16.14 Nasolacrimal Duct Obstruction
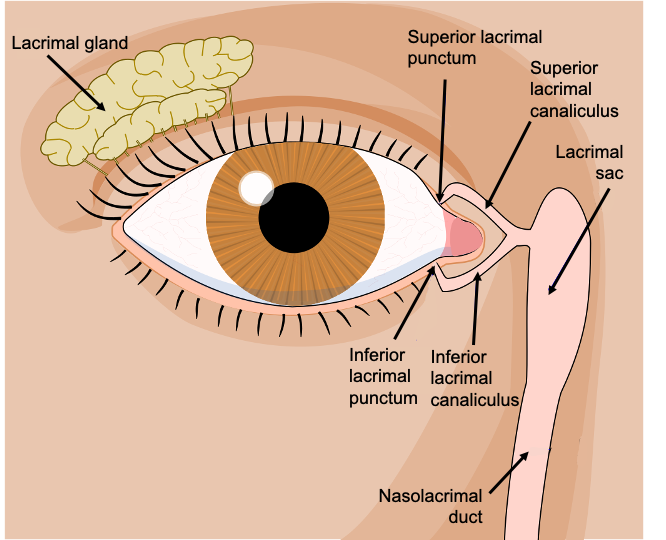
Nasolacrimal duct obstruction (NLDO), also known as dacryostenosis, is a common condition affecting up to 20% of newborn clients. It occurs due to a lack of patency or narrowing of the nasolacrimal duct that causes excessive eye watering and usually resolves spontaneously. See Figure 16.20[1] for an image depicting the nasolacrimal duct and associated structures. Although this is usually a congenital disorder, it can also be acquired later in life due to inflammation, trauma, or infections. Genetics may play a role in the development of this disorder, and other risk factors include premature birth, birth by cesarean section, Down syndrome, and maternal substance abuse.[2],[3]
When NLDO remains untreated, potential complications can result. Some potential complications of this disorder are recurrent conjunctivitis, infection of the lacrimal sac, orbital cellulitis, sepsis, meningitis, or brain abscess. Around 10% of pediatric clients with NLDO also develop visual acuity issues and/or amblyopia (lazy eye).[4]
Pathophysiology
During embryonic development, the nasolacrimal apparatus begins to form between the third and fifth week. Canalization, or the development of a canal in which tears can drain from the eye to the nose, starts in the third month of development and is usually complete by the eighth month. However, when delays or abnormalities in development occur, obstruction of the nasolacrimal duct can result. Usually, this obstruction occurs in the distal part of the nasolacrimal duct.[5]
Assessment (Recognize Cues)
Physical Exam
The most common presenting symptom of NLDO is epiphora (i.e., excessive eye watering). Eye watering may increase when the infant has nasal congestion or is exposed to wind or cold weather. Mucus-like discharge is also commonly seen.[6]
Common Laboratory and Diagnostic Tests
NLDO is a clinical diagnosis, but a variety of testing techniques are available to support this diagnosis, including the following[7]:
- Fluorescein dye disappearance test involves dye being placed into the eyes. In a client without NLDO, this dye will drain into the nose. However, in clients with NLDO, a large amount of dye will remain in the eye after five minutes.
- Dacryocystography consists of injecting a contrast dye into the lacrimal system and then using imaging to find the area of obstruction.
- Traditional imaging, such as CT scans, ultrasound, or MRI, can also be used to evaluate the nasolacrimal apparatus.
Diagnosis (Analyze Cues)
Nursing priorities for clients with nasolacrimal duct obstruction include symptom management and prevention of complications. Nursing diagnoses for clients with nasolacrimal duct obstruction are created based on the specific needs of the client, their signs and symptoms, and the etiology of the disorder. These nursing diagnoses guide the creation of client-specific care plans that encompass client outcomes and nursing interventions, as well the evaluation of those outcomes. These individualized care plans then serve as a guide for client treatment. Possible nursing diagnoses for clients with nasolacrimal duct obstruction include the following:
- Altered sensory perception r/t disease process
- Risk for injury r/t disease progression
Outcome Identification (Generate Solutions)
Outcome identification encompasses the creation of short- and long-term goals for the client. These goals are used to create expected outcome statements that are based on the specific needs of the client. Expected outcomes should be specific, measurable, achievable, relevant and timebound (SMART) within a set time frame based on the application of appropriate nursing interventions. Sample expected outcomes for clients with NLDO include the following:
- The client will exhibit a reduction in eye watering and discharge by ten months of age.
- The client will remain free from signs of infection.
Implementation (Take Action)
Medical Interventions
The majority of cases of congenital NLDO can be managed conservatively by massaging the lacrimal duct two to three times a day and applying prophylactic antibiotic ointment. If symptoms persist beyond six to ten months of age, the client should be referred to an ophthalmologist for further care. For persistent NLDO, surgical options are available such as the following[8]:
- Lacrimal duct probing with insertion of a cannula into the duct and progressing through the obstructed area.
- Nasolacrimal intubation that combines duct probing with the placement of a stent in the nasolacrimal duct.
- Balloon dacryoplasty that uses a balloon to dilate the obstructed area and then a stent is put in place.
Potential complications of surgical procedures are nasolacrimal duct scarring and infection.[9]
Nursing Interventions
Registered nurses develop interventions based on the expected outcomes of the client. Prior to implementation, the nurse must determine if all previously planned interventions are still suitable based on the current situation of the client. When caring for a client with nasolacrimal duct obstruction, nursing interventions can be divided into nursing assessments, nursing actions, and client teaching, as described in the following subsections.[10],[11]
Nursing Assessments
- Assess the client for the presence of pain, eye erythema, purulent drainage, or headache, as these symptoms could signify an infection or other complication.
Nursing Actions
- Reassure caregivers that most cases of NSLO resolve with lacrimal duct massage by the time the client is 12 months of age.
- Encourage caregivers to clean the infant’s eyes with a warm washcloth to wipe away excessive drainage.
Client Teaching
- Teach caregivers the proper technique for nasolacrimal duct massage. This technique can be viewed using the information in the following box.
View a supplementary YouTube video[12] on nasolacrimal duct massage: Ask-a-Doc | How to Clear a Babies Tear Duct | Cooks Children’s.
Review general nursing interventions related to caring for an ill child in the “Planning Care for the Ill Child” chapter.
Evaluation (Evaluate Outcomes)
Evaluation of client outcomes refers to the process of determining whether or not client outcomes were met by the indicated time frame. This is done by reevaluating the client as a whole and determining if their outcomes have been met, partially met, or not met. If the client outcomes were not met in their entirety, the care plan should be revised and reimplemented. Evaluation of outcomes should occur each time the nurse assesses the client, examines new laboratory or diagnostic data, or interacts with another member of the client’s interdisciplinary team.
- “51174745058_5d3c7e8311_o” by ASCCC OERI is licensed under CC BY-SA 2.0 ↵
- Perez, Y., Patel, B. C., & Mendez, M. D. (2023). Nasolacrimal duct obstruction. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK532873/ ↵
- Pezzoli, M., Zeppieri, M., & Patel, B. C. (2024). Dacryostenosis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK563132 ↵
- Pezzoli, M., Zeppieri, M., & Patel, B. C. (2024). Dacryostenosis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK563132 ↵
- Pezzoli, M., Zeppieri, M., & Patel, B. C. (2024). Dacryostenosis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK563132 ↵
- Pezzoli, M., Zeppieri, M., & Patel, B. C. (2024). Dacryostenosis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK563132 ↵
- Pezzoli, M., Zeppieri, M., & Patel, B. C. (2024). Dacryostenosis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK563132 ↵
- Pezzoli, M., Zeppieri, M., & Patel, B. C. (2024). Dacryostenosis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK563132 ↵
- Pezzoli, M., Zeppieri, M., & Patel, B. C. (2024). Dacryostenosis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK563132 ↵
- Perez, Y., Patel, B. C., & Mendez, M. D. (2023). Nasolacrimal duct obstruction. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK532873/ ↵
- Pezzoli, M., Zeppieri, M., & Patel, B. C. (2024). Dacryostenosis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK563132 ↵
- Cook Children’s Health Care System. (2017, February 9). Ask-a-doc | How to clear a babies tear duct | Cooks children’s [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=aPXlJgZSDbA ↵
A common condition affecting up to 20% of newborn clients. It occurs due to a lack of patency or narrowing of the nasolacrimal duct that causes excessive eye watering and usually resolves spontaneously; also known as dacryostenosis.
An obstruction of the nasolacrimal duct.
A lazy or wandering eye.
Excessive eye watering.
Injecting a contrast dye into the lacrimal system and then using imaging to find the area of obstruction.

