18.4 Benign Breast Disorders
Benign breast changes include noncancerous conditions that are often associated with fluctuations in hormones. In most cases, benign breast changes resolve on their own or are easily treated, but a few may increase the future risk of breast cancer.[1]
Read more about breast cancer in the “Female Reproductive System Disorders” section of the “Reproductive Concepts” chapter.
Fibrocystic Breast Changes
Fibrocystic breast changes can occur in one or both breasts and cause lumpiness, nodularity, or pain. They are caused by cyclic hormonal changes associated with the menstrual cycle and represent the most common benign breast disease in women between 20 and 50 years of age. Other risk factors include excess consumption of dietary fat, caffeine, and nicotine. See Figure 18.1[2] for an illustration comparing a normal breast and a breast with fibrocystic breast changes.[3]
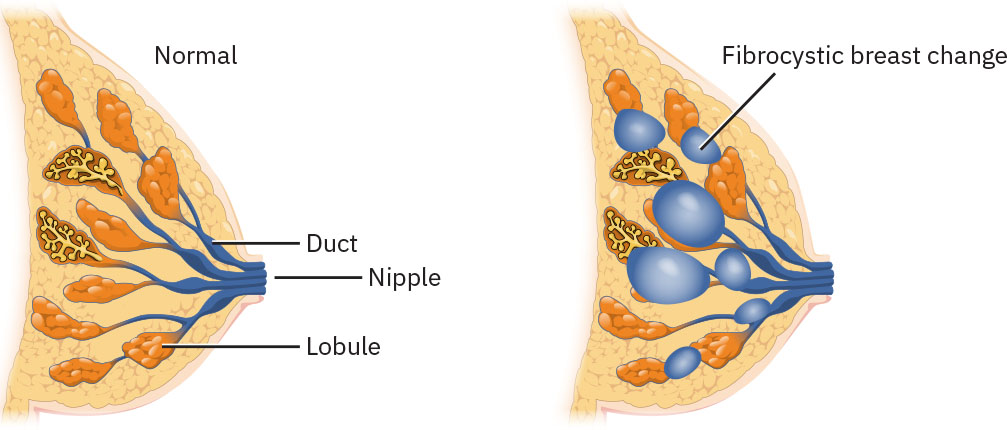
Symptoms associated with fibrocystic breast changes may include fullness or heaviness in the breast(s); tenderness in the upper, outer quadrant of the breast; and palpable, well-differentiated, and movable cysts. These symptoms tend to worsen the week before menstrual flow and improve within a week after menstrual flow begins.[4]
Fibrocystic breast changes are found during palpation on a clinical breast exam and feel firm and “ropelike.” A diagnostic mammogram and/or ultrasound is typically ordered by the health care provider for further evaluation. If cysts are found containing fluid, the fluid is aspirated and sent for pathologic examination to rule out cancer. If cysts are found that are solid, a fine-needle aspiration may be performed for pathologic examination of the cells to rule out cancer.[5]
Fibrocystic breast changes usually require only conservative management with a “watch and wait” approach after diagnosis is confirmed. In some cases, oral contraceptives can improve fibrocystic breast changes, but they may cause worsening of symptoms. Rarely, the provider may recommend surgical removal of the cyst or lump, usually only in cases where it is causing significant discomfort or distress to the client.[6]
Nurses provide health teaching about fibrocystic breast changes and can suggest the following strategies to reduce discomfort[7]:
- Use nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen for cyclical discomfort
- Reduce caffeine and alcohol consumption
- Avoid nicotine
- Wear a supportive bra
- Use heating pads for comfort
- Apply topical vitamin E oil
Fibroadenomas
Fibroadenomas are painless, solid, noncancerous tumors found in breast tissue. They can occur in people of all ages but are most common in women between 14 and 35 years old. See Figure 18.2[8] for an illustration of a fibroadenoma. It is hypothesized that fibroadenomas may be related to hormonal receptivity in the breast tissue. However, a key difference between fibrocystic changes and fibroadenomas is that fibroadenomas do not change in size during the menstrual cycle. Instead, they tend to stay constant in size or grow slowly with time. However, fibroadenomas may enlarge with pregnancy and decrease in size after menopause. In most cases, fibroadenomas do not increase a person’s risk for breast cancer. However, one type of fibroadenoma called a complex fibroadenoma may slightly increase breast cancer risk.[9]
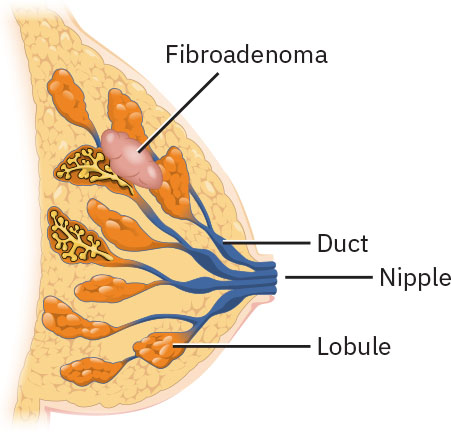
The most common symptom of a fibroadenoma is a small, solitary, painless lump in the breast tissue, usually less than 2.5 centimeters in diameter. Some people develop multiple fibroadenomas or fibroadenomas in both breasts. Fibroadenomas are typically well-defined, round, rubbery in consistency, and easy to move within the tissue. While the tumors don’t cause pain, some women experience tenderness at certain points in their menstrual cycle.[10]
Fibroadenomas are diagnosed based on findings during clinical exam, mammogram, ultrasound, and possibly a biopsy[11]:
- Mammography: Mammography is an X-ray procedure that uses low doses of radiation to examine the breast for cancer and other disorders. Fibroadenomas appear as distinct growths with smooth, round borders.
- Ultrasonography: Ultrasound imaging of the breast helps to distinguish fluid-filled cysts from solid structures. Fibroadenomas appear as round, well-defined masses that are hypoechogenic (i.e., have a decreased response to the ultrasound waves, producing a dark gray image).
- Biopsy: A biopsy is a medical procedure in which a small sample of tissue is removed from the body for examination under a microscope. Breast biopsy may be performed in women over 30 years of age to rule out cancer. A small sample of the tumor is taken either by fine-needle aspiration (FNA) or by core biopsy using ultrasound guidance.
In most cases, simple fibroadenomas do not require treatment and spontaneously resolve over time. However, large or complex fibroadenomas can increase the risk of developing breast cancer and may be treated by lumpectomy, where the lump (mass), as well as a small amount of breast tissue, is removed. Cryoablation, a procedure where a cryoprobe is inserted into the tumor to freeze and destroy the tumor cells, is an alternative to surgery.[12]
Intraductal Papilloma
Intraductal papilloma is a benign tumor that grows inside the milk ducts of the breasts. These tumors are wart-like and made of fibrous tissue, gland tissue, and blood vessels. See Figure 18.3[13] for an illustration of an intraductal papilloma. An individual, single tumor that grows close to the nipple in the larger milk ducts is called a solitary papilloma. Solitary papillomas can cause an unusual bloody or clear nipple discharge. Clients may present to the office due to feeling a painful lump near the nipple. Papillomas found in the smaller milk ducts farther from the nipple are called multiple papillomas and do not produce nipple discharge.[14]
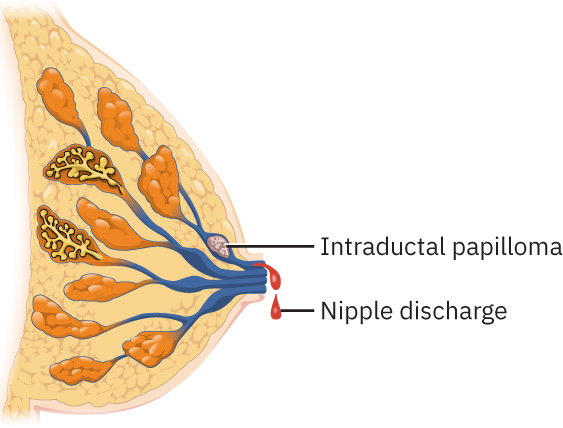
Thyroid and prolactin levels are typically ordered for clients with nipple discharge to confirm the discharge is not due to another medical issue. Galactorrhea (milk production not related to pregnancy or breastfeeding) may be caused by endocrine problems, neurologic disorders, or side effects of certain medications. A diagnostic mammogram and/or ultrasound of the breast is ordered for nipple discharge associated with breast masses to rule out breast cancer. A ductogram may also be performed, where dye is injected into the leaking duct and an X-ray is taken to determine if a papilloma is present and causing the nipple discharge. A breast biopsy may be performed for definitive diagnosis of a papilloma.[15]
In most cases, asymptomatic intraductal papillomas are monitored with regular exams and/or imaging tests and do not require treatment. However, large or painful papillomas may be surgically removed.[16]
Mastalgia
Mastalgia refers to breast pain that can be cyclical or noncyclical. Cyclical mastalgia is breast pain associated with the menstrual cycle that begins around the time of ovulation and resolves with menstruation. It may vary from mild pain to such severe pain that tight-fitting clothing or close contact with others is avoided. Treatment may include avoiding caffeine, taking vitamin E supplements, and eating a low-fat diet. In severe cases, oral contraceptives or hormone blockers may be prescribed. Noncyclical mastalgia does not vary with the menstrual cycle and is generally constantly present in one location. Treatment is based on the cause and severity of the pain.[17]
Nonlactation Mastitis
Nonlactation mastitis (NLM) is breast tissue inflammation in a woman who is not breastfeeding, which may or may not be associated with an infection. An infection can be caused by several microorganisms, although most are caused by Staphylococcus and are treated with appropriate antibiotics.
Periductal mastitis (PDM), or mammary ductal ectasia, is chronic inflammation of the breast tissue. PDM causes dilated mammary ducts with thickened walls and leakage of fluid into the surrounding tissue, resulting in inflammation and fat necrosis and sometimes the formation of an abscess. See Figure 18.4[18] for an illustration of PDM. PDM is associated with obesity, smoking, and diabetes mellitus. Signs and symptoms of PDM are pain or redness in the skin of the breast, nipple inversion, greenish nipple discharge, and fever.[19]
Because NLM and PDM have similar signs and symptoms as breast cancer, careful evaluation and diagnosis are crucial. Imaging such as ultrasound of the breast, diagnostic mammography, or magnetic resonance imaging (MRI) may be ordered by the health care provider for further evaluation. However, mammography can be extremely painful for clients with an infection or abscess. Drainage from the nipple is sent for pathologic evaluation and culture and sensitivity tests to determine the presence of infection and guide antibiotic treatment. Fine-needle aspiration or tissue biopsy may be performed to evaluate potential causes of abnormalities such as inflammation, infection, or cancer.[20]
Medical treatment of NLM and PDM may include the following[21]:
- Antibiotics based on the culture and sensitivity results
- Pain medication as indicated
- Surgical incision and drainage of an abscess, if present
- Hospitalization if signs of sepsis are present, if the infection does not respond to oral antibiotic treatment and continues to progress, or if the client is clinically unstable
Nurses provide health teaching about NLM and PDM and suggest comfort measures to help alleviate pain and promote healing that may include the following[22]:
- Applying heat or cold to the affected area
- Requesting referral for lymphatic drainage treatment
- Wearing a supportive bra
- Sleeping on the unaffected side
- Using breast pads to contain leakage or drainage
Gynecomastia
Gynecomastia refers to increased breast gland tissue in males associated with a drop in testosterone levels compared to estrogen. Gynecomastia may be caused by hormonal changes, side effects of certain medications, pituitary conditions, hyperthyroidism, kidney failure, liver failure, malnutrition, or recreational use of drugs or alcohol. Pseudogynecomastia is an increase in fat but not gland tissue in male breasts.[23]
Diagnostic tests are performed to determine the cause of gynecomastia and to check for breast cancer, as indicated. Gynecomastia often spontaneously resolves on its own but may require medical treatment if caused by a medical condition or if the condition causes pain or embarrassment. Medications may be prescribed by the health care provider, or surgery may be performed to reduce breast tissue.[24]
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- “06e6ce91be81be7c7fe9fb6e3745019d466e8790” by Rice University/Open Stax is licensed under CC BY 4.0. https://openstax.org/books/maternal-newborn-nursing/pages/8-1-benign-disorders-of-the-breast ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- “5b5a4fb7a7e1b95a66d8b739c4728506274844b5” by Rice University/Open Stax is licensed under CC BY 4.0. https://openstax.org/books/maternal-newborn-nursing/pages/8-1-benign-disorders-of-the-breast ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- “cdfb41fa3c51b921f4e5486932eaf8de8ba31a3b” by Rice University/Open Stax is licensed under CC BY 4.0. https://openstax.org/books/maternal-newborn-nursing/pages/8-1-benign-disorders-of-the-breast ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Johns Hopkins Medicine. (n.d.). Breast pain (mastalgia). https://www.hopkinsmedicine.org/health/conditions-and-diseases/mastalgia-breast-pain#:~:text=Mastalgia%20is%20breast%20pain.,and%20breast%20pain%20will%20appear ↵
- “694f635b9a75af7a987349a1a84aa177bebc3156” by Rice University/Open Stax is licensed under CC BY 4.0. https://openstax.org/books/maternal-newborn-nursing/pages/8-1-benign-disorders-of-the-breast ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Mayo Clinic. (2023). Enlarged breasts in men (gynecomastia). https://www.mayoclinic.org/diseases-conditions/gynecomastia/symptoms-causes/syc-20351793 ↵
- Mayo Clinic. (2023). Enlarged breasts in men (gynecomastia). https://www.mayoclinic.org/diseases-conditions/gynecomastia/symptoms-causes/syc-20351793 ↵
A common, non-cancerous condition that causes breast tissue to swell, become lumpy, or feel tender.
Painless, solid, noncancerous tumors found in breast tissue.
A noncancerous breast tumor that contains abnormal tissue changes, such as cysts, calcifications, or scar tissue.
An X-ray procedure that uses low doses of radiation to examine the breast for cancer and other diseases.
Imaging of the breast helps to distinguish fluid-filled cysts from solid structures.
A medical procedure in which a small sample of tissue is taken from the body for examination under a microscope to diagnose conditions such as cancer.
A surgical procedure to remove a breast tumor and some of the surrounding tissue.
A cryoprobe inserted into the tumor to freeze and destroy the tumor cells.
A benign tumor that grows inside the milk ducts of the breasts.
Milk production not related to pregnancy or breastfeeding.
Dye is injected into the leaking duct and an X-ray is taken to determine if a papilloma is present and causing the nipple discharge.
Breast pain that can be cyclical or noncyclical.
Breast pain associated with the menstrual cycle that begins around the time of ovulation and resolves with menstruation.
Breast pain which does not vary with the menstrual cycle and is generally constantly present in one location.
Breast tissue inflammation in a woman who is not breastfeeding, which may or may not be associated with an infection.
Also known as mammary ductal ectasia, is chronic inflammation of the breast tissue.
Increased breast gland tissue in males associated with a drop in testosterone levels compared to estrogen.
An increase in fat but not gland tissue in male breasts.

