9.6 Prenatal Care and Reducing Maternal Mortality
Barriers to Prenatal Care
Initiation of early and frequent prenatal care promotes positive pregnancy outcomes for the mother and the baby. However, several social determinants of health can create barriers for women to receive prenatal care such as financial resources, geographic location, and access to health care providers. One would think that pregnancy and childbirth would be safer than ever due to recent advances in medical care, but this is not the case in the United States. Over the past 30 years, the maternal mortality rate in the U.S. has doubled with approximately 700 women dying each year as a result of pregnancy or its complications. Maternal mortality rate is defined as death while pregnant or within 42 days of the end of pregnancy, irrespective of the duration and site of the pregnancy, from any cause related to or aggravated by the pregnancy or its management, but not from accidental or incidental causes. This rate is reported as a ratio per 100,000 births. See Table 9.6 for a comparison of maternal mortality rates across several developed countries with the United States having the highest rate.[1]
Table 9.6. Comparison of Maternal Mortality Rates for Developed Countries[2]
| Country | Maternal Mortality Ratio (per 100,000 live births) |
|---|---|
| New Zealand | 1.7 |
| Norway | 1.8 |
| Netherlands | 3.0 |
| Germany | 3.2 |
| Sweden | 4.3 |
| Switzerland | 4.6 |
| Australia | 4.8 |
| United Kingdom | 6.5 |
| Canada | 8.6 |
| France | 8.7 |
| United States | 17.4 |
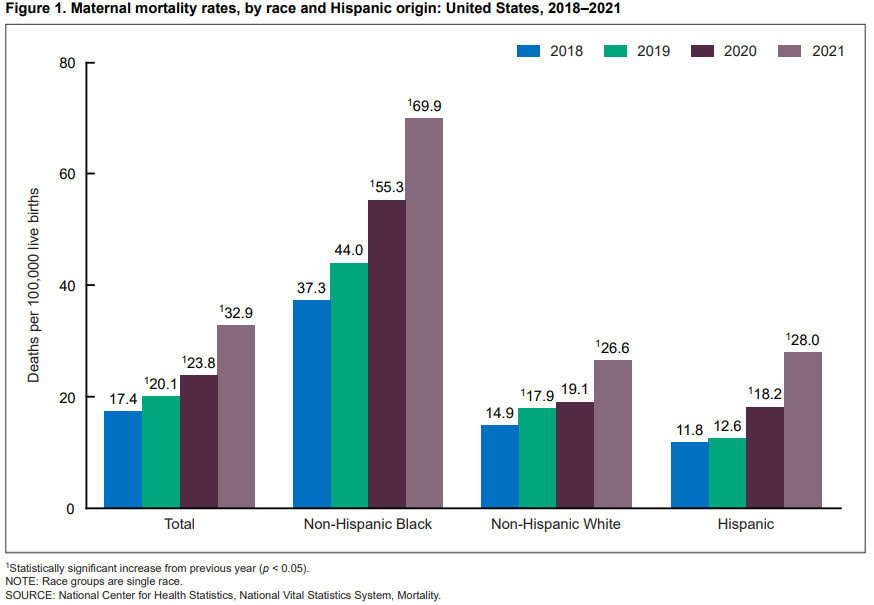
Women of color and American Indian/Alaska Native women suffer worse pregnancy outcomes than White women in the United States. For example, in 2018, Black women were three to four times more likely to die during pregnancy, childbirth, or the postpartum period, regardless of income or education level. American Indian/Alaska Native women were two to three times more likely to die. The reasons for these disparities are complex with reasons rooted outside and inside the health care system.[3] See Figure 9.15[4] for a comparison of maternal mortality rates across cultures in the U.S.
In 2023 the March of Dimes report titled Where You Live Matters: Maternity Care Deserts and the Crisis of Access and Equity shows more than 36% of U.S. counties are considered maternity care deserts, defined as counties without a hospital or birth center offering obstetric care and without any obstetric providers. More than 5.6 million women live in U.S. counties with no or limited access to maternity care services. Furthermore, 8 out of 10 maternity care deserts have high numbers of pregnant women with preexisting chronic health conditions like hypertension, diabetes, obesity, and smoking that further impact pregnancy and birth outcomes.[5]
Common Pregnancy and Childbirth Complications
Maternal mortality is caused by complications that occur during and following pregnancy and childbirth. Most of these complications are preventable or treatable. Other complications are caused by preexisting health conditions that exist before pregnancy but are worsened during pregnancy, especially if not managed as part of the woman’s prenatal care. Complications that account for nearly 75% of maternal deaths include the following[6]:
- Severe bleeding (mostly after childbirth)
- Infections (usually after childbirth)
- High blood pressure during pregnancy (i.e., preeclampsia and eclampsia)
- Complications from delivery
- Unsafe abortion
Severe bleeding after birth can kill a healthy woman within hours if she is untreated. Oxytocin intravenous infusions immediately after childbirth effectively reduce the risk of bleeding. Infection after childbirth can be eliminated if good hygiene is practiced and if early signs of infection are recognized and treated in a timely manner. It is important that high blood pressure is detected and appropriately managed before the onset of convulsions (eclampsia) and other life-threatening complications. Administering medications such as magnesium sulfate for preeclampsia can lower a woman’s risk of developing eclampsia. All births should be attended by skilled health professionals because timely medical treatment can prevent deaths of the mother and the newborn if complications occur during delivery. Unintended pregnancies can be prevented through effective contraceptive use by women and adolescents and help prevent maternal mortality from unsafe abortions. All pregnant women need access to high-quality prenatal care, as well as care during and after childbirth, to prevent maternal and newborn mortality.[7]
Improving Maternal Mortality Rates in the United States
In 2020 the Surgeon General’s Call to Action to Improve Maternal Health report suggested lowering the maternal mortality rate could be achieved with the following actions[8]:
- Recognizing the need to address mental and physical health across the life span, starting with young girls and adolescents and extending through the childbearing age.
- Supporting healthy behaviors that improve women’s health, such as breastfeeding, smoking cessation, and physical activity.
- Recognizing and addressing factors that are associated with overall health and well-being, including those related to social determinants of health.
- Understanding that maternal health disparities exist in the United States, including geographic, racial, and ethnic disparities, and work to address them.
- Acknowledging that maternal age and chronic conditions such as hypertension, obesity, and diabetes are risk factors for poor maternal health.
- Learning about early “warning signs” of potential health issues that can occur at any time during pregnancy or in the year after delivery.
- Working collaboratively to recognize the unique needs of women with disabilities and include this population of women in existing efforts to reduce maternal health disparities.
Nurses can help decrease maternal mortality by providing health teaching to clients regarding these suggestions to identify risk factors and prevent complications to the extent possible.
Hear Her Campaign
The Hear Her campaign is an initiative launched by the Centers for Disease Control and Prevention (CDC) with the aim of raising awareness about pregnancy-related complications and promoting timely recognition and response to warning signs during and after pregnancy. The primary goal of the Hear Her campaign is to reduce maternal mortality and severe maternal morbidity by encouraging women, their families, and health care providers to listen to women’s concerns, take them seriously, and take appropriate action when warning signs arise. The campaign emphasizes the importance of recognizing warning signs and symptoms of pregnancy-related complications such as preeclampsia, postpartum hemorrhage, blood clots, infection, and other conditions that can lead to severe maternal outcomes. It encourages women to trust their instincts and speak up if they feel that something is not right with their health or their pregnancy.[9]
Routine Prenatal Care
Routine prenatal care begins at the first prenatal visit and continues throughout the 40 weeks of pregnancy. The purposes of prenatal care are to gather assessment data at each prenatal visit, to analyze the data to ensure there are no factors placing the fetus or pregnant woman at risk for complications, to implement interventions if risk factors or complications are identified, and to promote positive mother and fetal outcomes. Registered nurses are part of the prenatal health care team in county public health departments, community health centers and clinics, and private practices and implement nursing interventions based on the nurse’s assessment of the family.[10] Licensed practical nurses also provide prenatal care at clinics under the direction of registered nurses and health care providers.
The 40 weeks of pregnancy are divided into three periods called trimesters. Each trimester is 14 weeks of gestation. The first trimester is from the first day of the woman’s last menstrual period to 13 weeks and six days of gestation, the second trimester is from gestational 14 to 27 weeks and six days of gestation, and the third trimester is from 28 weeks’ gestation until 40 weeks and 6 days. Clients are encouraged to schedule their first prenatal visit sometime between 8 and 12 weeks of gestation.[11],[12]
The first prenatal visit typically occurs during the first trimester, depending upon when the client realizes she is pregnant. During the first prenatal visit, a comprehensive health history, physical exam, and diagnostic tests are performed. Until approximately 28 weeks, the pregnant woman will have monthly visits. After approximately 36 weeks, prenatal visits will be weekly until delivery. The first prenatal visit, second trimester visits, and third trimester visits are further discussed in the remaining sections of this chapter.
View a supplementary YouTube video[13] on antepartum care: Topic 10: Antepartum Care.
- Tikkanen, R., Gunja, M., FitzGerald, M., & Zephyrin, L. (2020). Maternal mortality and maternity care in the United States compared to 10 other developed countries. Commonwealth Fund. https://doi.org/10.26099/411v-9255 ↵
- Tikkanen, R., Gunja, M., FitzGerald, M., & Zephyrin, L. (2020). Maternal mortality and maternity care in the United States compared to 10 other developed countries. Commonwealth Fund. https://doi.org/10.26099/411v-9255 ↵
- Hoyert, D. L. (2023). Maternal mortality rates in the United States, 2021. Centers for Disease Control and Prevention. https://dx.doi.org/10.15620/cdc:124678 ↵
- Hoyert, D. L. (2023). Maternal mortality rates in the United States, 2021. Centers for Disease Control and Prevention. https://dx.doi.org/10.15620/cdc:124678 ↵
- March of Dimes. (2023). New March of Dimes research shows access to maternity care worsening for millions of women in the U.S. https://www.marchofdimes.org/about/news/new-march-dimes-research-shows-access-to-maternity-care-worsening-millions-women-us ↵
- World Health Organization. (2024). Maternal mortality. https://www.who.int/news-room/fact-sheets/detail/maternal-mortality ↵
- World Health Organization. (2024). Maternal mortality. https://www.who.int/news-room/fact-sheets/detail/maternal-mortality ↵
- Office of the Surgeon General. (2020). Strategies and actions: Improving maternal health and reducing maternal mortality and morbidity. The Surgeon General’s Call to Action to Improve Maternal Health [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK568218/ ↵
- Centers for Disease Control and Prevention. (2024). Hear Her campaign. https://www.cdc.gov/hearher/index.html ↵
- Giles, A., Prusinski, R., & Wallace, L. (2024). Maternal newborn nursing. OpenStax. https://openstax.org/books/maternal-newborn-nursing/pages/1-introduction ↵
- Centers for Disease Control and Prevention. (2024). Hear Her campaign. https://www.cdc.gov/hearher/index.html ↵
- American College of Obstetricians and Gynecologists. (2024). How your fetus grows during pregnancy. https://www.acog.org/womens-health/faqs/how-your-fetus-grows-during-pregnancy ↵
- Association of Professors of Gynecology and Obstetrics (APGO). (2015, September 3). Topic 10: Antepartum care [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=JM7oqjqtA8o&t=2s ↵
Death while pregnant or within 42 days of the end of pregnancy, irrespective of the duration and site of the pregnancy, from any cause related to or aggravated by the pregnancy or its management, but not from accidental or incidental causes.
Counties without a hospital or birth center offering obstetric care and without any obstetric providers.
An initiative launched by the Centers for Disease Control and Prevention (CDC) with the aim of raising awareness about pregnancy-related complications and promoting timely recognition and response to warning signs during and after pregnancy.
0 to 13 weeks and six days of gestation.
14 to 27 weeks and six days of gestation.
28 weeks until delivery.

