https://www.nimh.nih.gov/health/publications/pandas ↵
- Anderson, J., & Paterek, E. (2023). Tonsillitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK544342/ ↵
- Wolford, R. W., Goyal, A., Belgam Syed, S. Y., et al. (2023). Pharyngitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK519550/ ↵
- Ashurst, J. V., & Edgerley-Gibb, L. (2023). Streptococcal pharyngitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK525997/ ↵
- “Throat_Culture” by BruceBlaus is licensed under CC BY-SA 4.0 ↵
- Anderson, J., & Paterek, E. (2023). Tonsillitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK544342/ ↵
- Wolford, R. W., Goyal, A., Belgam Syed, S. Y., et al. (2023). Pharyngitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK519550/ ↵
- Ashurst, J. V., & Edgerley-Gibb, L. (2023). Streptococcal pharyngitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK525997/ ↵
- Curran, A. (2022). Tonsillitis nursing diagnosis and nursing care plan. https://nursestudy.net/tonsillitis-nursing-diagnosis/?expand_article=1 ↵
- Curran, A. (2023). Strep throat nursing diagnosis and care plan. https://nursestudy.net/strep-throat-nursing-diagnosis/?expand_article=1 ↵
- Anderson, J., & Paterek, E. (2023). Tonsillitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK544342/ ↵
- Wolford, R. W., Goyal, A., Belgam Syed, S. Y., et al. (2023). Pharyngitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK519550/ ↵
- Ashurst, J. V., & Edgerley-Gibb, L. (2023). Streptococcal pharyngitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK525997/ ↵
- Martin, P. (2024). 4 tonsillitis nursing care plans. https://nurseslabs.com/tonsillitis-nursing-care-plans/ ↵
- Mayo Clinic. (2022). Tonsillectomy. https://www.mayoclinic.org/tests-procedures/tonsillectomy/about/pac-20395141 ↵
- Wolford, R. W., Goyal, A., Belgam Syed, S. Y., et al. (2023). Pharyngitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK519550/ ↵
- Ashurst, J. V., & Edgerley-Gibb, L. (2023). Streptococcal pharyngitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK525997/ ↵
- Martin, P. (2024). 4 tonsillitis nursing care plans. https://nurseslabs.com/tonsillitis-nursing-care-plans/ ↵
- Mayo Clinic. (2022). Tonsillectomy. https://www.mayoclinic.org/tests-procedures/tonsillectomy/about/pac-20395141 ↵
Inflammation of the pharynx.
Inflammation of the tonsils.
Inflammation of the pharynx and tonsils.
Inflammation of the adenoids.
Inflammation of the conjunctiva or outer lining of the eye.
A disorder that affects the valves of the heart and is caused by an untreated strep infection.
Inflammation of the glomerulus of the kidneys as a result of an untreated strep infection; leads to edema, increased blood pressure and alterations in kidney function.
An autoimmune reaction triggered by antibodies produced by a child’s immune system that attack the brain and causes symptoms of tic disorder or obsessive-compulsive disorder.
Surgical removal of the tonsils.

