12.2 Physical Changes After Birth
This section will discuss fetal circulation and the physiological changes that occur immediately after birth. It may be helpful to begin by reviewing anatomy of the cardiovascular system using the information in the following box. Recall that the pulmonary circuit in children and adults transports blood to and from the lungs, where it picks up oxygen and delivers carbon dioxide for exhalation. However, before birth, the lungs are nonfunctional, and the fetus instead receives oxygen and nutrients from the mother through the umbilical cord.
See the “Review of Anatomy and Physiology of the Cardiovascular System” section of the “Cardiovascular Alterations” chapter in Open RN Health Alterations.
Fetal Circulation and Shunts
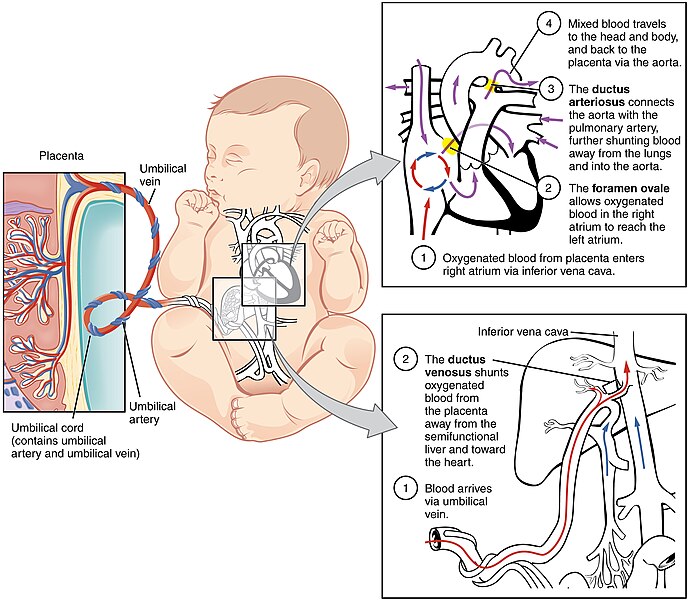
The major differences between fetal circulation and newborn circulation are the sources of oxygen and nutrients. Instead of the lungs providing oxygen and the gastrointestinal system providing nutrients, the fetus receives oxygen and nutrients from the mother’s placenta. Fetal circulation includes shunts, a term for alternative circulatory pathways that allow blood to bypass the lungs and liver until birth, when these organs become functional. These shunts include the ductus venosus, foramen ovale, and ductus arteriosus.
The fetal blood picks up oxygen and nutrients in the mother’s placenta and flows toward the fetal inferior vena cava via the umbilical vein. It mostly bypasses the immature liver via the ductus venosus shunt. The liver is semi-functional and requires a minimal amount of blood for metabolic requirements. From the inferior vena cava, oxygenated blood flows into the right atrium, mixing with deoxygenated venous blood from the superior vena cava.
Because fetal blood is not oxygenated in the lungs, fetal circulation bypasses the lungs by diverting most of the oxygenated blood through the foramen ovale, a shunt that connects the right atria to the left atria and avoids the pulmonary system altogether.
Remaining blood from the right atrium is pumped into the right ventricle and into the pulmonary artery. A shunt within the pulmonary artery called the ductus arteriosus diverts most of this blood into the aorta, which has much less resistance to blood flow than the blood vessels of the fetus’s uninflated lungs. Only a small volume of blood ultimately flows into the immature pulmonary system, which has only minor metabolic requirements.
In the left atrium, partially oxygenated blood flowing from the foramen ovale mixes with deoxygenated blood returning from the pulmonary system. This blood flows into the left ventricle, where it is pumped into the aorta. Mixed blood flows to the fetal head and body. As the blood circulates through the fetal body and returns to the umbilical cord, it collects carbon dioxide and waste products. Two umbilical arteries carry the deoxygenated blood with carbon dioxide and fetal wastes to the placenta, where they diffuse into the maternal circulation. Oxygen and nutrients from the mother diffuse from the placenta into the umbilical vein and the process repeats. See Figure 12.1[1] for an illustration of fetal circulation.
Transition After Birth to Neonatal Circulation
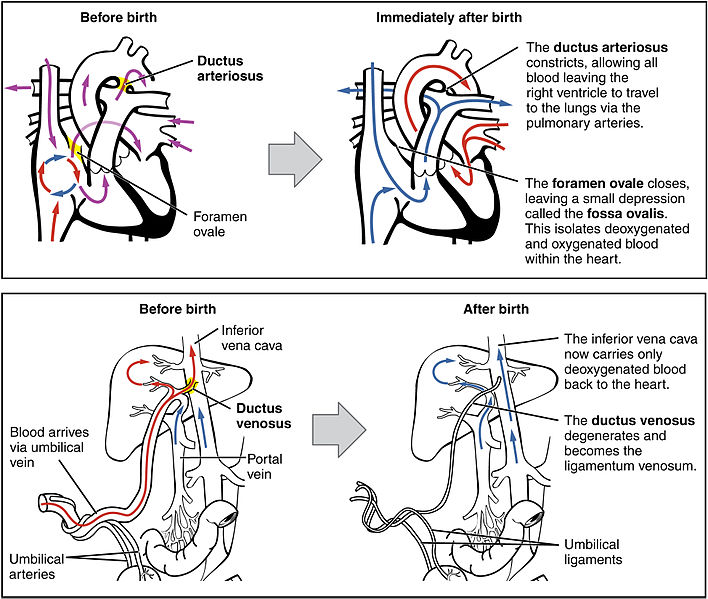
Transition from fetal to neonatal circulation begins immediately after birth. As the umbilical cord is clamped and cut, the neonate becomes responsible for its own cardiopulmonary functioning without the assistance of the placenta.
As the umbilical cord is cut, systemic vascular resistance increases, and the foramen ovale begins to close within minutes of birth. The ductus venosus begins to narrow and close in the first few days of life due to lack of blood flow and pressure from the umbilical vein. Permanent closure is completed within one to three months.[2]
With the first breath, the neonate’s lungs expand, allowing for increased capacity and release of surfactant, which decreases tension within the lungs. Fluid within the lungs is reduced as a result of the pressure change that occurs during the lung’s expansion and filling with air. Expansion of the lungs also causes a drop in pulmonary artery pressure, resulting in increased blood flow into the pulmonary circulation and decreased blood flow through the ductus arteriosus. The ductus arteriosus constricts and closes within 12 to 24 hours after birth. Permanent closure of the ductus arteriosus occurs within two to three weeks of birth. See Figure 12.2[3] for an illustration of the transition of circulation before birth to immediately after birth.
Impaired Transition and Neonatal Resuscitation
While the transition from fetal circulation to neonatal circulation is a natural process, it does not always happen smoothly. Neonatal resuscitation is initiated for infants who are struggling to transition from fetal to neonatal circulation. Nearly 10% of neonates will experience impaired transition, which will require some intervention, with less than 1% requiring extensive resuscitation efforts at birth.[4]
Impaired transition due to absent or minimal respiratory effort may be caused by birth asphyxia that can occur when the neonate does not receive enough oxygen before, during, or immediately after it is born. This lack of oxygen can be a result of umbilical cord prolapse; compression of the umbilical cord; uterine rupture; placenta abruption; or a prolonged, difficult labor. Other conditions can also cause impaired transition, such as congenital lung disorders, diaphragmatic hernia, Group B Streptococcal pneumonia, congenital heart disease, or prematurity.[5]
Read additional information about signs of fetal distress and related nursing interventions in the “Fetal Heart Rate Monitoring” section of the “Labor & Delivery Care” chapter.
When a neonate experiences cardiac arrest or respiratory distress at birth, Neonatal Resuscitation Program (NRP) guidelines are followed by the health care team. The most important priority for newborn survival is the establishment of adequate lung inflation and ventilation after birth. Newborn resuscitation requires anticipation and preparation by health care professionals who train individually and as teams. NRP guidelines include the following[6],[7]:
- Warmth: Place the infant on a radiant warmer
- Airway: Adjust airway and remove secretions if necessary
- Breathing: Start supplementary oxygen if SpO2 remains below 90%
- Circulation: Begin chest compressions if heart rate is below 60 beats per minute
- Intubation: Perform intubation if required
- Medication: Administer epinephrine if necessary
- “2916_Fetal_Circulatory_System-02.jpg” by OpenStax College is licensed under CC BY 3.0 ↵
- Sidhu, P. S. (2023). Embryology, ductus venosus. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK547759/ ↵
- “2921_Neonatal_Circulatory_System.jpg” by OpenStax College is licensed under CC BY 3.0 ↵
- Ferschl, M. B. (2023). Fetal circulation, transition at birth, and persistent fetal circulation. OpenAnesthesia. https://www.openanesthesia.org/keywords/fetal-circulation-transition-at-birth-and-persistent-fetal-circulation/ ↵
- Ferschl, M. B. (2023). Fetal circulation, transition at birth, and persistent fetal circulation. OpenAnesthesia. https://www.openanesthesia.org/keywords/fetal-circulation-transition-at-birth-and-persistent-fetal-circulation/ ↵
- Jogie, J. A. (2023). A case report on successful resuscitation of a two-month-old infant in the emergency room: Neonatal resuscitation program (NRP) guidelines in practice. Cureus, 15(4). https://doi.org/10.7759/cureus.38291 ↵
- American Heart Association. (n.d.). Neonatal resuscitation. https://cpr.heart.org/en/resuscitation-science/cpr-and-ecc-guidelines/neonatal-resuscitation ↵
A term for alternative circulatory pathways that allow blood to bypass the lungs and liver until birth.
The umbilical vein is a blood vessel in the umbilical cord that carries oxygenated blood and nutrients from the placenta to the fetus.
A shunt that carries oxygenated blood from the umbilical vein to the right atrium of the heart in a fetus, bypassing the liver.
A shunt that connects the right atria to the left atria and avoids the pulmonary system altogether.
A shunt within the pulmonary artery which diverts blood into the aorta.

