12.3 Common Complications During the Neonatal Period
Several common complications can occur during the neonatal period, including impaired thermoregulation, hypoglycemia, jaundice, and feeding and nutrition issues. Nurses monitor for signs of these complications and promptly report concerns to the health care provider.
Impaired Thermoregulation
External Factors
There are four external factors that contribute to heat loss in a newborn called evaporation, conduction, radiation, and convection. Nurses must understand these factors so that actions can be taken to reduce their impact:
- Evaporation causes heat loss as amniotic fluid or other fluids dry on the newborn’s skin.
- Conduction causes heat loss anytime the newborn is placed in direct contact with a cooler surface, such as a scale or cold mattress.
- Radiation causes heat loss when the newborn is placed near cooler objects, such as an outside wall or window.
- Convection causes heat loss from moving cool air, such as a fan or draft.
Physiological Factors
Several physiological factors contribute to a newborn’s inability to regulate their body temperature compared to an adult, such as a large body surface area in relation to their weight, thin skin with blood vessels near the surface, and minimal subcutaneous fat. Newborns also lack sufficient skeletal muscle mass to effectively increase body temperature through shivering.[1] As a result, newborns are at risk for losing heat, with smaller or premature infants being at even higher risk.
Newborns maintain their body temperature mainly through vasoconstriction, which keeps heat within the core of the body, and nonshivering thermogenesis that involves the metabolism of brown fat. Brown fat develops progressively during the third trimester and is mostly located around the neck, axillae, back, abdomen, and thighs. When thermal sensors in the skin detect a decrease in environmental temperature, metabolism of brown fat produces heat by increasing the metabolic rate and consumption of oxygen.[2] This response can lead to cold stress.
Hypothermia and Cold Stress
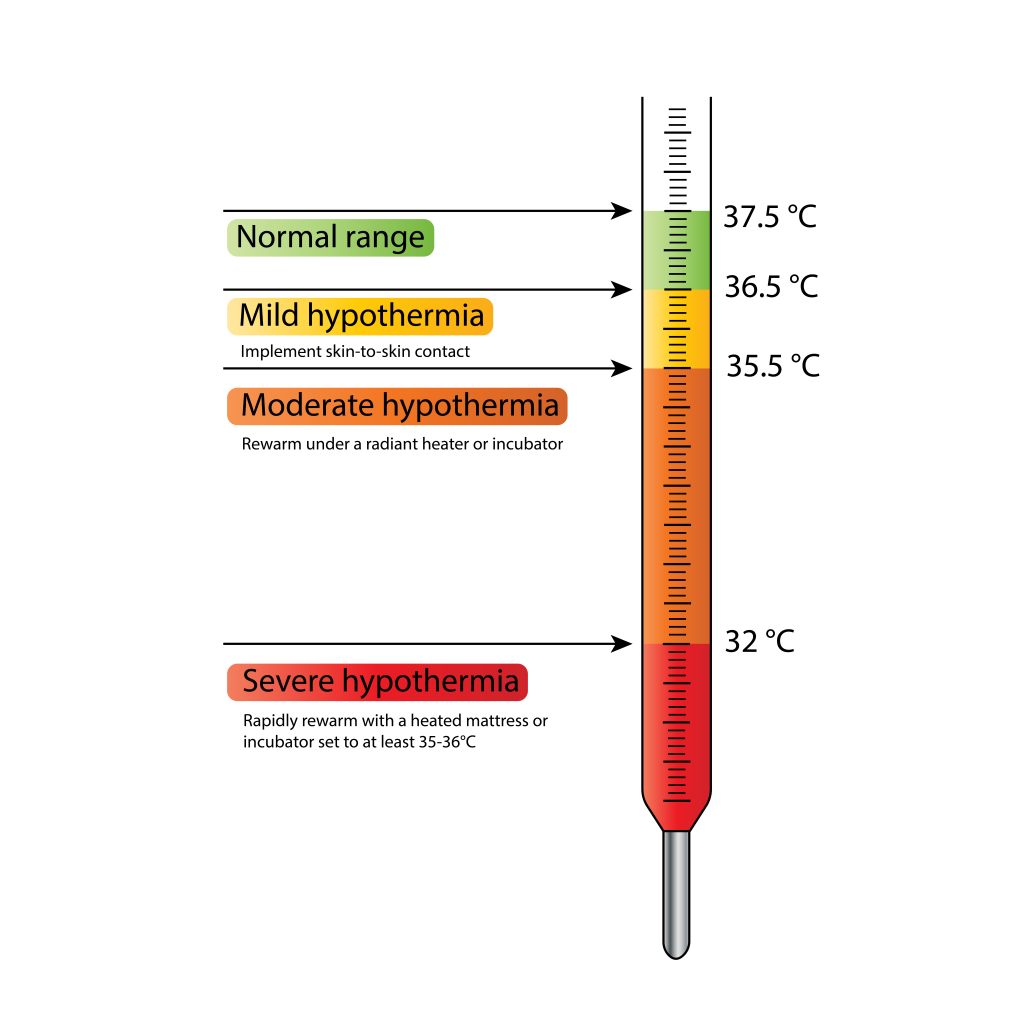
Nurses monitor newborns closely for signs of cold stress and hypothermia and act appropriately to stabilize their temperature. Cold stress and mild hypothermia in newborns is defined as temperature below 36.5°C (97.7°F) but above 35.5°C. Moderate hypothermia is 32.0°C to 34.9°C. Severe hypothermia is less than 32.0°C. See Figure 12.3[3] for an illustration of mild, moderate, and severe hypothermia.
Nursing Assessments and Interventions
Immediately after birth, newborns start losing heat due to evaporation and entering an environment much cooler than the womb. The nurse must ensure that heat loss is prevented, or hypothermia may develop that can result in a cascade of complications.[4],[5]
Given the risk, nurses closely monitor the newborn’s temperature and take steps at birth and in the days following to ensure the infant does not become hypothermic (i.e., temperature below 36.5°C/97.7°F) or hyperthermic (i.e., temperature above 37.5°C/99.5°F). Providing a thermoneutral environment helps the newborn maintain their body temperature, thereby reducing their expenditure of energy and consumption of oxygen and preventing the adverse effects of impaired thermoregulation.[6],[7]
Newborns with mild hypothermia have cool extremities, tend to be less active, and may not feed effectively. They often have a weak cry and rapid or labored breathing. Hypothermia can also cause hypoglycemia because of the increased amount of energy required to produce body heat. Effects of cold stress in the newborn include increased metabolic rate, oxygen consumption, and glucose utilization, which may lead to hypoglycemia. Increased anaerobic metabolism, which causes increased fatty acids, can lead to high levels of bilirubin in the blood, known as hyperbilirubinemia. Increased demand for oxygen can cause respiratory distress and lead to hypoxemia. Nursing interventions for mild hypothermia include rewarming through skin-to-skin contact with the mother in a warm room.
Newborns with moderate or severe hypothermia often have a decreased heart rate and difficulty breathing, with decreased respiratory rate and depth of respirations. As worsening hypothermia causes worsening hypoglycemia, metabolic acidosis can occur. Nursing interventions for moderate hypothermia include rewarming under a radiant heater or incubator set at 35-36° C (95-96.8°F). If a warmer is not available, the newborn can remain skin-to-skin with the mother in a room at least 77°F. Newborns with severe hypothermia require rapid rewarming with a heated mattress or incubator set to at least 35-36°C/95-96.8°F.
The World Health Organization identified “The Warm Chain” as a set of actions that can be taken to protect the newborn from the effects of hypothermia at birth and the following few days to minimize the risks for heat loss[8],[9]:
- Warm delivery room: Ensure the room is between 77-82.4°F and free of drafts or fans.
- Immediate drying: Dry the entire body with a towel within five seconds of birth. Cover the newborn with a second towel and place a hat on their head.
- Skin-to-skin contact: Immediately after delivery, place the newborn with skin-to-skin contact on the parent’s abdomen or chest and cover them for 60-90 minutes. Skin-to-skin contact can also be used any time to keep the baby warm or to rewarm them if their temperature is slightly low. See Figure 12.4[10] for an image of skin-to-skin contact.

- Feeding: Encourage breastfeeding or formula feeding as soon as possible after birth because it provides calories to generate heat.
- Postpone weighing and bathing: Weighing should be postponed for several hours to prevent heat loss. Bathing should be delayed until the second or third day of life. Immediate bathing is unnecessary. Delayed bathing allows the vernix to prevent heat loss, and it can also be reabsorbed into the skin. Vernix is a cheese-like substance that covers the skin of the newborn and protects their sensitive skin in utero from prolonged exposure to amniotic fluid. However, if cultural beliefs prefer early bathing, it should be delayed at least 24 hours to prevent heat loss.
- Promote appropriate clothing: Newborns generally require one or two more layers of clothing than adults to stay warm, and a hat is helpful for preventing heat loss for at least the first few hours of life.
- Encourage mother and baby to be together: Skin-to-skin contact and breastfeeding on demand is easier when the mother and baby remain together in the hospital setting.
- Provide warm transportation: Ensure the newborn is kept warm when transferred from one area to another (i.e., from the delivery room to the postpartum room).
Hyperthermia
Hyperthermia in newborns is defined as a temperature above 37.5°C. Newborns are unable to perspire to reduce their body temperature, so factors such as high environmental temperature, excessive clothing or bedding, sleeping in a prone position, or sharing the bed with others can cause hyperthermia. Additionally, research shows that hyperthermia increases the risk for sudden infant death syndrome (SIDS), so it is critical for nurses to teach parents about taking measures to avoid hyperthermia.[11]
Hypoglycemia
After a newborn is delivered, they can no longer depend on the placenta for delivery of nutrients or on the uterus for temperature regulation, putting them at risk for hypoglycemia, especially during the first hours of life. Hypoglycemia in newborns is defined as a blood glucose level below 40 mg/dL. Like adults, newborns require glucose for energy and brain functioning. If hypoglycemia occurs, brain function can be severely affected, resulting in seizures and possible neurologic damage. Actions to prevent hypoglycemia include keeping the infant warm and early initiation of feeding. Newborns use prenatal stores of glucose until feedings are established, so hypoglycemia can be prevented by feeding immediately after birth.[12],[13]
Risk factors for hypoglycemia in newborns include maternal preeclampsia or gestational diabetes, a newborn who is small or large for their gestational age, a small twin, or those born with metabolic disorders. Nurses must be aware of these risk factors so they can initiate blood glucose screenings and monitor for signs of hypoglycemia. The Pediatric Endocrine Society recommends hypoglycemia screening for all infants with these identified risk factors.[14]
Signs of hypoglycemia in the newborn, in addition to hypothermia, include the following[15],[16]:
- Lethargy
- Apathy
- Limpness
- High-pitched or weak cry
- Irritability
- Tremors
- Apnea
- Respiratory distress
- Pallor
- Cyanosis
- Poor feeding
- Exaggerated Moro reflex
- Diaphoresis
- Seizures
- Coma
Depending on its severity, treatment for neonatal hypoglycemia may include breastfeeding, oral supplementation of formula, IV fluids (D10W, D12.5W), glucagon, and, in severe cases, corticosteroids. Nurses must be familiar with agency policy for screening, testing, and treatment of hypoglycemia in newborns.[17]
Hyperbilirubinemia and Jaundice
Hyperbilirubinemia, often referred to as jaundice, is a common complication seen in the newborn period. Jaundice can be physiological or pathological. To understand these conditions, it is helpful to review how the liver regulates bilirubin levels. Bilirubin is a byproduct of the natural breakdown of red blood cells. The liver conjugates bilirubin into a form that can be removed from the body. Typically, the majority of bilirubin is filtered out of the blood by the liver and is excreted in the stool. Jaundice occurs when bilirubin builds up faster in the blood than the liver can conjugate it for excretion from the body.
A newborn’s liver is immature and still developing after birth, so it may not be able to remove adequate amounts of bilirubin from the blood. When large amounts of bilirubin are present in the blood, excess amounts are deposited in the subcutaneous tissue, causing a yellow appearance of the skin and sclera. This yellowing is a hallmark sign of jaundice. See Figure 12.5[18] for an image of jaundice in a newborn. Newborns may present with additional signs of jaundice such being difficult to awaken or get to sleep, difficulty breast- or bottle-feeding, irritability and fussiness, or having few wet or soiled diapers.[19],[20]

Physiological jaundice is a normal process that occurs during the transition from intrauterine to extrauterine life. It is not present during the first 24 hours of life in term infants, but appears on the second or third day of birth. It resolves by two to three weeks as the neonatal liver matures and begins to effectively conjugate bilirubin. Additionally, the life span of red blood cells in infants is shorter and only about 90 days compared to 120 days in the adult, resulting in hyperbilirubinemia (increased bilirubin levels) due to the faster breakdown of these cells. Cephalhematoma or other bruising can also cause hyperbilirubinemia. Other factors that can contribute to physiological jaundice include prematurity and poor hydration from inadequate intake of breastmilk or formula. Poor intake decreases intestinal motility and the elimination of bilirubin in the stool. For healthy newborns with physiological jaundice, a wait-and-watch approach is generally prescribed while also ensuring they are feeding effectively.[21]
Pathological jaundice occurs when there are abnormally elevated levels of unconjugated and conjugated bilirubin. Pathological jaundice may occur during the first 24 hours of life. Unconjugated bilirubin levels in pathological jaundice tend to rise earlier and more quickly when compared to physiological jaundice. Elevated levels of conjugated bilirubin indicate impaired liver function and are always considered pathological.
The most common cause of pathological jaundice is blood group incompatibilities (ABO or Rh factor), where maternal antibodies cross the placenta and destroy the fetal red blood cells, also called hemolytic disease of the newborn. Read more about blood group incompatibilities in the following box. Another cause of pathological jaundice is glucose-6 phosphate dehydrogenase (G6PD) deficiency that causes the hemolysis of red blood cells when the newborn is exposed to a variety of illnesses, medications, foods, or dyes. Pathological jaundice can also be caused from significant cephalohematoma or bruising that causes increased hemolysis of red blood cells, infection, intrauterine growth restriction (IUGR), infants of diabetic mothers, large for gestational age (LGA) infants, and maternal smoking.[22]
Blood Group Incompatibilities
Rh incompatibility occurs when a mother who is Rh-negative is pregnant with a fetus who is Rh-positive. The mother’s immune system interprets the Rh proteins on the fetus’s red blood cells as foreign substances and creates antibodies against them. The mother’s antibodies can travel through the placenta and umbilical cord and destroy the fetus’s red blood cells. Bilirubin is released as red blood cells break down, causing elevated bilirubin levels, referred to as hemolytic disease of the newborn. The risk of Rh incompatibility occurring during an Rh-negative mother’s first pregnancy is rare due to the time it takes for her immune system to produce the antibodies, but Rh-positive fetuses in subsequent pregnancies may be affected.
ABO incompatibility occurs when a mother has Type O blood and the fetus has Type A, B, or AB blood. The immune systems of mothers with Type O blood interpret the proteins contained in Type A and Type B blood as foreign substances. If their fetus has Type A, B, or AB blood, their immune system creates antibodies against those proteins that destroy the fetus’s red blood cells, although the reaction tends to be milder than Rh incompatibility.
Signs of pathological jaundice must be recognized and treated early to prevent complications. A rare but serious complication of untreated jaundice is kernicterus, a type of brain damage caused by elevated bilirubin levels greater than 25 mg/dL. Bilirubin levels greater than 30 mg/dL can cause irreversible brain damage in newborns.[23]
Nurses assess the risk for hyperbilirubinemia with the use of a free tool called the BiliTool. BiliTool recommendations are based on AAP Clinical Practice Guidelines. The BiliTool assesses the need for treatment by considering the newborn’s hours of age, total bilirubin level, and gestational age.
View the BiliTool at https://bilitool.org/.
Treatment for hyperbilirubinemia may include phototherapy, a special type of light used to lower bilirubin levels in the newborn’s blood through a process called photooxidation. Photooxidation adds oxygen to the bilirubin so that it dissolves easily in water and can be more easily excreted. See Figure 12.6[24] for an image of phototherapy.

When caring for newborns receiving phototherapy treatment, the nurse must closely monitor the newborn to ensure safe treatment is provided. Newborns are placed in a bassinet or warmer, usually only wearing a diaper to expose as much skin as possible to the light. Newborns remain under the light continuously, except during feedings. Some facilities have phototherapy blankets that can be wrapped around the newborn so phototherapy treatment can continue while they are being fed or held. During therapy, patches or a special mask are used to protect the infant’s eyes, and the temperature must be monitored frequently to ensure they do not become overheated.[25]
In serious cases, exchange transfusion may be performed for newborns who have not responded to phototherapy and other interventions and are at a high risk of developing brain damage. During exchange transfusion, the newborn’s blood is replaced with donated blood to quickly lower bilirubin levels.
Feeding Issues
Complications related to feeding can occur in breast-fed or formula-fed newborns. For example, premature newborns may have difficulty feeding due to an inability to coordinate sucking, swallowing, and breathing. The most common feeding issue in newborns is ineffective breastfeeding. Successful breastfeeding requires effective actions by both the mother and the newborn, with timing of feedings and proper positioning being critical aspects. Early, effective breastfeeding helps to establish the mother’s milk supply to ensure the newborn is able to receive adequate nutrients. Proper positioning ensures the newborn is latched correctly to the nipple, allowing for optimal intake of milk by the newborn, as well as minimal discomfort for the mother. Nurses evaluate the effectiveness of breastfeeding through observation of feedings, as well as by monitoring the number of wet and soiled diapers and the weight of the newborn. Early intervention is critical when either the mother or newborn are experiencing difficulty with breastfeeding to prevent complications.
Read additional information about breastfeeding in the “Health Teaching” subsection of “Applying the Nursing Process and Clinical Judgment Model to Newborn Care” section of this chapter.
Brachial Plexus Injury
Neonatal brachial plexus palsy (NBPP) is an injury that happens at or before birth to the group of nerves in the newborn’s shoulder, known as the brachial plexus. When these nerves are damaged by pressure or stretching the head and neck or arm, it creates weakness known as palsy. Risk factors for NBPP are breech delivery, maternal obesity, large for gestational age (LGA) infant, or shoulder dystocia, which is difficulty delivering the newborn’s shoulders after the head is delivered. The incidence of NBPP has decreased due to increased cesarean section deliveries for difficult births.[26]
Signs of NBPP injury may include the following[27]:
- No movement in the newborn’s affected arm or hand
- Absent Moro reflex on the affected side
- Elbow held to the side of the body with the arm extended straight
- Decreased grip on the affected side
- Affected arm may flop when infant moved side-to-side
See Figure 12.7[28] for an image of an infant displaying a sign of NBPP with one arm extended at their side. The health care provider may order an X-ray to rule out a clavicle fracture, which can also cause limited newborn arm movement. However, a clavicle fracture does not cause nerve damage, and the X-ray will not show nerve damage.

Treatment for mild cases includes a referral to a physical therapist for gentle massage and range-of-motion exercises. Most infants recover from mild cases by three to four months of age. However, if there is no improvement by three to nine months, full recovery is less likely. Surgery such as nerve grafts or nerve transfers may be performed, but they are not always effective.[29]
Colic
Colic is diagnosed when an otherwise healthy baby cries for no apparent reason, and they are not easily soothed. Colicky babies appear to be in pain and scream with a red face, clenched fists, and extended or flexed legs. Even though they appear to be in pain, they eat well and gain weight normally. They typically get fussy about the same time every day, often in the late afternoon or evening. Colic starts a few weeks after birth, typically lasts four to six months, and becomes its worst at four to six weeks of age. There is no known cause for colic, although when babies cry, they may swallow air, which distends the abdomen. They may show relief after passing gas or a bowel movement. Other potential causes for fussiness are gastroesophageal reflux or hernia, but these conditions typically have associated signs such as fussiness after feeding, excessive spitting or vomiting, or insufficient weight gain.[30],[31],[32]
Colic adds stress to new and/or overtired parents. Nurses should acknowledge parental feelings of helplessness and frustration and teach methods to cope with colic. Table 12.3 provides an overview of possible contributing factors to colic and suggested actions. Parents should be instructed to contact the health care provider if the infant’s crying changes suddenly or it is associated with fever, vomiting, loose or bloody stools, or decreased movement. Parents should also be encouraged to ask for help and take a break when feeling frustrated. They should never shake the infant because it can cause serious brain damage and even death. They should seek help immediately if feeling depressed or having thoughts of harming the baby.[33],[34],[35]
Table 12.3. Contributing Factors for Colic and Ways to Cope[36],[37],[38]
| Contributing Factors | Suggested Actions |
|---|---|
| Gas or Indigestion |
|
| Overfeeding |
|
| Sensitivity to Formula |
|
| Overexcitement |
|

View a supplementary YouTube video[40] on tips for colic relief from the American Academy of Pediatrics at Colic Relief Tips & When to Call Your Pediatrician | AAP #AskThePediatrician.
Positional Plagiocephaly
Positional plagiocephaly is a condition where an infant develops flat spots on the head, often due to repeated pressure on the back of the head. While positioning infants to sleep in a supine position decreases the incidence of SIDS, it increases the incidence of positional plagiocephaly. Parents can prevent this condition by using alternative positioning throughout the waking hours. Examples of alternative positions are as follows[41]:
- Holding the infant upright
- Limiting time in seats with their heads against a surface
- Alternating the direction the baby lies in the crib or positioning the crib in various places around the room to encourage the infant to move their head and look at objects
Other conservative treatments include physical therapy, massage, and helmets.
- Lidell, M. E. (2019). Brown adipose tissue in human infants. Handbook of Experimental Pharmacology, 251, 107–123. https://doi.org/10.1007/164_2018_118. https://pubmed.ncbi.nlm.nih.gov/29675580/ ↵
- Carter, B. W., & Schucany, W. G. (2008). Brown adipose tissue in a newborn. Proceedings, Baylor University Medical Center, 21(3), 328-330. https://doi.org/10.1080%2F08998280.2008.11928419 ↵
- “Neonatal Hypothermia” by Meredith Pomietlo is licensed under CC BY 4.0 ↵
- Wood, T., Johnson, M., Temples, T., & Bordelon, C. (2022). Thermoneutral environment for neonates: Back to the basics. Neonatal Network, 41(5), 289-296. https://doi.org/10.1891/nn-2022-0003 ↵
- World Health Organization. (1997). Thermal protection of the newborn: A practical guide. World Health Organization. https://iris.who.int/handle/10665/63986 ↵
- Wood, T., Johnson, M., Temples, T., & Bordelon, C. (2022). Thermoneutral environment for neonates: Back to the basics. Neonatal Network, 41(5), 289-296. https://doi.org/10.1891/nn-2022-0003 ↵
- World Health Organization. (1997). Thermal protection of the newborn: A practical guide. World Health Organization. https://iris.who.int/handle/10665/63986 ↵
- Wood, T., Johnson, M., Temples, T., & Bordelon, C. (2022). Thermoneutral environment for neonates: Back to the basics. Neonatal Network, 41(5), 289-296. https://doi.org/10.1891/nn-2022-0003 ↵
- World Health Organization. (2024). Keeping the newborn warm. https://www.who.int/tools/essential-newborn-care-course/materials ↵
- “mom_baby-1000x500” by Benjamin Chan is licensed under CC BY-NC-SA 3.0. Access for free at https://www.the-good-times.org/science_technology/skin-to-skin-contact-for-newborns-essential-and-beneficial/ ↵
- Bach, V., & Libert, J-P. (2022). Hyperthermia and heat stress as risk factors for sudden infant death syndrome: A narrative review. Frontiers in Pediatrics, 10(816136). https://doi.org/10.3389/fped.2022.816136 ↵
- Wells-Beede, E. (2022). Nursing care of women, families and newborns. Texas A&M University. https://pressbooks.pub/nurs323/ ↵
- Abramowski, A., Ward, R., & Hamdan, A. H. (2023). Neonatal hypoglycemia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK537105/ ↵
- Abramowski, A., Ward, R., & Hamdan, A. H. (2023). Neonatal hypoglycemia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK537105/ ↵
- Wells-Beede, E. (2022). Nursing care of women, families and newborns. Texas A&M University. https://pressbooks.pub/nurs323/ ↵
- Abramowski, A., Ward, R., & Hamdan, A. H. (2023). Neonatal hypoglycemia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK537105/ ↵
- Wells-Beede, E. (2022). Nursing care of women, families and newborns. Texas A&M University. https://pressbooks.pub/nurs323/ ↵
- “2973816964_60175c6710_k.jpg” by rchristie / Ryan is licensed under CC BY-ND 2.0 ↵
- Wells-Beede, E. (2022). Nursing care of women, families and newborns. Texas A&M University. https://pressbooks.pub/nurs323/ ↵
- March of Dimes. (2024). Newborn jaundice. https://www.marchofdimes.org/find-support/topics/planning-baby/newborn-jaundice ↵
- Ansong-Assoku, B. (2024). Neonatal jaundice. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK532930/ ↵
- Ansong-Assoku, B. (2024). Neonatal jaundice. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK532930/ ↵
- Hamza, A. (2019). Kernicterus. Autopsy & Case Reports, 9(1). https://doi.org/10.4322%2Facr.2018.057 ↵
- “148288153_d0a8b491d7_b.jpg“ by Mike Blyth is license under CC BY-NC-SA 2.0 ↵
- Wong, R. J., & Bhutani, V. K. (2022). Patient education: Jaundice in newborn infants (beyond the basics). UpToDate. https://www.uptodate.com/ ↵
- MedlinePlus [Internet]. (2023). Brachial plexus injury in newborns. https://medlineplus.gov/ency/article/001395.htm ↵
- MedlinePlus [Internet]. (2023). Brachial plexus injury in newborns. https://medlineplus.gov/ency/article/001395.htm ↵
- “baby-303068_1920.jpg” by Cheryl Holt from Pixabay is licensed under CC0 ↵
- MedlinePlus [Internet]. (2023). Brachial plexus injury in newborns. https://medlineplus.gov/ency/article/001395.htm ↵
- HealthyChildren.org. (2024). Colic relief tips for parents. https://www.healthychildren.org/English/ages-stages/baby/crying-colic/Pages/Colic.aspx ↵
- MedlinePlus [Internet]. (2023). Colic and crying - Self-care. https://medlineplus.gov/ency/patientinstructions/000753.htm ↵
- FamilyDoctor.org. (2023). Colic. https://familydoctor.org/condition/colic/ ↵
- HealthyChildren.org. (2024). Colic relief tips for parents. https://www.healthychildren.org/English/ages-stages/baby/crying-colic/Pages/Colic.aspx ↵
- MedlinePlus [Internet]. (2023). Colic and crying - Self-care. https://medlineplus.gov/ency/patientinstructions/000753.htm ↵
- FamilyDoctor.org. (2023). Colic. https://familydoctor.org/condition/colic/ ↵
- HealthyChildren.org. (2024). Colic relief tips for parents. https://www.healthychildren.org/English/ages-stages/baby/crying-colic/Pages/Colic.aspx ↵
- MedlinePlus [Internet]. (2023). Colic and crying - Self-care. https://medlineplus.gov/ency/patientinstructions/000753.htm ↵
- FamilyDoctor.org. (2023). Colic. https://familydoctor.org/condition/colic/ ↵
- “baby-20339_1920.jpg” by PublicDomainPictures from Pixabay is licensed under CC0 ↵
- American Academy of Pediatrics. (2023, November 22). Colic relief tips & when to call your pediatrician | AAP #AskThePediatrician [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=b-2-Vg5POpQ ↵
- National Institute of Child Health and Human Development. (n.d.). Tummy time for a healthy baby. https://safetosleep.nichd.nih.gov/reduce-risk/tummy-time ↵
A process impacting newborn thermoregulation which causes heat loss as amniotic fluid or other fluids dry on the newborn’s skin.
A process impacting newborn thermoregulation which causes heat loss anytime the newborn is placed in direct contact with a cooler surface, such as a scale or cold mattress.
A process impacting newborn thermoregulation which causes heat loss when the newborn is placed near cooler objects, such as an outside wall or window.
A process impacting newborn thermoregulation that causes heat loss from moving cool air, such as a fan or draft.
Temperature below 36.5°C but above 35.5°C.
Temperature below 36.5°C but above 35.5°C.
Temperature 32.0°C to 34.9°C.
Temperature less than 32.0°C.
Temperature below 36.5°C/97.7°F.
Temperature above 37.5°C/99.5°F.
A set of actions that can be taken to protect the newborn from the effects of hypothermia at birth and the following few days to minimize the risks for heat loss.
A cheese-like substance that covers the skin of the newborn and protects their sensitive skin in-utero from prolonged exposure to amniotic fluid.
Temperature above 37.5°C.
A blood glucose level below 40 mg/dL.
Often referred to as jaundice, a common complication in the newborn period.
Occurs when bilirubin builds up faster in the blood than the liver can conjugate it for excretion from the body.
A normal process that occurs during the transition from intrauterine to extrauterine life in which the immature neonatal liver gradually matures and begins to effectively conjugate bilirubin. It typically appears between 48 and 96 hours after birth and resolves within a few weeks. However, if jaundice is present the first 24 hours after birth, it is considered pathological jaundice.
Occurs when there are abnormally elevated levels of unconjugated and conjugated bilirubin. It may be present within the first 24 hours of life.
Blood group incompatibility which occurs when a mother who is Rh-negative is pregnant with a fetus who is Rh-positive.
Blood group incompatibility in which a mother has Type O blood and the fetus has Type A, B, or AB blood.
Diagnosed when an otherwise healthy baby cries for no apparent reason and they are not easily soothed.
A condition where an infant develops flat spots on the head, often due to repeated pressure on the back of the head.

