10.5 Fetal Heart Rate Monitoring
During labor, the nurse continually monitors the fetal heart rate for signs of well-being to help ensure a safe delivery. Fetal assessment involves evaluating the fetal heart rate (FHR) in response to uterine contractions (UC) by using intermittent monitoring or continuous electronic fetal monitoring. Nurses working on maternity care units are trained to read FHR tracings and can obtain certification in fetal monitoring. This section describes external and internal fetal monitoring, FHR patterns, and recognizing the need for intervention when FHR tracings indicate possible fetal hypoxia.[1]
Internal and External Monitoring
There are three methods of monitoring the fetal heart rate and uterine contractions. The first method is called intermittent auscultation. The other two methods provide the health care team with continuous data on the fetal heart rate and uterine contractions and are called external monitoring and internal monitoring.
Intermittent Auscultation
Intermittent auscultation (IA) refers to a technique of listening to and counting the fetal heart rate for a specific amount of time during specified intervals throughout labor to assess fetal well-being. This technique includes palpating the uterus to evaluate the duration, intensity, and frequency of contractions and then listening to the fetal heart rate before, during, and after the uterine contraction to evaluate for changes. IA may be performed with a fetoscope or a Doppler monitor. A fetoscope is similar to a stethoscope but uses bone conduction to better detect FHR. A fetoscope can be used after 20 weeks’ gestation to detect FHR. A Doppler monitor is a handheld device that uses ultrasonic waves to detect FHR. Doppler monitors are used to auscultate FHR during antepartum visits, as well as during labor. When auscultating the FHR using a Doppler monitor, it is important to also assess the maternal heart rate to ensure the Doppler is detecting fetal heart rate and not maternal heart rate.
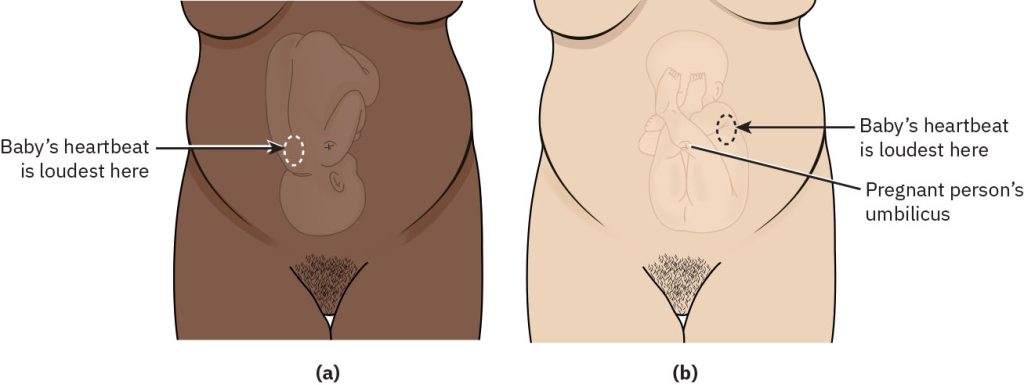
Leopold’s maneuvers are performed prior to IA to identify the fetal position for optimal placement of the fetoscope or transducer of the Doppler monitor. After the fetal spine is located, the fetoscope or transducer is placed on the mother’s abdomen directly over the fetal spine where the fetal heart is the loudest. See Figure 10.18[2] for an illustration of optimal positions for listening to the FHR in vertex and breech presentations.
Review how to perform Leopold’s maneuvers in the “Third Trimester Prenatal Care” section of the “Antepartum Care” chapter.
One advantage of IA is the freedom of movement by the client during labor. Movement helps the fetus descend into the pelvis and is also a nonpharmacological pain intervention for the laboring client. Because IA does not require attached monitors, the laboring client can walk, shower, sit on a birthing ball, or take a bath. The absence of monitors strapped onto the abdomen can also facilitate rest between contractions. A disadvantage of IA is the lack of FHR tracings that provide a visual history of the uterine contractions and FHR. These tracings are used during communication with the health care provider and provide a permanent record of labor, both of which are not possible with IA because there are no tracings recorded.[3]
Continuous External Monitoring
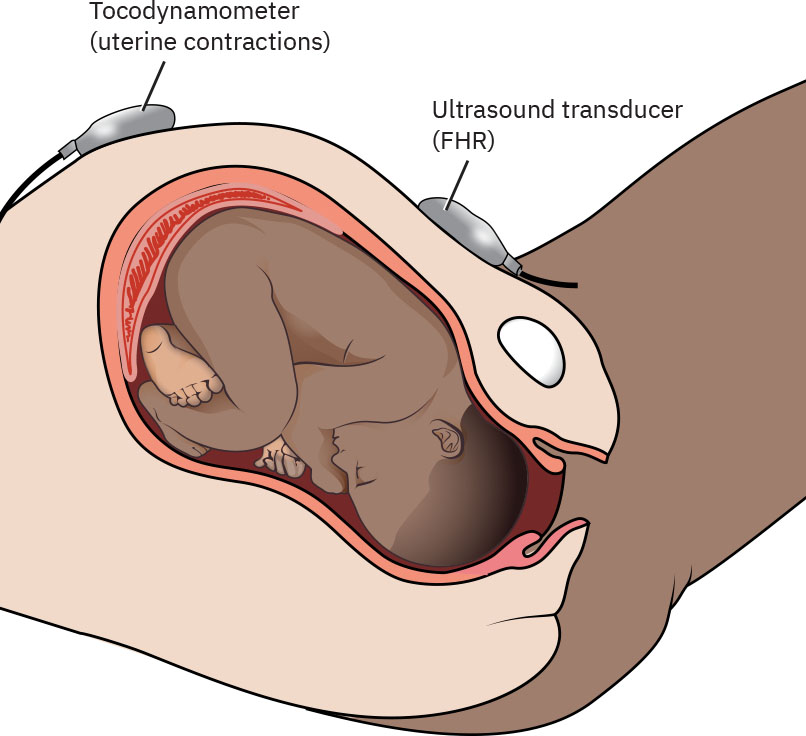
The most common method of monitoring FHR and uterine contraction patterns is through continuous external monitoring. Continuous external monitoring requires the use of two monitoring devices, including an ultrasound transducer to evaluate the fetal heart rate and a tocodynamometer (toco) to detect the frequency of uterine contractions.[4]
The nurse applies these external monitors to the client’s abdomen and they are held in place with belts or adhesives. The nurse identifies the optimal placement of these devices using Leopold’s maneuvers as previously described under IA. The ultrasound transducer is placed on the maternal abdomen over the fetal back and close to the fetal head, where the FHR is usually the loudest. The toco transducer is placed on the maternal abdomen where the fundus is firmest, typically over the fetal buttocks if the fetus is in a cephalic presentation. See Figure 10.19[5] for an illustration of the placement of these transducers for external monitoring. Both external monitors are connected to a monitor, and their signals are traced onto graph paper.
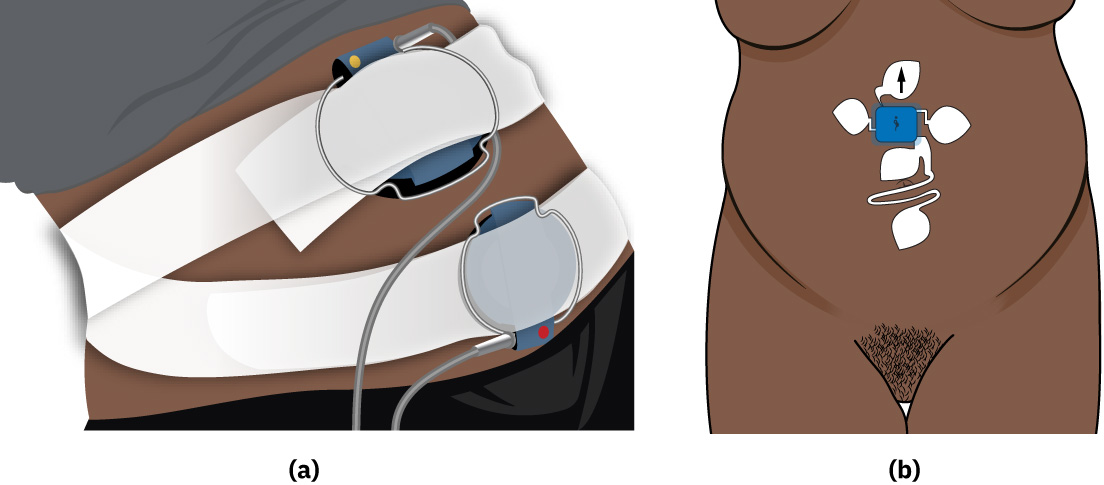
See Figure 10.20[6] for an illustration of a continuous external fetal monitor compared to a wireless fetal monitoring system. Wireless monitors provide continuous monitoring but also allow clients to ambulate. Some wireless monitors are waterproof and allow for continuous monitoring during hydrotherapy and water birth.
The advantages of external fetal monitoring are its ease of use, the ability to digitally store the results, and the opportunity for advanced fetal assessment. Digital monitoring also allows nursing staff and health care providers to assess the fetal monitor tracing from anywhere, including the maternal care unit, the health care provider’s office, or the health care provider’s home.[7]
Disadvantages of continuous external monitoring is that the placement of the transducers can shift when the person changes positions or gets out of bed, resulting in a lost signal. Continuous monitoring can also limit the client’s freedom to walk, shower, or bathe if wireless monitoring is not available. Additionally, the tocodynamometer can accurately measure the frequency and duration of contractions, but not necessarily the accurate intensity of the contractions.[8]
Continuous Internal Monitoring
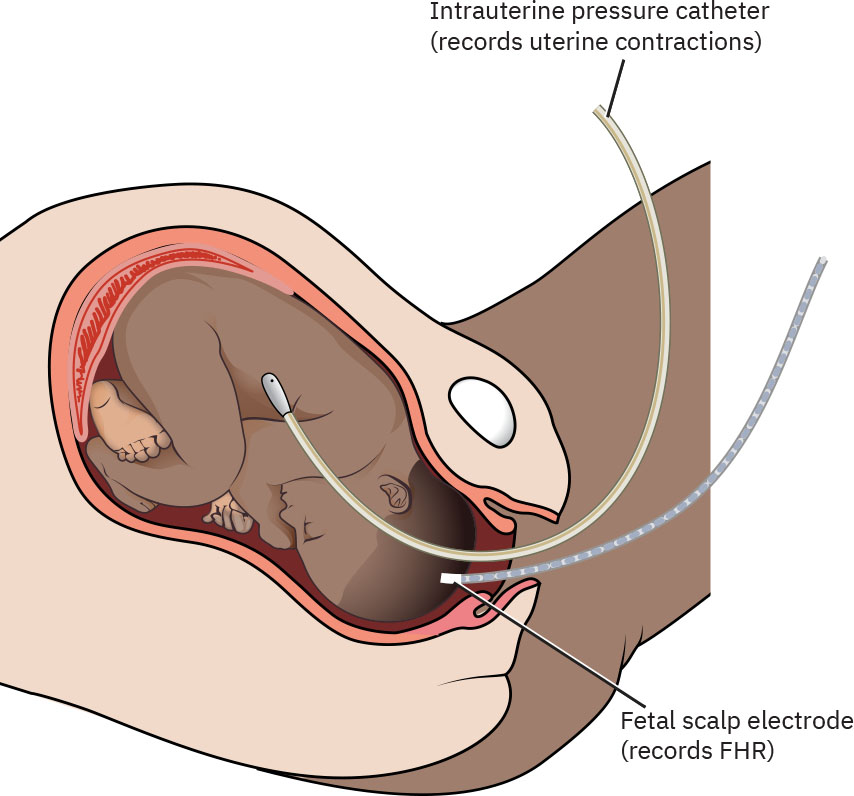
Internal fetal monitoring consists of two devices called a fetal scalp electrode and an intrauterine pressure catheter. The fetal scalp electrode affixes to the scalp of the fetus and monitors the fetal heart rate. The intrauterine pressure catheter is placed inside the uterus and measures the duration, intensity, and frequency of uterine contractions, as well as the resting tone of the uterus. Internal monitors are used in client situations that require more in-depth fetal surveillance, such as nonreassuring fetal heart rates, decreased amniotic fluid, or during labor induction or augmentation with oxytocin. See Figure 10.21[9] for an illustration of continuous internal monitoring.
Continuous internal monitors are placed by health care providers and specially trained labor and delivery nurses. First, a vaginal exam is performed to assess cervical dilation and membrane status. The cervix must be dilated, and the amniotic membrane must be ruptured to place the monitors in the uterus. If the amniotic sac is intact, the health care provider weighs the risks and benefits of rupturing the amniotic membrane and when appropriate, artificially breaks the bag of amniotic fluid using an amniotomy hook.
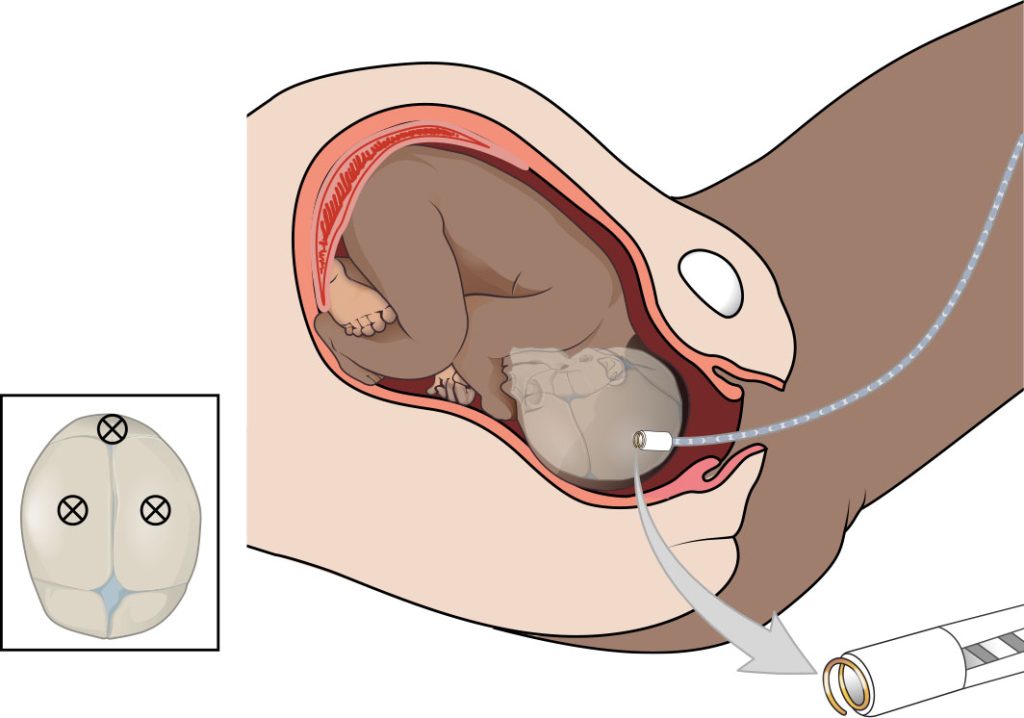
To place the fetal scalp electrode, the fetal head must be low enough to be palpated during the vaginal exam, and the cervix must be open. The fetal head is assessed to identify suture lines and fontanelles. Avoiding the fontanelles, the scalp electrode is placed firmly over bone on the fetal scalp and turned clockwise to adhere the electrode. Then, the scalp electrode transducer is connected to the monitor.[10] See Figure 10.22[11] for an illustration of placement of the fetal scalp electrode.
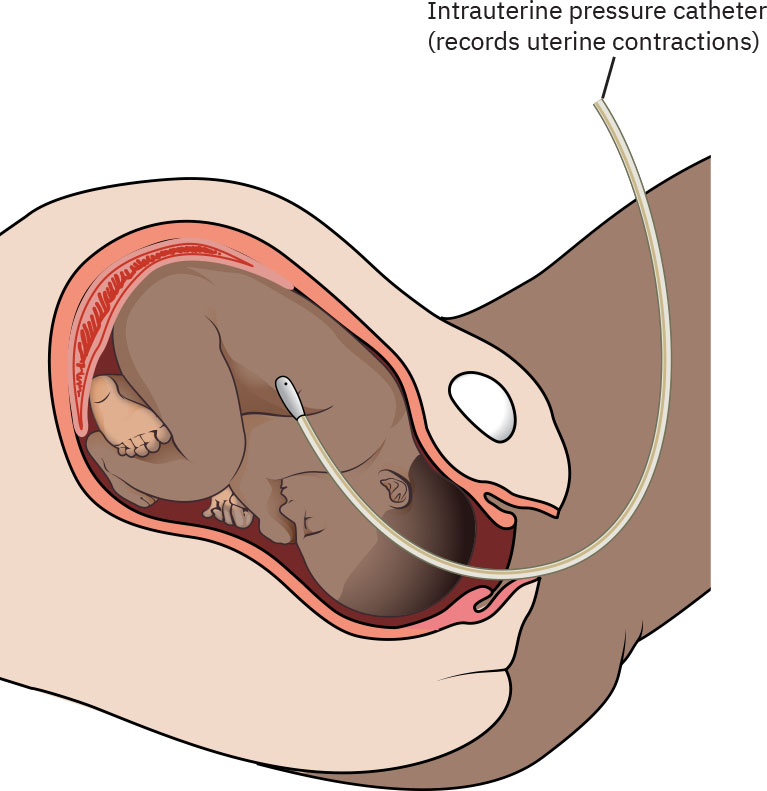
The intrauterine pressure catheter (IUPC) is inserted using a firm plastic introducer containing the pressure catheter. It is placed between the walls of the uterus and the fetus. The catheter has markers to guide the depth of placement to avoid uterine perforation. To avoid the IUPC being inserted through the placenta, the introducer is retracted immediately if frank red blood is noted. The pressure catheter transducer is attached to a monitor and measures in millimeters of mercury (mmHg) the strength of the contractions, as well as the uterine resting tone. See Figure 10.23[12] for an illustration of placement of the IUPC.
Continuous internal monitoring is used during client situations that require comprehensive and continuous evaluation of fetal well-being and uterine contractions. The fetal scalp electrode is the most precise way to monitor the fetal heart rate because it receives signals directly from the fetus and transmits them to the monitor tracing. In situations of FHR decelerations, the internal monitor provides exact timing of the FHR deceleration in relation to the strength of contraction. The scalp electrode also allows the nurse to evaluate variability more precisely. This information is helpful in determining nursing interventions to resolve FHR decelerations. In situations where labor is not progressing as expected, the IUPC is used to detect the strength of contractions, and this data is used to manage the administration of oxytocin.[13]
The disadvantages of internal continuous monitoring include increased risk of infection due to the required rupture of membranes and the break in fetal skin integrity during placement of the fetal scalp electrode. There is also a risk of puncturing the uterus and placenta during placement of the IUPC.[14]
Fetal Assessment
When a fetal monitor is used for continuous monitoring, the nurse monitors fetal heart rate baseline, variability, and the presence of periodic accelerations or decelerations that indicate signs of fetal distress. Fetal heart rate patterns are evaluated in association with the overall clinical picture of the laboring client and other signs of fetal well-being. If nonreassuring fetal heart rate patterns are observed, the nurse implements nursing interventions and promptly notifies the health care provider to ensure the safety of the mother and the baby.
Three principles of client safety offer a uniform interpretation of FHR tracings[15]:
- Principle 1: Variable, late, or prolonged FHR decelerations demonstrate interruption of the transfer of oxygen from the environment to the fetus at one or more points.
- Principle 2: Moderate variability and/or FHR accelerations indicate fetal well-being and the absence of fetal metabolic acidosis.
- Principle 3: Neurologic injury to the fetus can occur if fetal hypoxia causes significant fetal metabolic acidosis (i.e., umbilical artery pH < 7.0 and base deficit > 12 mmol/L).
Several terms related to fetal heart rate monitoring are discussed in the following subsections.
Review the basic components of fetal monitoring in the “Power” subsection of “The P’s of Labor” section.
Fetal Heart Rate Baseline
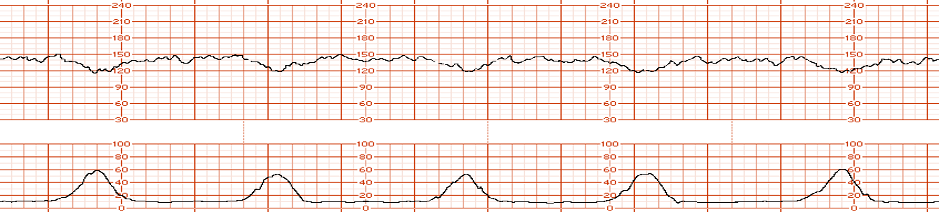
The top half of a FHR tracing indicates FHR, and the bottom half indicates uterine contractions. Figure 10.24[16] shows an FHR tracing on graph paper. Each small box is 10 seconds, and the darker red vertical lines indicate 60 seconds.
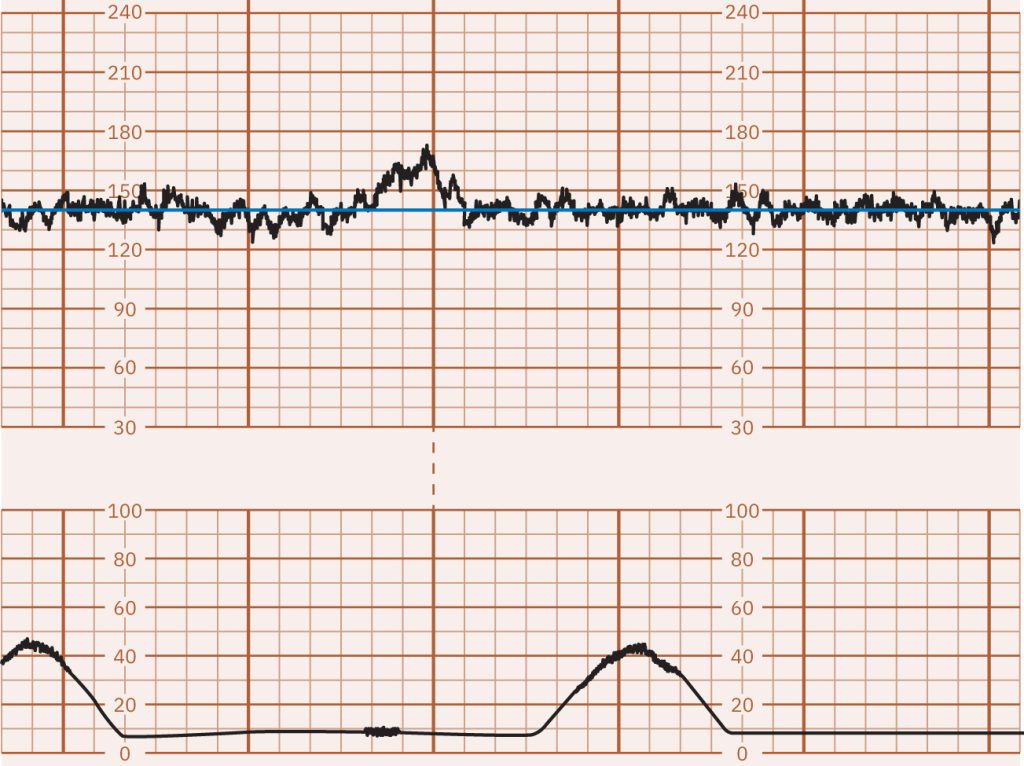
The fetal heart rate baseline is the average beats per minute in a ten-minute segment, excluding periodic changes or marked variability. A normal FHR baseline ranges from 110 to 160 bpm and is documented in increments of five beats per minute (bpm). See Figure 10.25[17] for an illustration of a FHR baseline of 150 bpm as indicated by the blue line. The FHR baseline is controlled by the fetal sympathetic and parasympathetic nervous systems. The sympathetic nervous system increases the FHR, while the parasympathetic nervous system decreases the FHR. Complications such as fetal hypoxia and hypercapnia activate chemoreceptors that impact the FHR.
Fetal Tachycardia
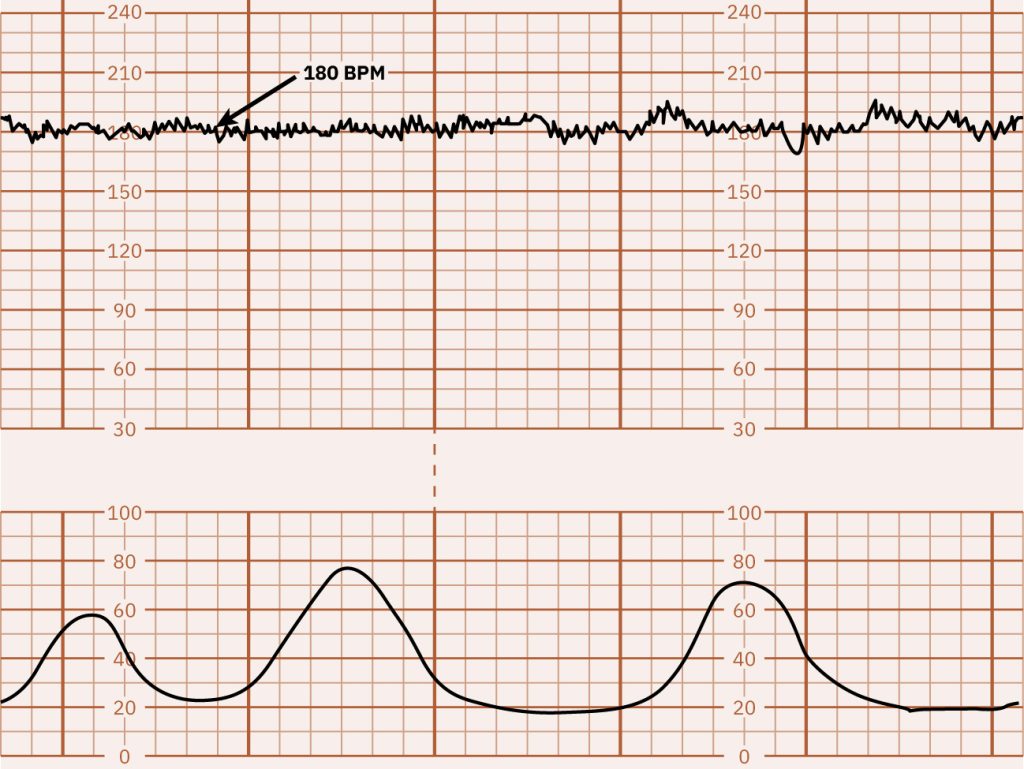
A sustained FHR baseline greater than 160 bpm for ten minutes is classified as fetal tachycardia. Figure 10.26[18] for an illustration of fetal tachycardia of 180 bpm. Fetal tachycardia can be caused by multiple factors but is not considered a sign of fetal distress in the absence of FHR decelerations.[19] Factors that cause fetal tachycardia and associated nursing interventions are discussed in the following subsection.
Nursing Interventions
Interventions for fetal tachycardia are based on the cause. The most common cause of fetal tachycardia is maternal fever. If the client has a temperature greater than 100.4° F (38° C), the nurse should notify the health care provider for anticipated prescriptions of antibiotics and antipyretics. However, the nurse is aware that epidural anesthesia can cause a minimal rise in maternal temperature due to inflammatory responses and/or effects on the thermoregulatory system, causing shivering that, in turn, causes elevated temperature.[20]
Maternal dehydration can also cause fetal tachycardia. If dehydration is apparent, the nurse encourages oral intake of fluid or notifies the health care provider for anticipated prescription of intravenous fluids.[21]
Additionally, a maternal history of anemia or hyperthyroidism can cause fetal tachycardia. The nurse reviews the client’s prenatal history to determine if anemia or hyperthyroidism were noted during prenatal care.[22]
Fetal tachycardia can also be caused by fetal stress (especially during prolonged labor), infection, hypoxia, or prolonged stimulation by oxytocin. If oxytocin is being administered, discontinuation of the oxytocin infusion may be indicated. The nurse should notify the health care provider and receive orders for further management.
Fetal Bradycardia
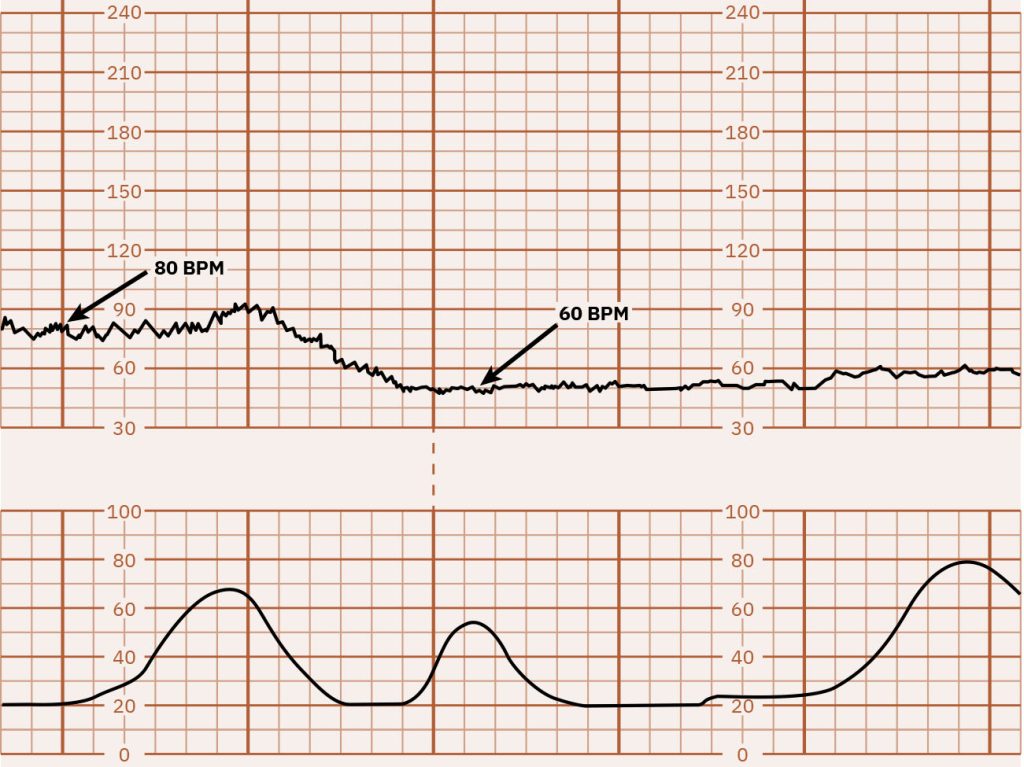
Fetal bradycardia is defined as an FHR baseline less than 110 beats for ten minutes. See Figure 10.27[23] for an illustration of fetal bradycardia. Fetal bradycardia can be caused by multiple factors such as fetal hypoxia, umbilical cord compression, maternal hypotension or hypoglycemia, or side effects of medications like magnesium sulfate. The nurse must determine if the decreased FHR is a benign episode of bradycardia or a pathologic prolonged deceleration requiring further intervention and prompt notification of the health care provider.[24]
Nursing Interventions
The nurse tailors interventions to treat the cause of fetal bradycardia. The first nursing intervention is to reposition the laboring client on their left side to facilitate blood flow to the placenta.[25]
The cause of bradycardia may be evident on vaginal examination, such as a prolapsed umbilical cord resulting in umbilical cord compression. Umbilical cord prolapse occurs when the umbilical cord leaves the cervical os before the fetal presenting part and, as a result, gets compressed by the fetal presenting part. A prolapsed umbilical cord is considered a medical emergency, and the priority intervention is to relieve pressure on the cord until delivery via cesarean section is possible because cord compression results in hypoxia to the fetus. Relieving cord compression is done by inserting two fingers into the client’s vagina, taking care to avoid further compression of the umbilical cord, locating the presenting fetal part, and elevating the presenting part away from the umbilical cord. This action can resolve the cord compression and allow return of oxygenated blood flow to the fetus, helping to prevent anoxic brain injuries in the fetus. It is important to remember that manual cord decompression must be maintained until the fetus is delivered to reduce the risk of complications related to hypoxia, including encephalopathy, cerebral palsy, or fetal death.[26],[27]
Uterine tachysystole is defined as excessive uterine contractions, typically with more than five contractions in ten minutes occurring in at least two consecutive intervals. Uterine tachysystole can also cause fetal bradycardia because the lack of time for fetal recovery between contractions uses up the fetal reserve of oxygen. Resulting fetal hypoxia causes fetal bradycardia. If oxytocin is being administered, the health care provider may discontinue administration and prescribe a tocolytic medication (i.e., medications used to relax the uterus, such as terbutaline) to facilitate placental blood flow to the fetus.[28]
Placental abruption and uterine rupture are serious complications that can cause concealed hemorrhage resulting in fetal bradycardia. These conditions are both medical emergencies and require immediate delivery via cesarean birth, as well as life sustaining interventions to manage hemorrhage in the mother.
FHR Variability
Nurses and health care providers assess FHR variability and consider it, along with other factors, to assess fetal well-being. FHR variability refers to the beat-to-beat fluctuations in the FHR baseline caused by stimulation of the fetal sympathetic and parasympathetic nervous systems. Variability is classified as moderate, minimal, absent, marked, or sinusoidal. Moderate variability indicates a healthy fetus but minimal, absent, or marked variability can indicate fetal hypoxia.[29]
Potential pharmacologic causes of decreased variability include opioids, corticosteroids, and magnesium sulfate. Maternal ingestion of cocaine can also decrease FHR variability. These causes are transient and will resolve once the medication is excreted.[30]
Moderate FHR Variability
Moderate FHR variability is considered normal and indicates fluctuations in FHR between 6 and 25 bpm above or below baseline. Clear and frequent fluctuations indicate a healthy fetus that is well-oxygenated with a normal acid-base balance and a well-functioning nervous system. See Figure 10.28[31] for an illustration of moderate FHR variability.
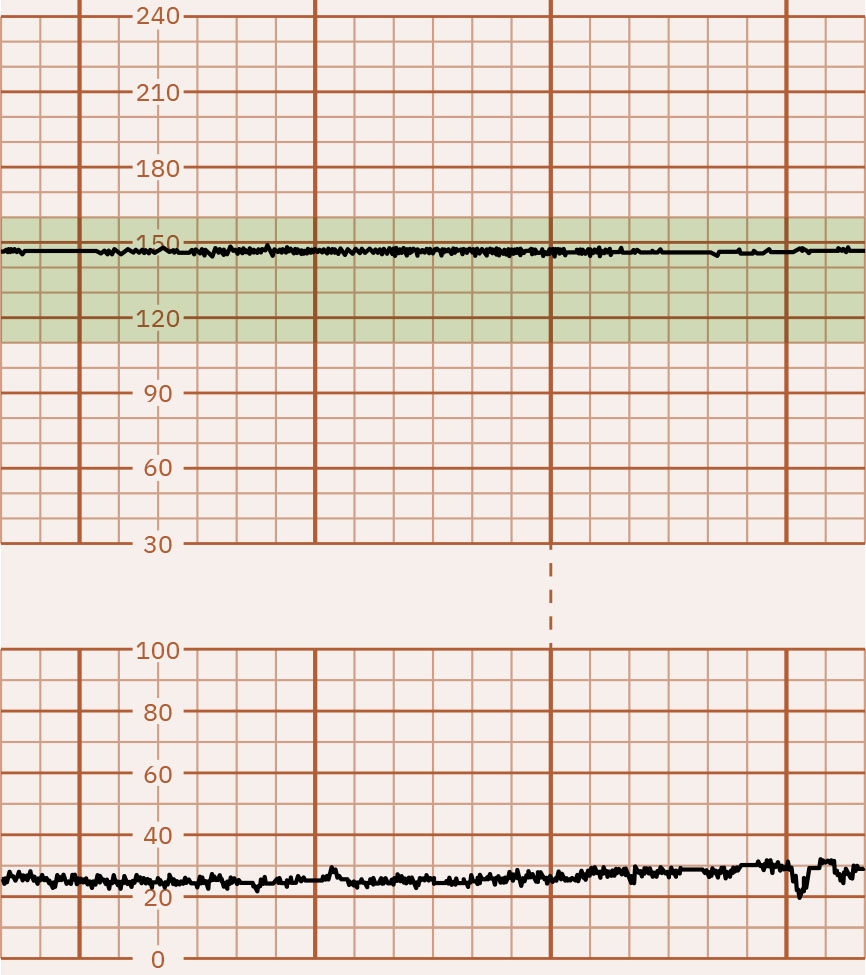
Minimal FHR Variability
Minimal FHR variability means the fetal heart rate shows slight fluctuations of 5 bpm or less. Minimal variability can be caused by many factors, such as fetal sleep cycles, preterm gestation, side effects of medications such as magnesium sulfate, or fetal acidemia (low blood pH). While minimal FHR variability may not be alarming on its own, it indicates closer monitoring is required by the nurse. See Figure 10.29[32] for an illustration of minimal FHR variability.
Absent FHR Variability
Absent FHR variability means the fetal heart rate shows very little or no fluctuation and appears flat or nearly flat. Maternal acidosis or fetal metabolic acidosis due to poor oxygenation can also cause absent FHR variability. Absent variability is concerning and must be promptly reported to the health care provider for additional assessment and intervention. See Figure 10.30[33] for an illustration of absent FHR variability.[34]
Marked FHR Variability
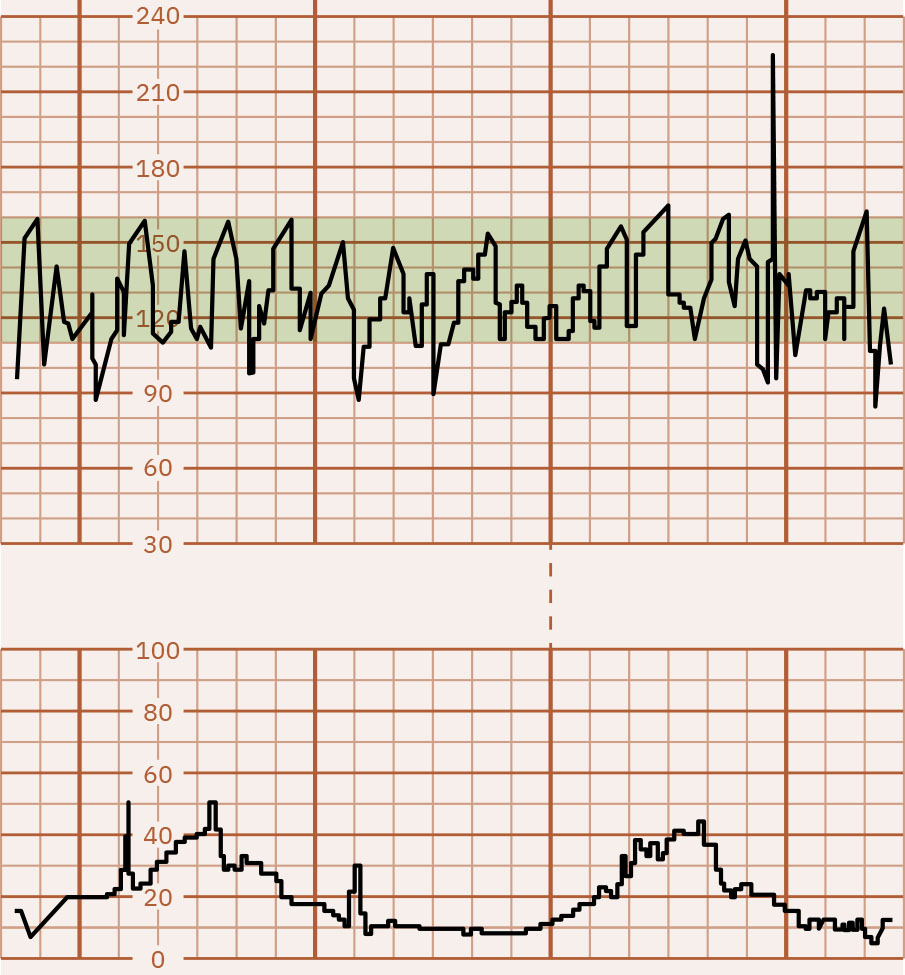
Marked FHR variability indicates the fetal heart rate varies significantly from beat to beat with frequent fluctuations in the fetal heart rate greater than 25 bpm. Because of the extreme fluctuations, the FHR baseline is undeterminable. Marked FHR variability is rare. The most common time for marked variability is during the two hours prior to delivery after an event of decreased fetal oxygenation, such as cord compression or a maternal seizure. It is associated with an increased risk for neonatal respiratory distress after birth. If cord compression is present, the nurse relieves the cord compression, administers oxygen, notifies the health care provider immediately, and anticipates the need for an emergent cesarean section delivery. If a maternal seizure occurs, the nurse administers oxygen after the seizure. Marked FHR variability requires further assessment to determine the cause, as well as prompt notification of the health care provider. See Figure 10.31[35] for an illustration of marked FHR variability.
Sinusoidal Pattern
A sinusoidal FHR pattern refers to a wavelike pattern with regular frequency (three to five per minute) and amplitude. However, the wavelike pattern is not FHR variability, and FHR variability is actually absent although the FHR is usually within normal range. Sinusoidal pattern is linked with fetal compromise, acidemia, and morbidity. It may be caused by side effects of medications administered to the mother (such as butorphanol), sepsis, or from severe fetal anemia due to loss of blood. Fetal anemia may occur due to bleeding resulting from blood sampling through the fetal scalp or cord, a hemolytic blood reaction in the fetus as a result of Rh incompatibility, fetomaternal transfusion, or from maternal-fetal hemorrhage during placental abruption.[36] See Figure 10.32[37] for an illustration of a sinusoidal FHR pattern.
Periodic Changes in the Fetal Heart Rate
Accelerations and decelerations of the FHR in relation to the FHR baseline are considered periodic changes in the FHR. Periodic changes in FHR are described as abrupt or gradual.[38]
Temporary FHR Acceleration
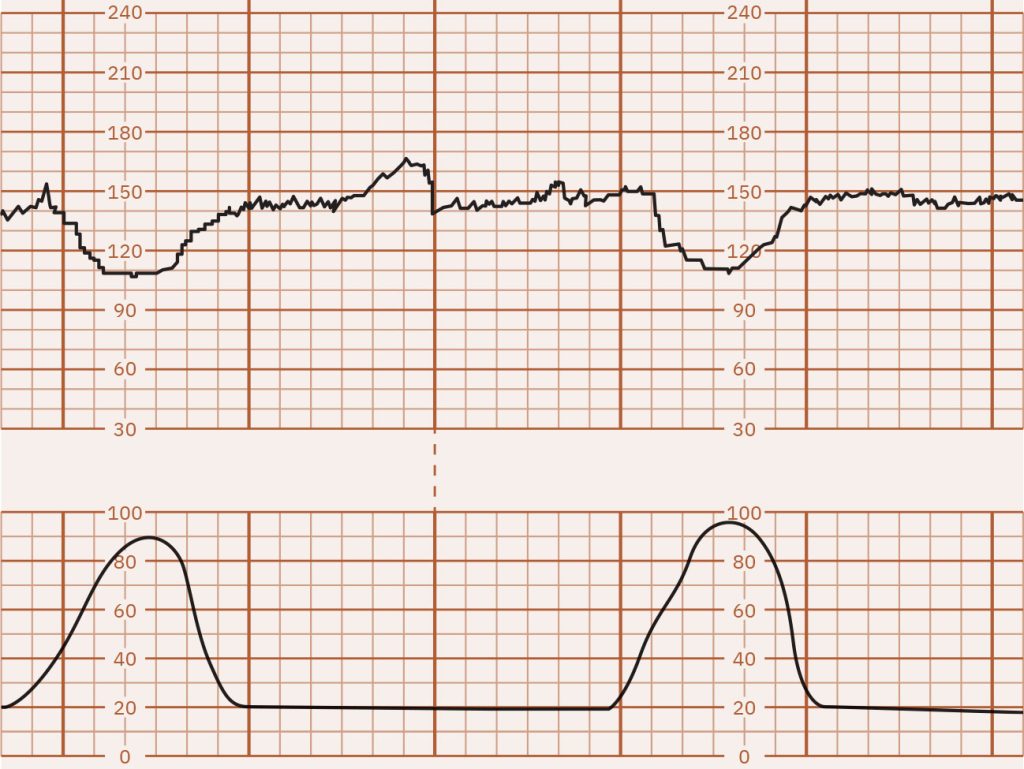
Abrupt but temporary increases in the FHR above the baseline with an onset-to-peak of less than 30 seconds are called accelerations. Accelerations are typically associated with fetal movement and occur independently from uterine contractions. They are identified by an FHR peak of at least 15 bpm above the baseline, with a duration of at least 15 seconds but less than two minutes. Accelerations are a reassuring indication of fetal well-being. See Figure 10.33[39] for an illustration of a periodic FHR acceleration of 120 bpm to 160 bpm lasting about 30 seconds. Note that the acceleration in this illustration is not related to the uterine contraction.[40]
Decelerations
Decelerations are intermittent decreases in the FHR below baseline, classified as early, late, variable, and prolonged. Decelerations can be associated with fetal hypoxia and require additional assessment, nursing interventions, and notification of the health care provider.
Early Decelerations
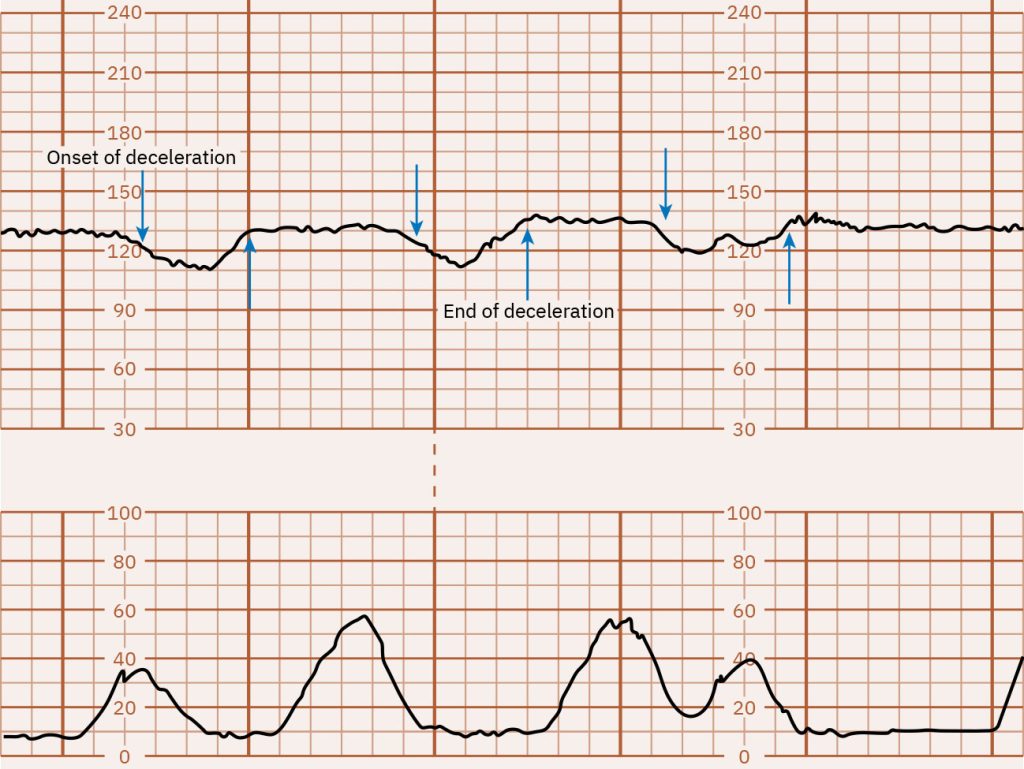
A gradual, uniform decrease in FHR that returns to baseline and mirrors the uterine contraction is called early deceleration. Early decelerations are commonly seen during active labor as the fetal head descends into the maternal pelvis, causing compression of the fetal head that activates the fetal vagal nerve and causes decreased FHR. The degree of deceleration is proportional to the strength of the uterine contraction causing fetal head compression.[41] See Figure 10.34[42] for an illustration of early FHR decelerations that mirror the uterine contraction.
Late Decelerations
Decelerations in the FHR below the baseline that start during a uterine contraction and continue after completion of the contraction are called late decelerations. During a uterine contraction, the decrease in oxygen delivered to the fetus causes a decreased FHR that begins late in the contraction. The nadir, or lowest point, of the deceleration occurs after the peak of the contraction. Late decelerations are typically repetitive and form a pattern in association with uterine contractions.[43] See Figure 10.35[44] for an illustration of late decelerations where the FHR decreases during the contraction and does not return to baseline until after the contraction ends.
Late decelerations are nonreassuring and indicate fetal hypoxia. Late decelerations can be caused by several conditions. One condition is uteroplacental insufficiency, which is a lack of oxygenated blood coming from the uterus to the placenta, and, therefore, to the fetus. Another common cause of late decelerations is tachysystole, where contractions occur too frequently or last longer than two minutes. Tachysystole is often caused by the administration of oxytocin and can result in lack of blood flow and subsequent hypoxia to the fetus. Spinal or epidural anesthesia can also cause maternal hypotension, resulting in hypoperfusion of the placenta. Other causes of late decelerations are maternal hypertension, anemia, and placental abruption.[45]
Variable Decelerations
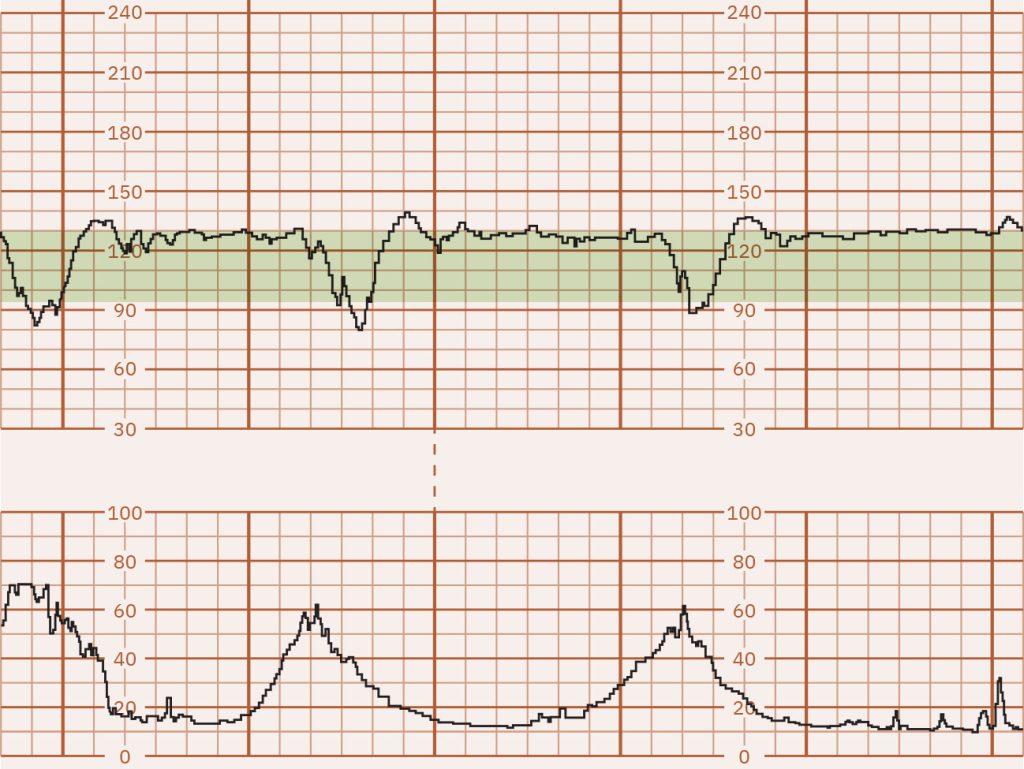
Abrupt decelerations of FHR of at least 15 bpm below the baseline that last at least 15 to 30 seconds are called variable decelerations. Variable decelerations may appear as a “V” or “W” shape on the tracing due to their abruptness and may or may not appear in a pattern. Variable decelerations are caused by temporary compression of the umbilical cord. Compression of the umbilical cord can occur if a fetal body part squeezes the cord against the wall of the uterus, the cord is squeezed by a uterine contraction, or the cord is squeezed by the mother assuming a specific position. Variable decelerations may lead to fetal hypoxia, especially if they are repetitive over a prolonged period.[46] See Figure 10.36[47] for an illustration of variable decelerations associated with uterine contractions that appear as a “V” or “W” shape.
Prolonged Decelerations
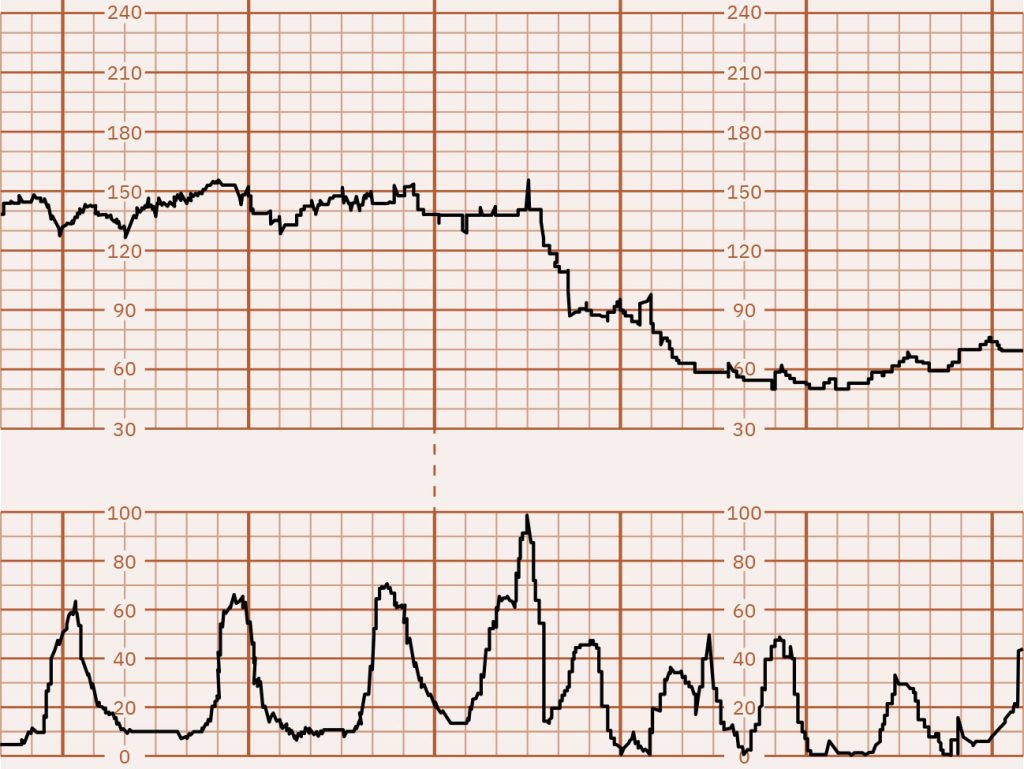
Isolated, sporadic decelerations of at least 15 bpm from the FHR baseline that last two to ten minutes from onset to return to baseline are called prolonged decelerations. Prolonged decelerations are concerning due to their risk of fetal hypoxia. The extent of fetal hypoxia relates to the depth and duration of the deceleration; the deeper and longer the deceleration, the greater the risk of fetal hypoxia. After the prolonged deceleration returns to the FHR baseline, signs of significant fetal hypoxia include fetal tachycardia and/or decreased FHR variability. Prolonged decelerations can be caused by tachysystole, cord compression, maternal hypotension, placental abruption, seizure, or impending birth.[48] See Figure 10.37[49] for an illustration of prolonged deceleration to an FHR of less than 60 bpm caused by tachysystole (too frequent contractions).
Nursing Interventions for Decelerations
Examples of nursing interventions for different types of decelerations are summarized in Table 10.5a.
Table 10.5a. Nursing Interventions for Different Types of Decelerations[50]
| Type of Deceleration | Cause | Intervention |
|---|---|---|
| Early |
|
|
| Late |
|
|
| Variable |
|
|
| Prolonged |
|
|
Uterine Activity
Adequate uterine contractions during labor is defined as five contractions or fewer in a ten-minute period. Expected contraction length is between 45 and 60 seconds and may increase to 90 seconds closer to the onset of the second stage of labor. Abnormal uterine activity called uterine tachysystole refers to more than five uterine contractions in ten minutes or a contraction length of two or more minutes within a 30-minute period. Uterine tachysystole causes diminished placental perfusion because there is diminished blood flow to the placenta while the uterus is contracting. Diminished placental perfusion can cause fetal hypoxia. The nurse evaluates fetal well-being during labor by assessing and documenting the fetal heart rate, uterine activity, and fetal response to the uterine activity.[51]
Fetal Heart Rate Classification System
A classification system is used to interpret fetal heart rate patterns and allows for consistent terminology and management by nurses and health care providers. The system includes three categories based on specific patterns observed in the fetal heart rate to assess the well-being of the fetus during labor.[52],[53] A summary of the three categories is found in Table 10.5b.
Table 10.5b. Fetal Heart Rate Pattern Classification System[54]
| Category | Description |
|---|---|
| Category I | FHR racing includes all of the following:
|
| Category II | FHR tracing includes any of the following:
All tracingings not applicable to Category I or III |
| Category III | FHR tracing includes:
|
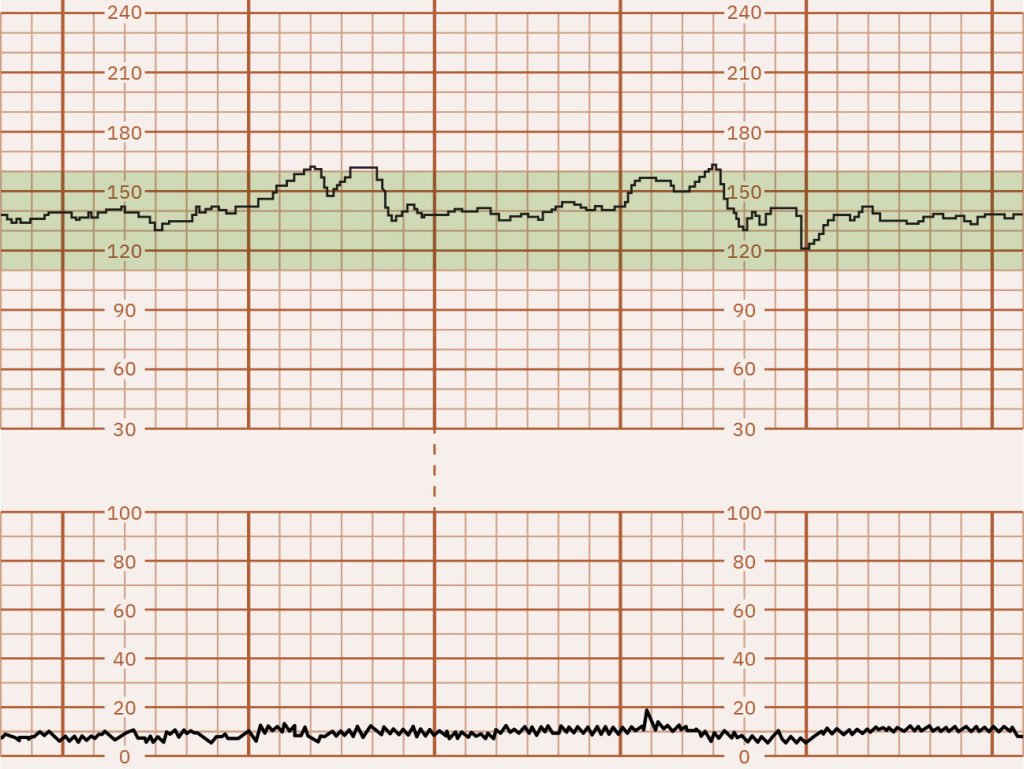
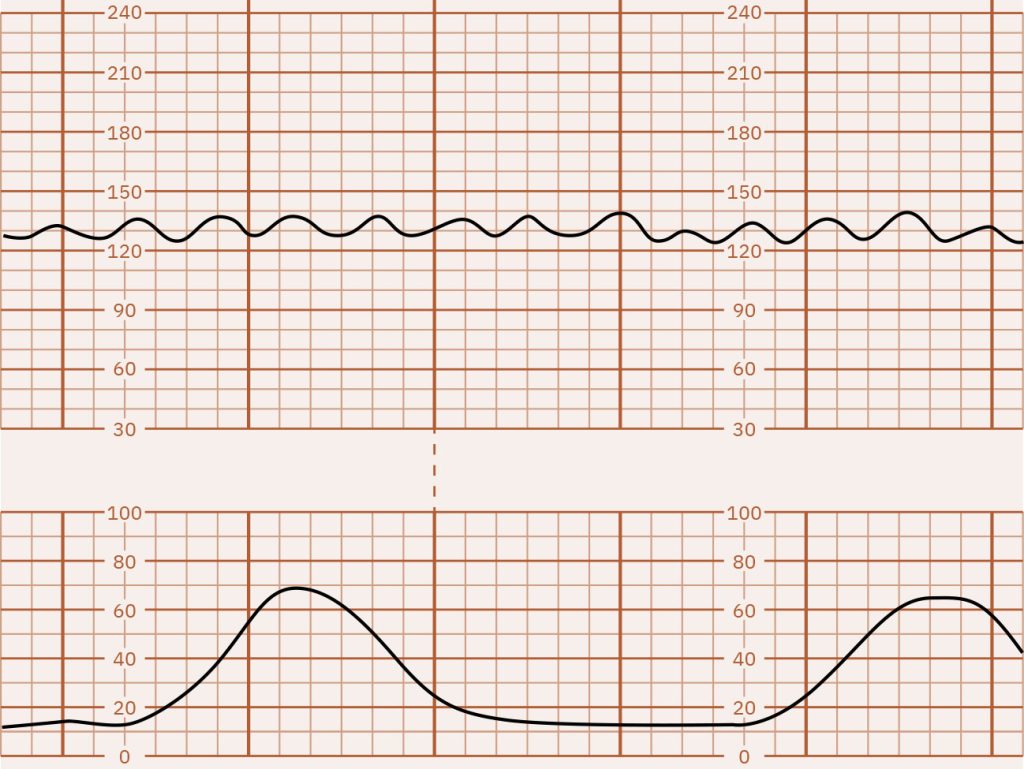
Category I represents normal and reassuring fetal heart rate patterns that do not require interventions by the nurse or health care provider. See Figure 10.38[55] for an illustration of a Category I tracing showing moderate FHR variability, accelerations, no decelerations, and uterine contractions about every eight minutes suggesting Stage 1 early labor.[56]
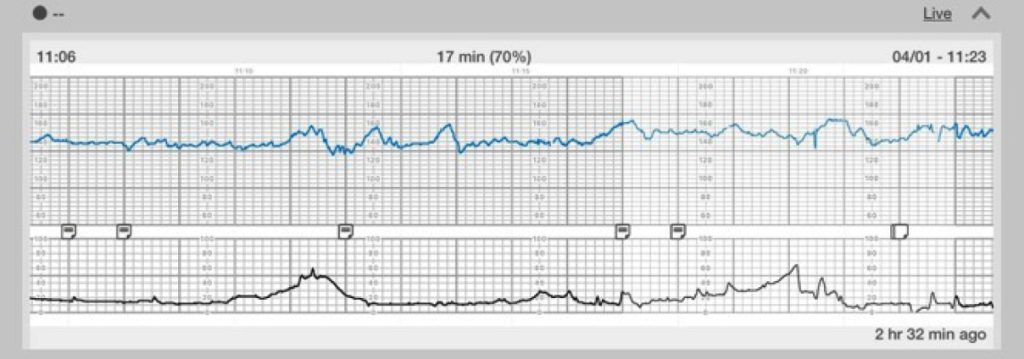
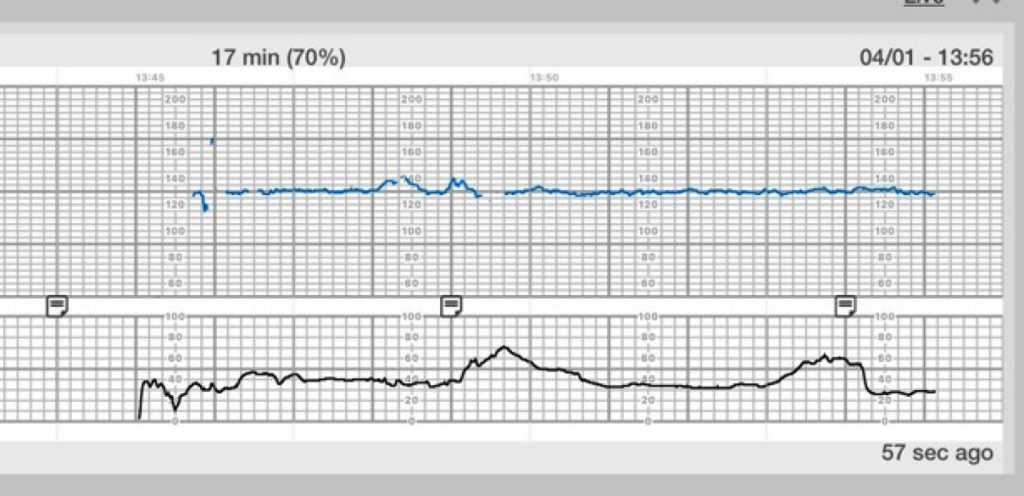
Category II is an indeterminate category, meaning it does not clearly indicate a normal or abnormal pattern. It raises concerns and requires close monitoring for additional signs of fetal distress. See Figure 10.39[57] for an illustration of a Category II tracing showing minimal FHR variability and uterine contractions about every four minutes. This tracing requires continued surveillance by the nurse with consideration of clinical circumstances and notification of the health care provider.[58]
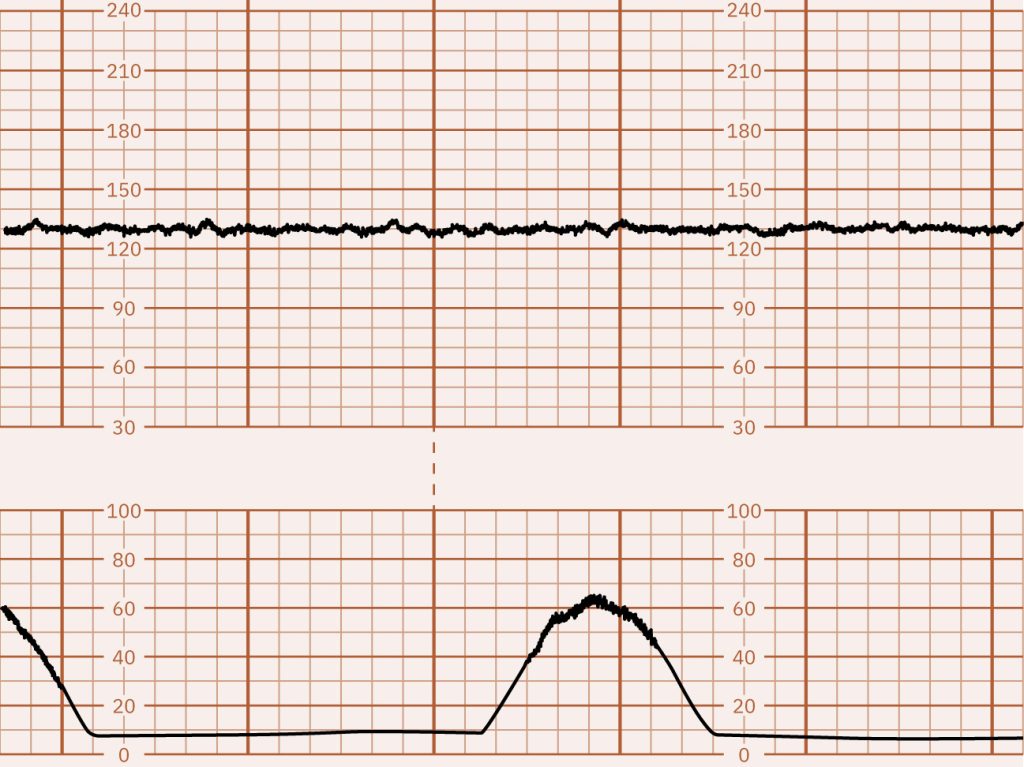
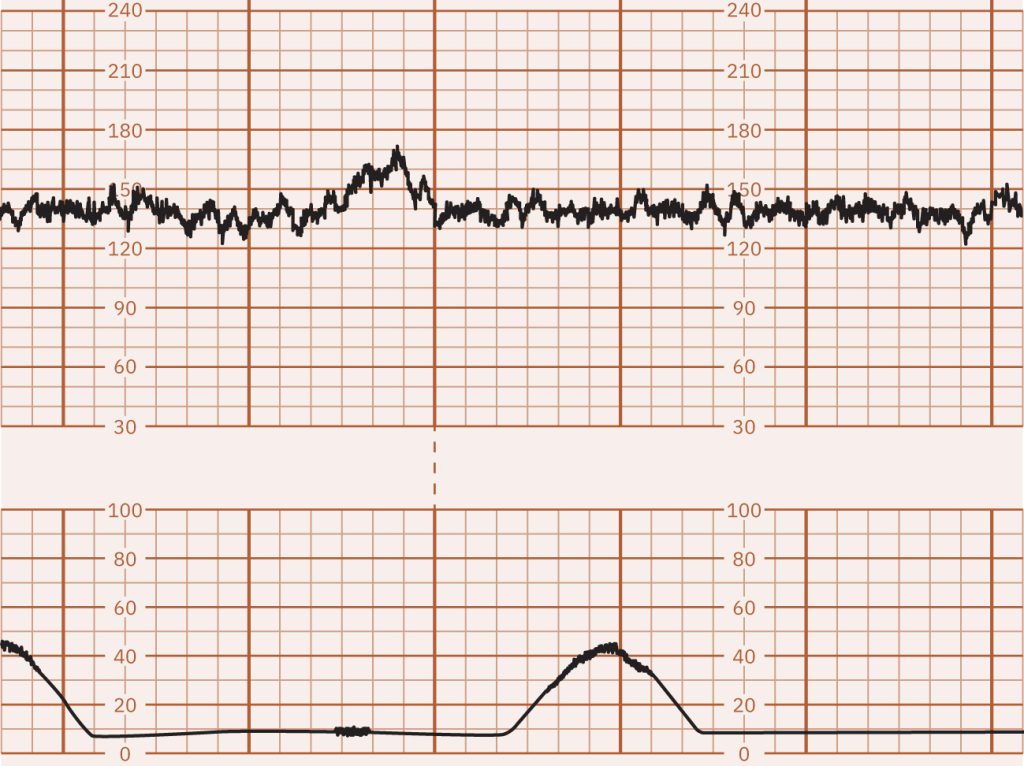
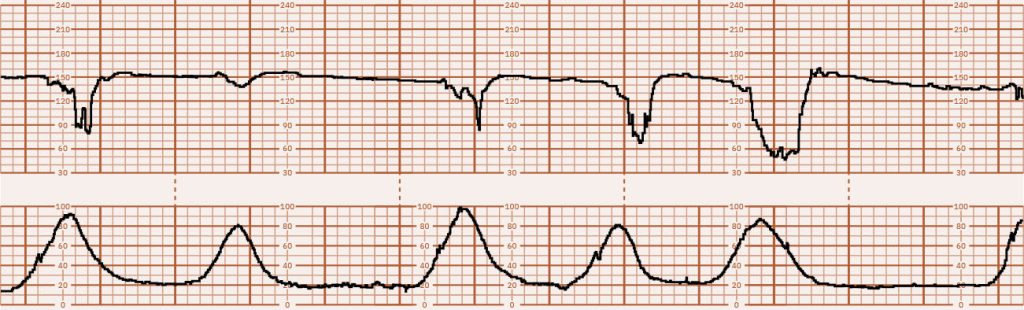
Category III represents abnormal fetal heart rate patterns associated with an increased risk of fetal acidosis. Category III patterns require immediate intervention and notification of the health care provider, as they may indicate fetal distress. Prompt nursing interventions may include intrauterine resuscitation and preparing for an emergency cesarean section if necessary. See Figure 10.40[59] for an illustration of a Category III FHR tracing showing absent FHR variability with a pattern of variable decelerations associated with uterine contractions that are occurring every two to three minutes.[60]
Intrauterine Resuscitation Nursing Interventions
If Category III FHR patterns occur, nurses perform intrauterine resuscitation interventions to help restore fetal blood flow and oxygenation while the health care provider is notified. The steps involved in intrauterine resuscitation are as follows[61]:
- Rotating the laboring client to the left or right lateral position to relieve supine hypotension or hypertension.
- Initiating IV fluid bolus to correct hypotension by increasing hydration, which increases perfusion.
- Administering oxygen at 10 L/min via a non-rebreather mask if maternal oxygen saturation is decreased.
- If oxytocin is being administered, discontinuing administration to decrease the intensity of uterine contractions and allow for reoxygenation of the fetus.
- Administering prescribed terbutaline to resolve tachysystole or elevated uterine resting tone.
- Amnioinfusion may be ordered to replace amniotic fluid by adding fluid back to the uterus. A bag of normal saline or lactated ringer solution is connected to a port on the intrauterine pressure catheter, and fluid is infused as a bolus or at a continuous rate. The extra fluid allows more space for the umbilical cord and can relieve cord compression. The nurse monitors the pressure of the uterus during the amnioinfusion to avoid overdistention. Amnioinfusion is contraindicated during fetal distress, active genital herpes infection, placenta previa, placental abruption, or fetal malpresentation. Complications can occur during amnioinfusion such as chorioamnionitis, umbilical cord prolapse, prolonged labor, and perforated uterus.[62]
Documentation of FHR Monitoring
Documentation of FHR monitoring is determined by agency policy. A process for evaluating and documenting fetal monitor tracings typically includes the following steps[63]:
- Document external or internal monitoring.
- Describe FHR baseline rate and variability.
- Describe the presence or absence of FHR accelerations or decelerations. If decelerations are present, identify the type of deceleration.
- Document the uterine contraction pattern, including frequency, duration, intensity, and presence or absence of uterine resting tone.
- Interpret the tracing and identify the tracing as Category I, II, or III.
- Document the plan of care, including communication with the client and the health care provider, as well as new orders received and implemented.
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- “4055b8171d601f862ac544467e1d7d71b8a68720” by Rice University/OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/maternal-newborn-nursing/pages/16-2-external-and-internal-monitoring ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- “8fc6e1fbf996cf3cf9f4fe36968949f53d44da19” by Rice University/OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/maternal-newborn-nursing/pages/16-2-external-and-internal-monitoring ↵
- “da980e8eb81a2be9351152153e761255f0292f33” by Rice University/OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/maternal-newborn-nursing/pages/16-2-external-and-internal-monitoring ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- “125830c9d86e0f03b4e25b60bb2bae43e32beb2f” by Rice University/OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/maternal-newborn-nursing/pages/16-2-external-and-internal-monitoring ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- “dbe72fa41b49b48100e71cb8194258e753bb3d82” by Rice University/OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/maternal-newborn-nursing/pages/16-2-external-and-internal-monitoring ↵
- “d334738d7da32b16ed3e8d5a4d5834bf460643f9” by Rice University/OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/maternal-newborn-nursing/pages/16-2-external-and-internal-monitoring ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- “FHR Tracing on Graph Paper” by Meredith Pomietlo is licensed under CC BY-NC 4.0 ↵
- “ef4179a40dbdc8211915812e197ffd889f418dd5” by Rice University/Open Stax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/maternal-newborn-nursing/pages/16-1-basic-terms-of-fetal-heart-rate-and-contraction-patterns ↵
- “13f7c7b2ae784332f5daa9c8d1797326bd0c00f2” by Rice University/OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/maternal-newborn-nursing/pages/16-1-basic-terms-of-fetal-heart-rate-and-contraction-patterns ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Jones, L. E., Whitburn, L. Y., Davey, M.-A., & Small, R. (2015). Assessment of pain associated with childbirth: Women׳s perspectives, preferences and solutions. Midwifery, 31(7), 708–712. https://doi.org/10.1016/j.midw.2015.03.012 ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- “8c4215d2bb37aabcaf14bcb2f2355906330002a9” by Rice University/OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/maternal-newborn-nursing/pages/16-1-basic-terms-of-fetal-heart-rate-and-contraction-patterns ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Boushra, M., Stone, A., & Rathbun, K.M. (2023). Umbilical cord prolapse. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK542241/ ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- “b8691535ef75eb4e7c341d634957d0b7f73d56c9” by Rice University/OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/maternal-newborn-nursing/pages/16-1-basic-terms-of-fetal-heart-rate-and-contraction-patterns ↵
- “b03b4985f80f1dbf93e41520d2cef1ae628f8397” by Rice University/OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/maternal-newborn-nursing/pages/16-1-basic-terms-of-fetal-heart-rate-and-contraction-patterns ↵
- “16bbe150a780629d245f6a2e5a01e5a8d73a2e62” by Rice University/OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/maternal-newborn-nursing/pages/16-1-basic-terms-of-fetal-heart-rate-and-contraction-patterns ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- “16bbe150a780629d245f6a2e5a01e5a8d73a2e62” by Rice University/OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/maternal-newborn-nursing/pages/16-1-basic-terms-of-fetal-heart-rate-and-contraction-patterns ↵
- Savirón-Cornudella, R., Bielsa, A.L. Esteban-Escaño, J., et al. (2024). Diagnosis of cardiotocographic sinusoidal patterns by spectral analyses. Biomedical Signal Processing and Control, 93, 106174. https://www.sciencedirect.com/science/article/pii/S1746809424002325 ↵
- “fbbc1115019e255aa48a1a1e65ea9178e4f5f12a” by Rice University/OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/maternal-newborn-nursing/pages/16-1-basic-terms-of-fetal-heart-rate-and-contraction-patterns ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- “3e6ddacd545c294b6d38e7d516beb8d30c5d5d53” by Rice University/OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/maternal-newborn-nursing/pages/16-1-basic-terms-of-fetal-heart-rate-and-contraction-patterns ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- “44de509286d4052f4b318129eb8a0eeacf4ae574” by Rice University/OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/maternal-newborn-nursing/pages/16-1-basic-terms-of-fetal-heart-rate-and-contraction-patterns ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- “b3e8d0bde6e7209e06cd5ddefeeaf0d9f0b79f36” by Rice University/OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/maternal-newborn-nursing/pages/16-1-basic-terms-of-fetal-heart-rate-and-contraction-patterns ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- “5d1f21a3ca24017350a03cf4385a47739ab480d8” by Rice University/OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/maternal-newborn-nursing/pages/16-1-basic-terms-of-fetal-heart-rate-and-contraction-patterns ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- “898383830d340423245a5807b33922551d0f1a3d” by Rice University/OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/maternal-newborn-nursing/pages/16-1-basic-terms-of-fetal-heart-rate-and-contraction-patterns ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- American College of Obstetricians and Gynecologists. (2009). ACOG Practice Bulletin No. 106. Intrapartum fetal heart rate monitoring: Nomenclature, interpretation, and general management principles. Obstetrics & Gynecology, 114(1), 192–202. https://doi.org/10.1097/aog.0b013e3181aef106 ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- “0b1954a7c6892c0c8e3f422915dc83715162cf7a” by Rice University/OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/maternal-newborn-nursing/pages/16-2-external-and-internal-monitoring ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- “586baeadbab451e321145c5353e91867e1407851” by Rice University/OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/maternal-newborn-nursing/pages/16-2-external-and-internal-monitoring ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- “9b5ca3841325cd414f4961731cc26f711fa79f24” by Rice University/OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/maternal-newborn-nursing/pages/16-2-external-and-internal-monitoring ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
Evaluating the fetal heart rate (FHR) in response to uterine contractions (UC) by using intermittent monitoring or continuous electronic fetal monitoring.
Refers to a technique of listening to and counting the fetal heart rate for a specific amount of time during specified intervals throughout labor to assess fetal well-being.
Similar to a stethoscope but uses bone conduction to better detect FHR.
A handheld device that uses ultrasonic waves to detect FHR.
Pressure sensitive contraction transducer which records the pressure force produced by the contorting abdomen during uterine contractions.
Affixes to the scalp of the fetus and monitors the fetal heart rate.
Placed inside the uterus and measures the duration, intensity, and frequency of uterine contractions, as well as the resting tone of the uterus.
The average beats per minute in a 10-minute segment, excluding periodic changes or marked variability.
A sustained FHR baseline greater than 160 bpm for ten minutes.
FHR baseline less than 110 beats for ten minutes.
Medications used to relax the uterus that help facilitate blood flow to the uterus.
Refers to the beat-to-beat fluctuations in the FHR baseline caused by stimulation of the fetal sympathetic and parasympathetic nervous systems.
Considered normal and indicates fluctuations in FHR between 6 and 25 bpm above or below baseline.
The fetal heart rate shows slight fluctuations of 5 bpm or less.
The fetal heart rate shows very little or no fluctuation and appears flat or nearly flat.
Refers to a wavelike pattern with regular frequency (three to five per minute) and amplitude.
Accelerations and decelerations of the FHR in relation to the FHR baseline.
Abrupt but temporary increases in the FHR above the baseline with an onset-to-peak of less than 30 seconds.
Intermittent decreases in the FHR below baseline, classified as early, late, variable, and prolonged.
A gradual, uniform decrease in FHR that returns to baseline and mirrors the uterine contraction.
Decelerations in the FHR below the baseline that start during a uterine contraction and continue after completion of the contraction.
Lowest point.
A lack of oxygenated blood coming from the uterus to the placenta.
Contractions occur too frequently or last longer than two minutes.
Abrupt decelerations of FHR of at least 15 bpm below the baseline that last at least 15 to 30 seconds.
Isolated, sporadic decelerations of at least 15 bpm from the FHR baseline that last two to ten minutes from onset to return to baseline.
Too little amniotic fluid.
A procedure that adds fluid to the amniotic sac.
Have enough duration, strength, and frequency to cause the cervix to dilate and efface and move the fetus through the maternal pelvis.
Refers to more than five uterine contractions in ten minutes or a contraction length of two or more minutes within a 30-minute period.
Represents normal and reassuring fetal heart rate patterns that do not require interventions by the nurse or health care provider.
An indeterminate category, meaning it does not clearly indicate a normal or abnormal pattern.
Represents abnormal fetal heart rate patterns associated with an increased risk of fetal acidosis.
Interventions to help restore fetal blood flow and oxygenation.

