10.7 Complications Associated With Labor
The majority of clients have uncomplicated birthing experiences. However, specific complications can occur during any stage of labor due to a pregnant woman’s preexisting condition or a complication that develops during labor. The nurse must be aware of common complications that may occur during labor and be ready to provide applicable nursing interventions while notifying the health care provider. Ensuring the safety of the laboring client and the fetus is the responsibility of the health care team.[1] This section will discuss common complications and medical interventions that may occur during labor. Specific complications associated with the second and third stages of labor are discussed in the “Complications and Medical Interventions During the Second Stage of Labor” and “Complications and Medical Interventions During the Third Stage of Labor” sections.
Premature Labor
Labor occurring from 20 weeks’ gestation to 36 6/7 weeks’ gestation is classified as preterm labor. Spontaneous preterm labor can be caused by several factors, including premature cervical dilation, cervical insufficiency, uterine abnormalities, infection, fetal anomalies, multiple gestations, or polyhydramnios (excessive amniotic fluid).[2]
Preterm prelabor rupture of membranes (PPROM) refers to rupture of amniotic membranes prior to the 37th completed week of gestation and before spontaneous labor. The most common risk factors for PPROM are low socioeconomic status, young or advanced maternal age, smoking, periodontal disease, multiple gestations, polyhydramnios, gestational hypertension, maternal diabetes, prior preterm birth, and fetal anomalies.[3]
Clients in preterm labor are typically admitted to a hospital setting where the client and fetus can be closely observed until contractions cease and imminent delivery is no longer anticipated. Tocolytic medications may be administered to reduce the strength and frequency of uterine contractions so that antenatal corticosteroids, such as betamethasone, can be administered to promote fetal lung maturity. Examples of tocolytic medications are terbutaline, indomethacin, and nifedipine. In specific cases, magnesium sulfate may be administered.[4]
Terbutaline
Terbutaline may be prescribed for clients with preterm labor. Terbutaline is a tocolytic that selectively stimulates beta-2 adrenergic receptors, relaxes smooth muscle, and, therefore, stops uterine contractions. It is contraindicated with ischemic heart disease, hypertension, arrhythmias, diabetes mellitus, seizure disorders, hyperthyroidism, and tachycardia greater than 120 beats per minute. It is not approved for prolonged tocolysis greater than 48 to 72 hours. Serious adverse effects include increased heart rate, transient hyperglycemia, hypokalemia, cardiac arrhythmias, pulmonary edema, myocardial infarction, increased fetal heart rate, and neonatal hypoglycemia. It has a boxed warning against prolonged use past 48 to 72 hours related to these maternal cardiac problems and risk of maternal death.[5]
Indomethacin
Indomethacin is a cyclooxygenase inhibitor (COX inhibitor) and nonsteroidal anti-inflammatory drug (NSAID) that inhibits prostaglandins released during labor. Prostaglandins soften the cervix and relax the cervical muscles, which helps the cervix dilate. They also increase intracellular calcium levels, which causes the myometrial muscle to contract and move the fetus through the maternal pelvis. Indomethacin helps stop these physiological actions of labor.
Adverse effects include gastrointestinal upset (nausea, vomiting, reflux, abdominal pain), thrombocytopenia, oligohydramnios, renal dysfunction, hypertension, and neonatal complications (chronic lung disease and intraventricular hemorrhage). It is contraindicated for maternal thrombocytopenia, renal impairment, gastrointestinal bleeding, or greater than 32 weeks’ gestation due to risk of premature closure of the fetal ductus arteriosus.[6]
Nifedipine
Nifedipine is a calcium channel blocker that blocks calcium ions from entering the uterine muscle cell membrane, which ultimately results in uterine wall relaxation. Adverse effects include nausea, vomiting, flushing, headache, dizziness, palpitations, hypotension, and peripheral edema. It is contraindicated with maternal hypotension, heart failure, and liver dysfunction.[7]
Magnesium Sulfate
Magnesium sulfate is a CNS depressant that decreases the release of acetylcholine and relaxes smooth muscle of the uterus. It is used primarily to prevent eclampsia but may also be used in some settings for short-term treatment of preterm labor to allow the administration of antenatal corticosteroids to promote fetal lung maturity. Adverse effects are related to magnesium toxicity that causes muscle weakness and can lead to respiratory depression and cardiac arrest.[8]
Labor Induction
Labor may be induced by the health care provider for several reasons, such as gestation greater than 41 weeks, oligohydramnios (not enough amniotic fluid surrounding the fetus), preeclampsia/hypertension, prelabor rupture of membranes, chorioamnionitis (infection of the amniotic membranes), intrauterine growth restriction (when the estimated weight of the fetus is less than the 10th percentile for gestational age), and nonreassuring fetal heart rate.
The stimulation of uterine contractions prior to the spontaneous onset of labor is called labor induction. When determining the appropriateness of labor induction, the health care provider considers the benefits to the pregnant woman and fetus compared to the risks of continuing the pregnancy. The cervix is evaluated to determine if it is ready for labor, commonly referred to as a “ripe” or “favorable” cervix. The Bishop score is a tool used to determine if the cervix is favorable for labor. See Table 10.7a for components of the Bishop score. The higher the Bishop score, the more favorable the cervix is for labor induction. If the Bishop score is low, the nurse anticipates administering a cervical ripening agent to prepare the cervix for labor.[9]
Table 10.7a. Bishop Score[10]
| Score | Dilation | Position of Cervix | Effacement | Station | Cervical Consistency |
|---|---|---|---|---|---|
| 0 | Closed | Posterior | 0–30% | −3 | Firm |
| 1 | 1–2 cm | Mid position | 40–50% | −2 | Medium |
| 2 | 3–4 cm | Anterior | 60–70% | −1, 0 | Soft |
| 3 | 5–6 cm | — | 80% | +1, +2 | — |
Cervical Ripening
Cervical ripening is a process by which the cervix softens and thins (effaces) in preparation for childbirth. This process is essential for the cervix to dilate sufficiently during labor to allow the fetus to pass through the birth canal. Cervical ripening can occur naturally as the body prepares for labor, but it may need to be accelerated prior to labor induction. Medical interventions to accelerate cervical ripening may include medications and/or the use of mechanical methods such as an indwelling catheter with a balloon.
Cervical ripening medications are prostaglandins that relax cervical smooth muscle and stimulate uterine contractions. They may be administered orally or inserted near the cervix. Examples of cervical ripening medications are misoprostol and dinoprostone. Adverse effects include uterine tachysystole, abdominal cramps, fever, chills, vomiting, and diarrhea. If tachysystole occurs, a tocolytic medication (such as terbutaline) can be administered.
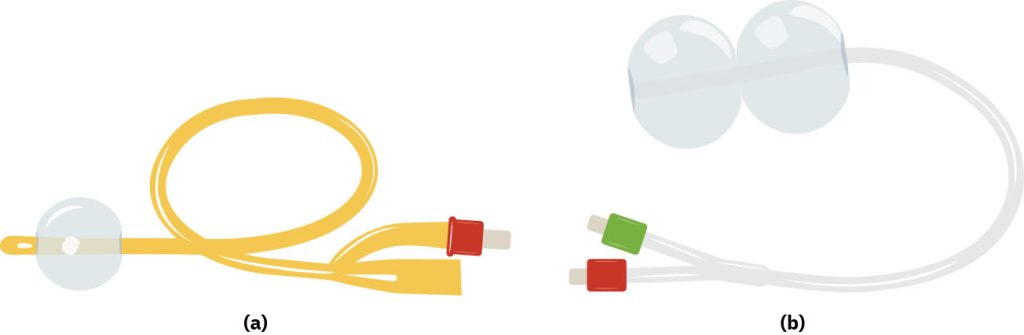
If an indwelling catheter with a balloon (commonly referred to as a Foley catheter) is used for cervical ripening, the tip of the catheter is inserted through the client’s cervical canal, and the balloon is inflated to put pressure on the internal cervical os. The balloon is usually in place for 8 to 12 hours. If a double balloon catheter is used, the catheter is inserted through the cervical canal, and the balloon at the internal cervical os is inflated with 30 to 60 milliliters of sterile saline or water and then the balloon at the outer cervical os is inflated. The catheter remains in place between 12 and 24 hours. See Figure 10.48[11] for illustrations of a balloon catheter and a double balloon catheter used for cervical ripening.
Oxytocin
Oxytocin is the most commonly used medication for labor induction. Oxytocin is a uterotonic (medications that promote uterine contractions) that binds to oxytocin receptors in the myometrium, increasing intracellular calcium and stimulating muscle contractions. The amount of oxytocin administered is adjusted during labor to facilitate regular contractions until delivery. Oxytocin is administered using an infusion pump and is infused in milliunits per minute. The typical time for the uterus to respond to the initiation of the infusion is three to five minutes. Oxytocin has a boxed warning and is classified as a high-risk medication by the Federal Drug Association (FDA). Adverse effects of oxytocin are related to overstimulation of the uterus and include fetal distress, fluid retention, and, in rare cases, uterine rupture. Fetal distress can occur if the frequency of contractions does not allow for placental perfusion and adequate fetal recovery and oxygenation. Fluid retention can occur because oxytocin has an antidiuretic action. A uterus that has been scarred from a previous cesarean birth or myomectomy (surgical removal of uterine fibroids) is at higher risk of rupture. The maximum dose of oxytocin is usually determined by agency policy. The nurse’s role when administering oxytocin is to prepare the client by teaching about its effects and possible adverse effects. Oxytocin-induced contractions may be stronger, more frequent, and more intense than those during natural labor, so the client may require analgesics.
Dystocia
When labor begins, the release of maternal oxytocin causes the involuntary activation of uterine smooth muscle fibers. While most clients have adequate contractions that allow for the progression of labor, some may have contractions that are inadequate. Dystocia refers to lack of progression of active labor that may require medical interventions. The American College of Obstetricians and Gynecologists (ACOG) defines arrest of labor during the active phase of the first stage of labor as no progression in cervical dilation in clients who are at least 6 cm dilated with rupture of membranes despite four hours of adequate uterine activity, or six hours of inadequate uterine activity with oxytocin augmentation. Prolonged second stage of labor is defined as more than three hours of pushing in nulliparous individuals and two hours of pushing in multiparous individuals.[12]
There are different categories of dystocia called uterine, pelvic, and fetal. Uterine dystocia is caused by lack of power, meaning that uterine contractions or the maternal pushing effort is inadequate to cause cervical changes that progress to birth. Pelvic dystocia is a problem of the passage, meaning that the pelvic outlet does not allow the passage of the fetus for birth. Fetal dystocia is a problem of the passenger, meaning that the fetus is unable to descend through the maternal pelvis for birth. Common factors associated with labor dystocia based on the “5 P’s of labor” include the following[13]:
- Power: Insufficient uterine contractions and/or pushing effort
- Passenger: Fetal malposition or malpresentation
- Passage: Inadequate pelvis inlet, midpelvis, or outlet
- Psyche: Client’s emotions regarding preparedness, anxiety, or lack of support regarding the labor and the birthing process
- Positioning: Position of the laboring client
Risk factors associated with each of the 5 P’s are outlined in Table 10.7b.
Table 10.7b. Risk Factors Associated With Labor Dystocia[14]
| Cause | Risk Factor |
|---|---|
| Power |
|
| Passenger |
|
| Passage |
|
| Psyche |
|
| Positioning |
|
Uterine Dystocia
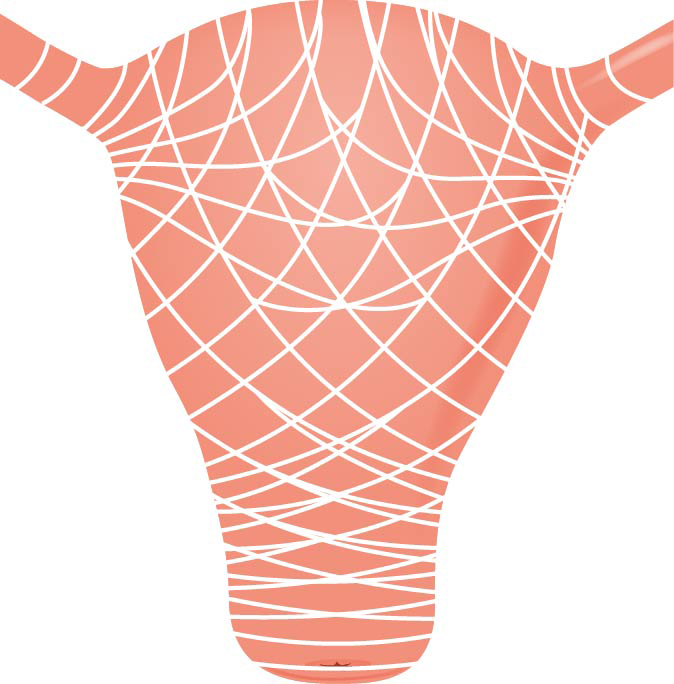
During a normal uterine contraction pattern, the upper uterine muscles shorten during the contraction to elongate the lower uterine segment, which results in dilation and effacement of the cervix, as well as descent of the fetal head. During uterine dystocia, there is insufficient contraction strength, frequency, or duration to cause changes and descent of the fetal head. See Figure 10.49[15] for an illustration of the uterine muscles.[16]
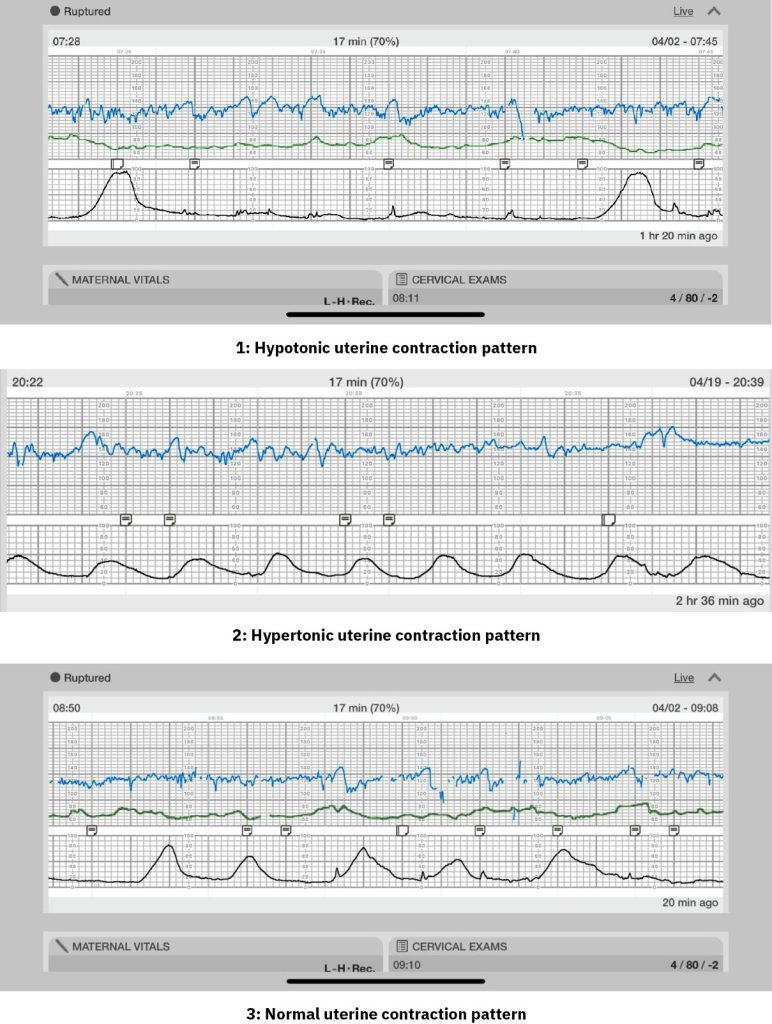
Electronic fetal monitoring strips offer cues that uterine dystocia is occurring. See Figure 10.50[17] for a comparison of fetal monitoring strips that compare three strips over 15 minutes. The first strip illustrates hypotonic uterine contractions where there are too few contractions. The second strip shows hypertonic uterine contractions with too many contractions that lack strength and duration, referred to as a tachysystole pattern. The third strip shows a normal uterine contraction pattern with five contractions of normal duration, intensity, and frequency over 15 minutes.[18]
As Table 10.7b describes, there are several possible factors that can cause uterine dystocia during the first stage of labor. Pregnant women experiencing long labors who have little to eat or drink can become exhausted, hypoglycemic, and/or dehydrated, preventing the uterine muscles from contracting properly. Emotional stress can occur due to fear or pain, causing the release of cortisol that inhibits oxytocin and the stimulation of contractions. A previous history of multiple gestations, a fetus that is large for gestational age or malpositioned, grand multiparity, and polyhydramnios are conditions that distend the uterus and decrease the strength of the uterine contractions. Epidural anesthesia can also decrease the strength and frequency of uterine contractions. If present, chorioamnionitis can cause inadequate contraction of the uterine muscle due to the inflammatory process of infection. The role of the nurse is to notice cues of prolonged labor and notify the health care provider, encourage hydration, assist with frequent movement and position changes, and provide emotional support to alleviate fear and stress in the laboring client.[19]
Uterine dystocia can also occur in the second stage of labor. When the cervix is fully dilated and the fetal head has descended, most clients feel an overwhelming urge to push. However, epidural anesthesia can reduce the urge to push. Second stage dystocia can also be caused by the same risk factors that can cause first stage uterine dystocia. Guidelines for the second stage of labor recommend that a nulliparous client push at least three hours, and a multiparous client push at least two hours prior to diagnosing dystocia. The role of the nurse during the second stage of labor is to provide support and assist in the pushing process.[20]
Pelvic Dystocia
Pelvic dystocia occurs when the size of the fetal head is larger than the size of the maternal pelvis due to a small capacity of the pelvic inlet, midpelvis, or pelvic outlet. Recall that during normal labor, the fetal head engages in the pelvic inlet and then as it descends into the midpelvis, the head flexes and rotates to the occiput-anterior (OA) position. The fetal head enters the pelvic outlet in a flexed OA position and exits the birth canal by the extension of the head. If any part of the pelvis is too small for these cardinal movements, fetal descent and cervical dilation and effacement stall.[21]
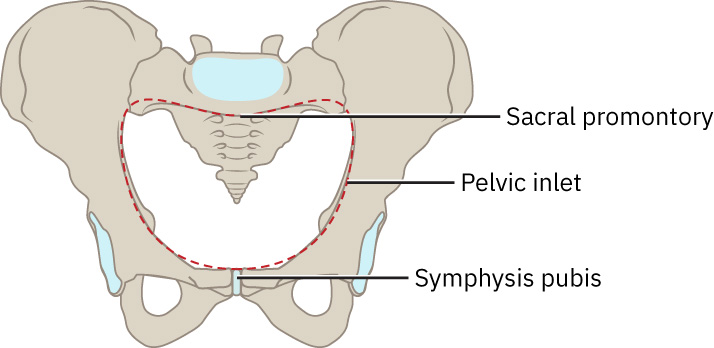
A normal pelvic inlet allows passage of a fetal head diameter of approximately 9.5 centimeters (cm). If the pelvic inlet is less than 10 cm, the fetal head may not be able to engage and pass through the pelvic inlet.[22] See Figure 10.51[23] for an illustration of the pelvic inlet.
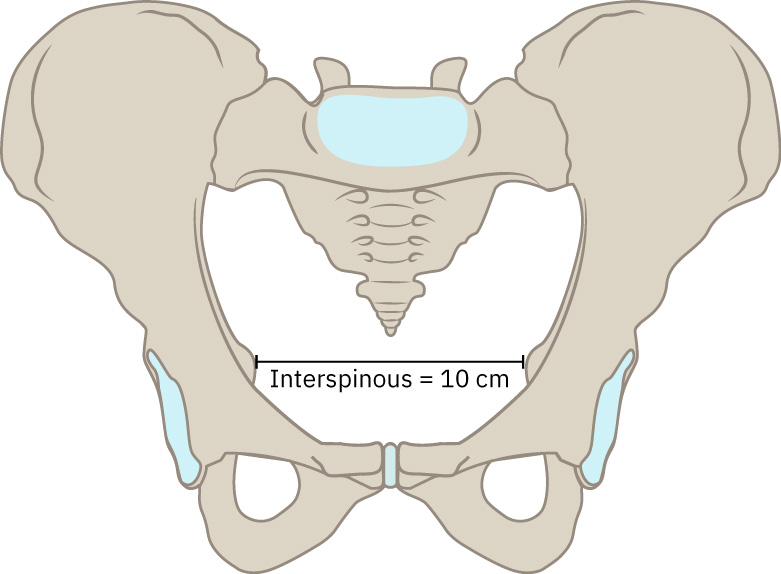
The midpelvis is measured by the distance between the ischial spines and should average more than 9 cm. See Figure 10.52[24] for an illustration of the midpelvis showing an interspinous space of 10 cm. When the nurse performs a cervical exam during labor, these ischial spines are the landmarks used for determining fetal station. However, if the ischial spines are encroaching and prominent, the nurse is aware that midpelvis dystocia could occur if the fetal head engages but is unable to flex or rotate anteriorly. If this type of dystocia occurs, fetal head molding can cause caput succedaneum (fluid underneath the fetal scalp that causes swelling).[25]
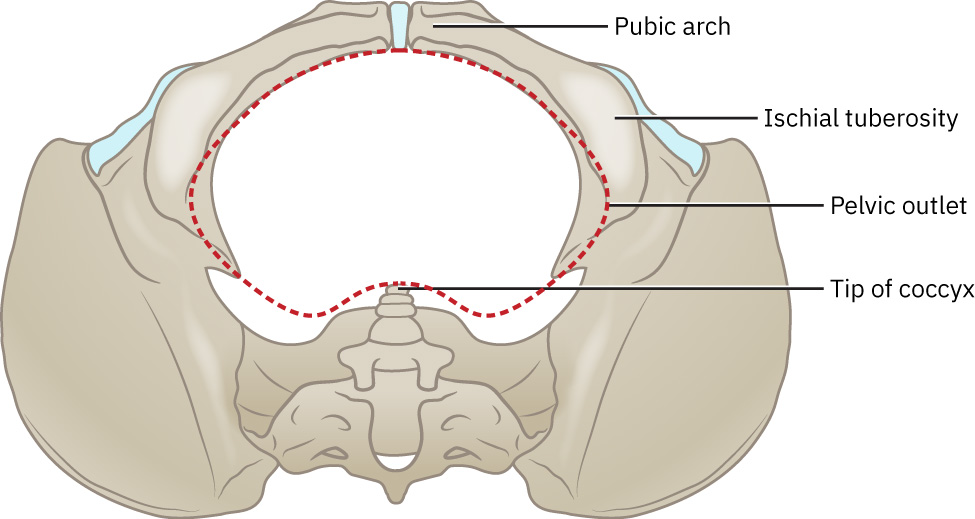
Pelvic outlet dystocia is seen when the distance between the ischial tuberosity is less than 8 cm. See Figure 10.53[26] for an illustration of the pelvic outlet. When the pelvic outlet is too small, the fetal head can become malpositioned as the fetus attempts to turn its head to find the path of least resistance through the pelvis. Pelvic outlet dystocia can lead to prolonged pushing, forceps birth, cesarean birth, and/or extreme caput succedaneum.[27]
Fetal Dystocia
Fetal dystocia refers to the inability of the fetal head to navigate through the maternal pelvis. Causes of fetal dystocia include occiput posterior or transverse fetal positions or brow or face fetal presentations. Occiput posterior or transverse fetal positions can stall cervical dilation due to a lack of pressure exerted on the cervix and can cause failure of the presenting part to descend. A brow or face presentation occurs when the fetal neck is hyperextended. A vaginal delivery may be possible if the fetal chin is directed at the maternal symphysis pubis (i.e., mentum anterior position). However, it is impossible for the fetal head to navigate the pelvis if the chin is pointing toward the maternal back (i.e., mentum posterior); therefore, a cesarean birth is necessary. The role of the nurse is to support and educate the laboring person and family regarding the possible changes in birth plan to a forceps or cesarean birth.[28]
Review fetal positions in the “Passenger” subsection of “The P’s of Labor.”
Medical Interventions for Labor Dystocia
Labor augmentation is the process of stimulating the uterus to increase the frequency, duration, and intensity of contractions after the onset of spontaneous labor contractions. It is commonly performed for lack of labor progression when ineffective uterine contractions are the underlying cause. Medical interventions to augment labor include oxytocin administration or a combination of amniotomy and oxytocin administration.
Review information about oxytocin administration under the “Labor Induction” subsection above. The nurse’s role in oxytocin administration during labor augmentation is to increase or decrease the administration rate according to the client’s uterine contraction pattern, fetal tolerability to the contractions, and health care provider orders. The nurse discontinues the oxytocin infusion in the presence of tachysystole, nonreassuring fetal heart rate pattern, or suspected uterine abruption or rupture, and immediately notifies the health care provider. When an oxytocin infusion is stopped, the amount of oxytocin in the plasma rapidly declines due to the drug’s 3- to 5-minute half-life.[29]
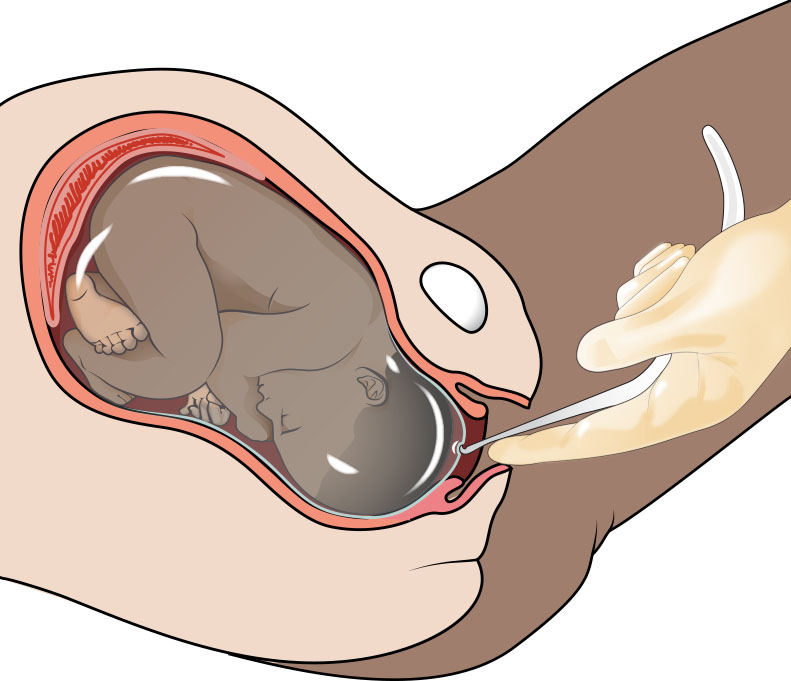
Amniotomy is the artificial rupture of the membranes (AROM) by a midwife or obstetrician using an amniotic hook. To prevent the risk of a prolapsed cord, the fetal head must be engaged in the pelvis prior to performing an amniotomy. Research indicates that performing an amniotomy alone during normal, spontaneous labor does not decrease the time to delivery or reduce the incidence of cesarean birth, but when performed in combination with oxytocin administration, labor is expedited by 1 to 1.5 hours.[30] See Figure 10.54[31] for an illustration of an amniotomy.
Precipitous Labor
Labor and delivery that are extremely rapid, usually less than three hours from start of the contractions to birth, is considered precipitous labor. Pregnant women may describe contractions that are very close together without a break between them, sudden strong contractions without a slow build, or experiencing a sudden urge to push. Although the cause is unknown, several risk factors have been associated with precipitous labor, such as a small fetus, a previous precipitous birth, high blood pressure, or cocaine use. Precipitous birth can cause lower 1-minute Apgar scores and increase the risk for postpartum hemorrhage, newborn respiratory distress, third- or fourth-degree lacerations, and placental abruption.[32]
For precipitous labor occurring in a hospital setting, the nurse focuses on promoting the well-being of the laboring client and the fetus. Clients may have increased anxiety or panic due to the rapid progression. The nurse should speak in a calm manner, explaining what to expect and reassuring the client they are safe. In preparing for the upcoming delivery, the nurse should ensure medications to treat postpartum hemorrhage are readily available. If the infant is born prior to the health care provider’s arrival, the nurse follows agency policy in assisting in the delivery of the infant, drying the infant, cutting the umbilical cord, and placing the infant skin-to-skin on the client’s chest, with the top priority being keeping the infant warm. The pediatric team should be in the room in case the infant does not begin breathing spontaneously after the rapid descent and birth. If the placenta is delivered spontaneously before the health care provider is present in the room, the nurse should be prepared to administer oxytocin per agency protocol to decrease the risk of postpartum hemorrhage.[33]
Conditions Associated With the Amniotic Membranes and Fluid
The amniotic sac is filled with amniotic fluid and consists of two layers called the amnion and chorion. The amnion is the inner layer and the chorion the outer layer. They lie so closely together that sometimes they cannot be separated. The purpose of the amniotic fluid is to provide cushioning to protect the fetus, to maintain an appropriate temperature, and to allow the fetus to move and grow unrestricted.
Complications affecting the amniotic fluid consist of oligohydramnios, polyhydramnios, chorioamnionitis, and meconium-stained fluid. These complications can affect labor progression and pose risks to the client and fetus. Oligohydramnios and polyhydramnios are typically diagnosed prior to labor, while meconium-stained fluid and chorioamnionitis are typically diagnosed during labor. Each of these conditions is further discussed in the following subsections.
Oligohydramnios
Oligohydramnios is the lack of sufficient amniotic fluid, typically less than 500 milliliters (mL). This amount is usually measured during ultrasound examination. Causes of oligohydramnios can be fetal or maternal, so identifying the causative agent is important to determine treatment. Premature rupture of membranes, placental insufficiency, multiple gestation, fetal anomalies, and maternal medication use can cause oligohydramnios. For example, indomethacin, a medication used to treat preterm labor, is associated with oligohydramnios. Symptoms of oligohydramnios are fluid leaking from the vagina, poor or lack of uterine growth, or decreased fetal movements. Complications of oligohydramnios can be fetal growth restriction and fetal malformations. In cases of severe oligohydramnios, induction of labor is warranted. Complications during labor consist of nonreassuring FHR tracings, such as variable and prolonged decelerations due to cord compression during uterine activity. Amnioinfusion may be ordered to replace fluid in the uterus to relieve umbilical cord compression during labor.[34]
Polyhydramnios
Polyhydramnios refers to elevated levels of amniotic fluid. Two common causes of polyhydramnios are maternal diabetes mellitus and fetal anomalies. Complications include premature labor, prelabor rupture of membranes, and postpartum hemorrhage because the uterine muscle is overstretched. Umbilical cord prolapse can occur if excessive fluid prevents the fetal head from descending into the maternal pelvis, allowing the umbilical cord to lie below the fetal presenting part. Treatment may include amniocentesis (to remove excess amniotic fluid) or labor induction. Placental abruption can occur after rupture of membranes due to the sudden decompression of the uterus.[35]
Chorioamnionitis
Chorioamnionitis refers to infection and inflammation of the amniotic fluid, placenta, or fetus. Chorioamnionitis is caused by bacteria present in the vagina that ascend into the amniotic area, such as Group B streptococcus. Risk factors during labor include prolonged labor, multiple vaginal exams, use of internal fetal monitors, meconium-stained fluid, and genital tract bacteria. Fetal complications are neonatal morbidity from pneumonia, meningitis, sepsis, and death. Complications in the laboring client include dysfunctional labor, postpartum atony, postpartum hemorrhage, endometritis, sepsis, and, rarely, death. Symptoms of chorioamnionitis are maternal or fetal tachycardia, uterine tenderness, foul-smelling amniotic fluid, and purulent cervical discharge. Treatment includes broad-spectrum antibiotics that are continued until after the birth. The role of the nurse is to explain the condition and purpose of the medications being administered and to monitor for signs of complications in the laboring client and fetus.[36]
Meconium-Stained Amniotic Fluid
The brown or green staining of amniotic fluid due to the fetal passage of meconium is called meconium-stained amniotic fluid (MSF). Meconium passage can be attributed to normal gastrointestinal function, fetal hypoxia, and vagal response to umbilical cord compression. Two risk factors for MSF are postterm pregnancy and fetal distress. A common complication of MSF is meconium aspiration when the fetus inhales MSF, which can cause neonatal pneumonia.
Treatment of MSF during labor consists of amnioinfusion and preparation for resuscitation. The nurse calls the neonatal intensive care unit (NICU) team to be present at the birth. The neonatal team is prepared for resuscitation if needed. If the newborn is vigorous at delivery, no suctioning is necessary. If the newborn is not vigorous, the neonatal team will initiate the steps of neonatal resuscitation, and the newborn would likely be admitted to the NICU for continued observation.
Preeclampsia
Preeclampsia is a serious disorder that occurs after 20 weeks of gestation that causes new-onset high blood pressure greater than 140/90 mm Hg and proteinuria. When caring for clients previously diagnosed with preeclampsia, the nurse monitors the laboring client’s vital signs and symptoms more frequently than those of a low-risk client. New onset elevated blood pressure during labor requires the nurse to further assess the client for other signs of preeclampsia, such as proteinuria, presence of a headache, visual disturbances, hyperreflexia, and epigastric pain. Complications during labor can be seizure, fetal distress due to uteroplacental insufficiency, and stroke. Stroke can occur when the blood pressure is critically high (i.e., 160/110 mm Hg or higher). The HELLP syndrome (hemolysis, elevated liver enzymes, and low platelet count) is a complication associated with preeclampsia that can cause life-threatening bleeding issues during labor and postpartum.[37]
Preeclampsia affects the entire body. The kidneys can be affected and cause edema in the extremities and lungs, so strict monitoring of the preeclamptic client’s intake and output (I&O) is essential. During labor, the nurse also assesses for pedal and facial edema and the lungs for signs of pulmonary edema, such as crackles, wheezes, and dyspnea.
Medical management of preeclampsia typically includes administering antihypertensive medications and magnesium sulfate; encouraging the laboring client to rest; and minimizing environmental stimuli, such as keeping the lights low; limiting visitors, and keeping the room quiet. Increases in BP are rechecked and immediately reported to the health care provider.
Read additional information about preeclampsia in the “High Blood Pressure Disorders of Pregnancy” section of the “High-Risk Perinatal Client Care” chapter.
Gestational Diabetes
Gestational diabetes is a condition causing insulin resistance and hyperglycemia during pregnancy. Clients with gestational diabetes, type 1, or type 2 diabetes mellitus have their blood glucose levels closely monitored during labor. Hourly blood glucose checks during labor are common. High energy expenditure and limited calorie intake during labor places both the client and fetus at risk for hypoglycemia. Intravenous insulin may be administered during labor and titrated to ideal glucose levels between 70 mg/dL and 110 mg/dL. Chronic maternal hyperglycemia also places the fetus at risk for hypoglycemia after delivery, so fetal blood glucose levels are closely monitored after delivery with fetal hypoglycemia protocols in place.[38]
Review fetal hypoglycemia in the “Common Complications During the Neonatal Period” section of the “Healthy Newborn Care” chapter.
Gestational diabetes is associated with complications such as prelabor rupture of membranes, induction of labor, operative vaginal delivery, cesarean birth, and shoulder dystocia. Birth injury to the fetus occurs more often in cases of gestational diabetes, especially with macrosomic infants (over 4,000 grams). Potential fetal injuries include nerve damage, fractures, and cephalohematoma. To reduce risks to the fetus and pregnant woman, induction of labor is recommended between 38- and 39-weeks’ gestation. After birth, the newborn is assessed for hypoglycemia, and the mother is encouraged to frequently breastfeed or bottlefeed.[39]
Read additional information about gestational diabetes in the “Pregestational Diabetes and Gestational Diabetes” section of the “High-Risk Perinatal Client Care” chapter.
Fetal Malpresentation
The fetal head presents in the maternal pelvis during 95 percent of labors. The most common cephalic malpresentation is the occiput posterior presentation that occurs in 15 to 30 percent of cephalic presentations. See Figure 10.55[40] for an illustration of occiput posterior presentation. Breech positions occur in 3 to 4 percent of labors.[41]
Fetal malpresentation causes difficult and prolonged labor with higher rates of cesarean section deliveries. Risk factors for fetal malpresentation are unstable fetal lie, large for gestational age, multiple gestations, polyhydramnios, contracted pelvis, pendulous abdomen, uterine anomalies, and abnormal placenta location. Abnormal fetal lie causes increased molding and caput succedaneum after birth, and neonates may have lower Apgar scores due to long, difficult labors. The nurse’s role during occiput posterior presentation is to assist the client into alternative positions such as hands-and-knees, forward-leaning, or side-lying positions to encourage rotation of the fetal occiput. If the malpresentation does not resolve, it is called a persistent occiput posterior position.

Review information about fetal presentation in the “Passenger” subsection of “The P’s of Labor” section.
Read about Apgar scoring in the “Applying the Nursing Process and Clinical Judgment Model to Newborn Care” section of the “Healthy Newborn Care” chapter.
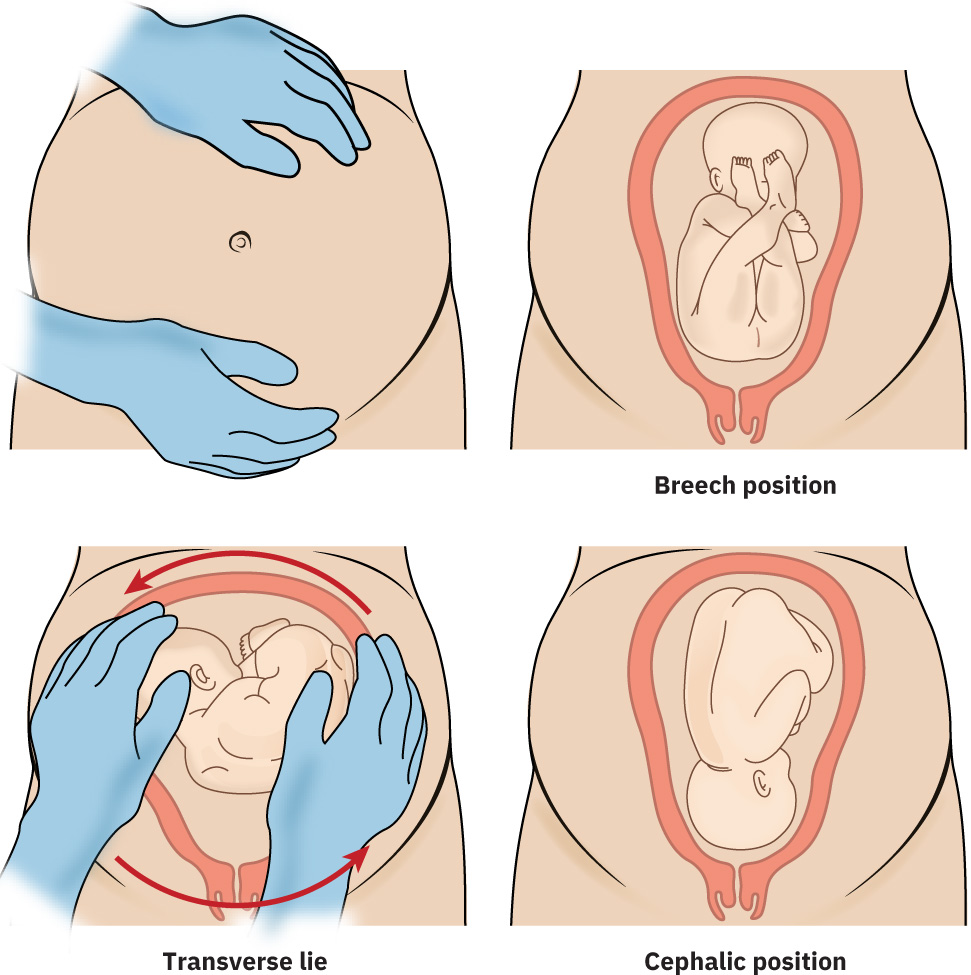
Maneuvers to Alter Fetal Lie and/or Presentation
If a fetus is in a malpresentation or non-longitudinal lie, external cephalic version (ECV) maneuvers may be attempted by the health care provider to turn the fetus into a cephalic position and promote vaginal labor. During ECV, the fetus is manipulated through the external abdominal wall in an attempt to move it into a cephalic presentation. The procedure is 58 percent successful. ECVs are more successful in multipara clients, when the presenting part is unengaged, and the placenta is posterior with normal amniotic fluid amount. An ECV is contraindicated in clients with a history of a vertical cesarean scar, multiples, oligohydramnios, uterine or fetal anomalies, nonreassuring fetal heart rate, or fetal growth restriction. After consent is signed, medications such as terbutaline or nifedipine are administered, or an epidural is placed to relax the uterus. The nurse prepares for a possible emergency cesarean birth by having the operating room ready and ensuring that staff are available for a cesarean section. After the uterus is relaxed, the health care provider attempts to lift the presenting part of the fetus and rotate the fetus into cephalic position. If the maneuver is successful, vaginal birth is attempted, but if unsuccessful, cesarean birth is performed. See Figure 10.56[42] for an illustration of EVC.[43]
Prolapsed Cord
If the umbilical cord lies beside or in front of the fetal presenting part, it is called a prolapsed cord. A prolapsed cord is considered an obstetric emergency because oxygen is unable to reach the fetus due to cord occlusion. See Figure 10.57[44] for an illustration of a prolapsed cord. A prolapsed cord is usually suspected by the nurse after rupture of the amniotic membranes, either spontaneously or artificially, when the fetal monitor tracing shows a prolonged deceleration. If a prolapsed cord is suspected, the nurse performs a vaginal exam. Many times, the umbilical cord can be palpated in the vagina with a pulsation. The nurse uses their hand to lift the presenting fetal part off the umbilical cord to promote perfusion to the fetus while calling for emergency assistance. If a cord is not palpated, the nurse lifts the presenting fetal part and evaluates the FHR tracing to determine if compression is relieved. If either of these actions relieves compression and FHR returns to normal, the nurse’s hand must remain in place, lifting the presenting fetal part, until the fetus is delivered by emergency cesarean section. However, if manually lifting the fetal presenting part does not relieve compression, the client is turned onto their hands and knees, with their head down and the buttocks lifted, until an emergency cesarean birth is performed.[45]
Fetal Distress
Fetal distress occurs when the fetus is not receiving sufficient oxygenation during labor. Uteroplacental insufficiency is the most common reason for fetal distress and can be caused by uterotonic medications causing tachysystole, maternal hypotension, prolonged umbilical cord compression, or an aged placenta. Refer to the “Fetal Heart Rate Monitoring” section for interpreting fetal monitor tracings associated with fetal distress. Fetal distress often requires immediate delivery by emergency cesarean section.
Read about cesarean section in the “Complications and Medical Interventions During the Second Stage of Labor” section.
Placenta Previa
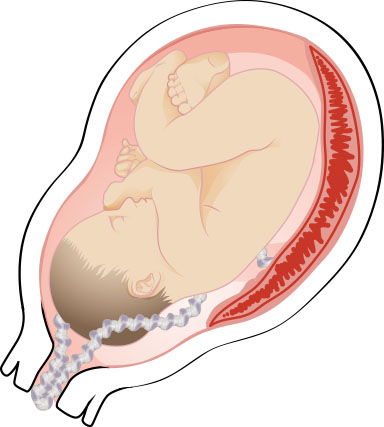
In placenta previa, the placenta is located on the lower aspect of the uterus near the internal cervical os. Risk factors for the development of a placenta previa include a history of placenta previa, multiple gestation pregnancy, multiparity, history of prior uterine surgeries (including C-sections), uterine abnormalities, advanced maternal age, use of assisted reproductive technology, and smoking. Severity ranges from the placenta lying near the internal cervical os to the placenta completely covering the os and lower uterine segment. The term low-lying placenta is often used to signify a placenta that does not entirely cover the internal os, reserving the term placenta previa for when the os is completely covered. See Figure 10.58[46] for illustrations comparing normal placental location and abnormal placental locations.
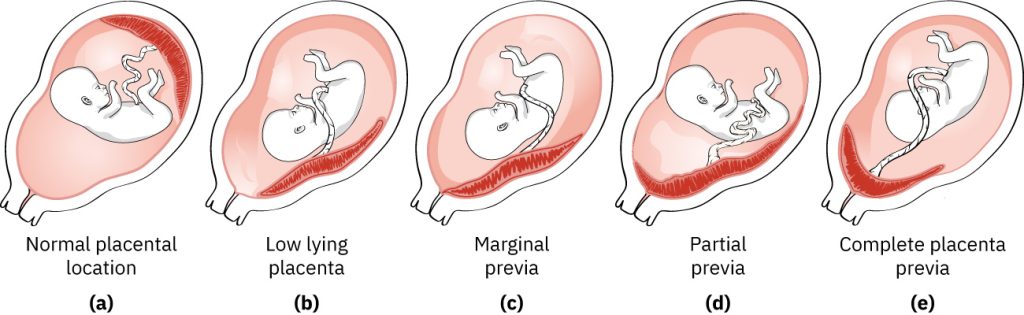
Diagnosis of placenta previa is often made during an ultrasound during the second trimester. Placenta previa can cause hemorrhage during pregnancy or labor. Signs include bright red vaginal bleeding with or without pain. Clients with placenta previa must undergo a cesarean birth because of risk of bleeding and placental tearing.[47]
Placental Abruption
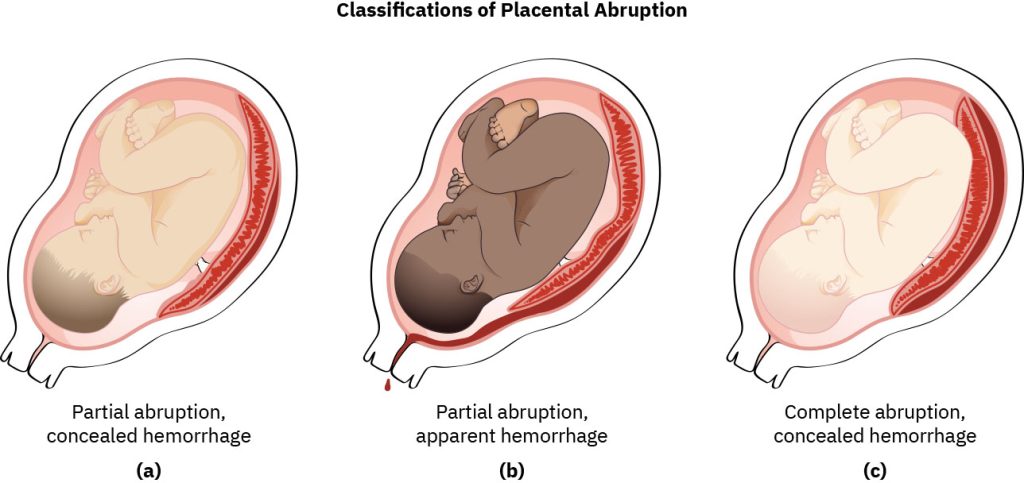
A placental abruption occurs when the placenta or part of the placenta separates from the uterine lining, which may lead to significant maternal-fetal blood loss, intrauterine fetal demise, or maternal death. Placental abruption can occur during pregnancy or labor. Risk factors for placental abruption include hypertension, smoking, cocaine use, and abdominal trauma during pregnancy. Signs of placental abruption include sudden onset of severe abdominal pain with or without dark red bleeding. Fetal heart rate monitoring may demonstrate changes in FHR and prolonged uterine contractions or a uterus that remains contracted without achieving a resting tone. Emergency cesarean section may be performed based on the severity of maternal or fetal distress. Fluid replacement and blood product transfusions, along with hemodynamic monitoring, are often required due to significant blood loss resulting in hemodynamic instability.[48] See Figure 10.59[49] for an illustration of the classifications of placental abruption that can include concealed or apparent hemorrhage.
Uterine Rupture
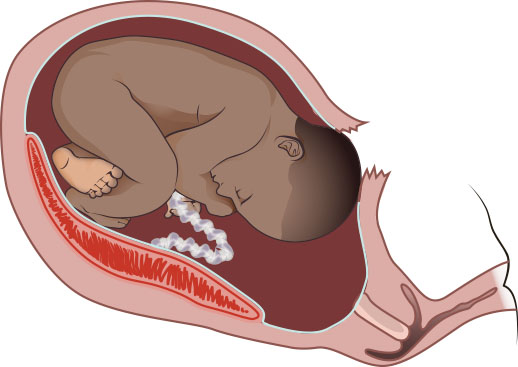
A uterine rupture refers to tearing or an opening in the muscle of the uterus. Most ruptures occur during labor, but some occur during pregnancy. See Figure 10.60[50] for an illustration of a uterine rupture. Risk factors for uterine rupture are a history of a cesarean or other uterine surgery, uterine trauma, polyhydramnios, and prolonged labor. Symptoms of a uterine rupture on electronic fetal monitoring are sudden lack of FHR and uterine contractions. Clients who do not have an epidural in place may notice a sudden lack of contractions. Other signs include late decelerations, prolonged decelerations, or severe abdominal pain. Vaginal bleeding may or may not be seen. When uterine rupture is suspected, the nurse quickly calls for assistance, prepares for an emergency cesarean birth, and prepares to order blood products because risk for postpartum hemorrhage is high. Uterine rupture is an obstetric emergency because the client can hemorrhage quickly, and the fetus can become deprived of oxygen. Emergency cesarean section is typically performed with repair of the uterus before there is an excessive loss of blood. The perinatal team will be in the operating room to provide neonatal resuscitative care due to fetal hypoxia.[51]
Amniotic Fluid Embolus
An amniotic fluid embolus, also called an anaphylactoid syndrome of pregnancy (ASP), is a rare condition that occurs when an opening develops between the amniotic sac and the client’s venous system, allowing amniotic fluid and other fetal tissue to enter the maternal cardiovascular and respiratory systems. This complication may occur during the rupture of membranes or other times during labor and delivery. Symptoms include respiratory distress, cyanosis, hypotension, and seizure. Many clients go into cardiac arrest and require intubation and ventilator support, and the majority develop disseminated intravascular coagulation (DIC). The mortality rate associated with ASP is 60 to 80 percent.[52]
View a supplementary YouTube video[53] about amniotic fluid embolus: Amniotic Fluid Embolism (AFE) | Nursing Care of the Childbearing Family.
Read additional information in the “Amniotic Fluid Embolism” section of the “High-Risk Perinatal Client Care” chapter.
Disseminated Intravascular Coagulation
Disseminated intravascular coagulation (DIC) is a rare and potentially fatal condition that can occur during pregnancy and the four stages of labor. DIC affects the coagulation cascade with the release of all clotting and anti-clotting factors, leading to massive hemorrhage and organ failure. It can be caused by preeclampsia, placental abruption, amniotic fluid embolism, fetal demise, and sepsis. Medical treatment is based on treating the cause and also includes blood product transfusions and possible intubation and mechanical ventilation.[54]
Intrauterine Fetal Demise
Intrauterine fetal demise (IUFD), commonly called stillbirth, occurs in 1 in 160 births. It is typically caused by fetal hypoxia but the cause can be unknown. Fetal hypoxia may occur due to prolonged labor; placental insufficiency; postterm pregnancy; placental infarcts; placental abruption; umbilical cord accidents such as knots, loops, or prolapse; and fetal malpresentation. A history of prior stillbirth greatly increases the risk of repeat stillbirth. Other factors such as nulliparity, advanced maternal age, obesity, preexisting diabetes, chronic hypertension, multiple gestation, smoking, and use of alcohol during pregnancy have been associated with IUFD. Autopsy and DNA testing can be performed with parental consent to determine the cause of fetal death in hopes of preventing another demise. The role of the nurse is to encourage the client, partner, and other family members to hold the infant and take pictures to keep as memories of the infant. The nurse plays a significant role in emotionally supporting the client, partner, and family. IUFD can also be emotionally difficult for nurses, and many labor and delivery units have support groups, social workers, or counselors that help the nurse, as well as train nurses in assisting with perinatal bereavement.[55]
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- “ed99ff8ca641a308a7c68f13fe2bec8df29e8bd8” by Rice University/OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- The American College of Obstetricians and Gynecologists. (2024). First and second stage labor management. Clinical practice guideline Number 8. https://www.acog.org/clinical/clinical-guidance/clinical-practice-guideline/articles/2024/01/first-and-second-stage-labor-management ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- “d57cecd3a05beab4a5a46ada350f730aff7ac536” by Rice University/OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/maternal-newborn-nursing/pages/19-1-labor-dystocia ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- “53a91face67cae19504767744ef91af79200d94e” by Rice University/OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/maternal-newborn-nursing/pages/19-1-labor-dystocia ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- “df1630199d31eb2d9d9b1460442d44cce3eb2a2e” by Rice University/OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/maternal-newborn-nursing/pages/19-1-labor-dystocia ↵
- “c34aeb22d76862174d515ade9326e996d5d438e0” by Rice University/OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/maternal-newborn-nursing/pages/19-1-labor-dystocia ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- “1bab953701f9121cab305fcd6ed5570bd42cc12c” by Rice University/OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/maternal-newborn-nursing/pages/19-1-labor-dystocia ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- “1bab953701f9121cab305fcd6ed5570bd42cc12c” by Rice University/OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/maternal-newborn-nursing/pages/16-2-external-and-internal-monitoring ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- “83ba8826d32ac94cbab04bcf7568058541ca326c” by Rice University/OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/maternal-newborn-nursing/pages/19-3-obstetrical-conditions-affecting-labor-and-birth ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- “4b8c18fdcda4bd8b3b39fa4537a42f5da467bf8d” by Rice University/OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/maternal-newborn-nursing/pages/15-1-factors-influencing-the-process-of-labor-and-birth#fig-00007 ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- “2811fdd58c50cb68f886b4037bbf4e4aa42ea613” by Rice University/OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/maternal-newborn-nursing/pages/19-7-obstetrical-emergencies ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- “aa79236cd245e3339a87b19710cf8e55371fcdf1” by Rice University/OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/maternal-newborn-nursing/pages/12-2-conditions-limited-to-pregnancy ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- “4363e28718e1f1f94d6239bbc3a93a7e3ba50c0b” by Rice University/OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/maternal-newborn-nursing/pages/12-2-conditions-limited-to-pregnancy ↵
- “e3ef1d779d7613f0798bac81dc6868c6303f0806” by Rice University/OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/maternal-newborn-nursing/pages/19-7-obstetrical-emergencies ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Lecturio Nursing. (2023, June 13). Amniotic fluid embolism (AFE) | Nursing care of the childbearing family [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=vyWWjN1xYc0 ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal-newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
Labor occurring from 20 weeks gestation to 36 6/7 weeks gestation.
Too much amniotic fluid.
Refers to rupture of amniotic membranes prior to the 37th completed week of gestation and before spontaneous labor.
Drugs used to delay preterm labor by suppressing uterine contractions.
Too little amniotic fluid.
Infection of the amniotic membranes.
When the estimated weight of the fetus is less than the 10th percentile for gestational age.
Stimulation of uterine contractions prior to the spontaneous onset of labor.
A tool used to determine if the cervix is favorable for labor.
The softening and opening of the cervix as it prepares for labor.
The most commonly used medication for labor induction.
Medications that promote uterine contractions.
A surgical procedure to remove uterine fibroids while preserving the uterus. It is often recommended for women who wish to maintain fertility.
No progression in cervical dilation in clients who are at least 6 cm dilated with rupture of membranes despite 4 hours of adequate uterine activity, or 6 hours of inadequate uterine activity with oxytocin augmentation.
Defined as more than 3 hours of pushing in nulliparous individuals and 2 hours of pushing in multiparous individuals.
Uterine contractions or the maternal pushing effort is inadequate to cause cervical changes that progress to birth.
A problem of the passage, meaning that the pelvic outlet does not allow the passage of the fetus for birth.
A problem of the passenger, meaning that the fetus is unable to descend through the maternal pelvis for birth.
At least five previous births at a gestational age of at least 20 weeks.
Edema of the scalp that occurs due to pressure exerted on the head during delivery.
The process of stimulating the uterus to increase the frequency, duration, and intensity of contractions after the onset of spontaneous labor contractions.
The artificial rupture of the membranes (AROM) by a midwife or obstetrician using an amniotic hook.
Labor and delivery that is extremely rapid, usually less than three hours from start of the contractions to birth.
Brown or green staining of amniotic fluid due to the fetal passage of meconium.
When the fetus inhales MSF.
New onset of hуреrtеnѕion (blood pressure greater than 140/90) and рrotеinuriа, or new onset of hуреrtеsion plus significant end-organ dysfunction with or without рroteinuriа, in a previously normotensive pregnant client.
A complication associated with preeclampsia that can cause life-threatening bleeding issues during labor and postpartum evidenced by hemolysis, elevated liver enzymes, and low platelet count.
A condition causing insulin resistance and hyperglycemia during pregnancy.
The fetus is manipulated through the external abdominal wall in an attempt to move it into a cephalic presentation.
The umbilical cord lies beside or in front of the fetal presenting part.
When the fetus is not receiving sufficient oxygenation during labor.
The placenta is attached in the lower part of the uterus and covers the cervix.
Separation of the placenta from the uterine wall before delivery that can cause life-threatening complications such as postpartum hemorrhage and fetal hypoxia.
Tearing or an opening in the muscle of the uterus.
A rare condition that occurs when an opening develops between the amniotic sac and the client’s venous system, allowing amniotic fluid and other fetal tissue to enter the maternal cardiovascular and respiratory systems.
A rare and potentially fatal condition that can occur during pregnancy and the four stages of labor affecting the coagulation cascade with the release of all clotting and anticlotting factors leading to massive hemorrhage and organ failure.
Stillbirth commonly caused by fetal hypoxia.

