2.8 Applying the Nursing Process and Clinical Judgment Model to Promoting Healthy Lifestyles
Nursing Process
The nursing process is a critical thinking model based on a systematic approach to client-centered care. Nurses use the nursing process to perform clinical reasoning and make clinical judgments when providing patient care. As discussed in Chapter 1, the nursing process is based on the Standards of Professional Nursing Practice established by the American Nurses Association (ANA). These standards are authoritative statements of the actions and behaviors that all nurses, regardless of role, population, specialty, and setting, are expected to perform competently. The mnemonic ADOPIE is an easy way to remember the ANA Standards and the nursing process. Each letter refers to the six components of the nursing process: Assessment, Diagnosis, Outcomes Identification, Planning, Implementation, and Evaluation.[1]
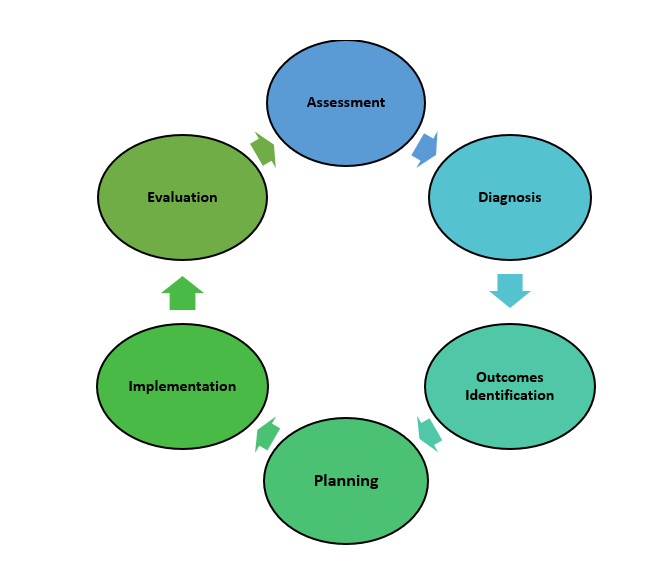
The nursing process is a continuous, cyclic process that is constantly adapting to the client’s current health status. See Figure 2.13[2] for an illustration of the nursing process.
NCSBN Clinical Judgment Model
A second critical thinking model is the National Council of State Boards of Nursing (NCSBN) Clinical Judgment Measurement Model (NCJMM) used on the National Council Licensure Examination (NCLEX). The NCLEX is the exam that all nursing graduates must successfully pass to obtain their nursing license and become a nurse. Graduates take the NCLEX-PN to receive their Practical/Vocational Nurse license and the NCLEX-RN to receive their Registered Nurse license. The purpose of the NCLEX is to evaluate if a nursing graduate (i.e., candidate) is competent to provide safe, competent, entry-level nursing care.[3]
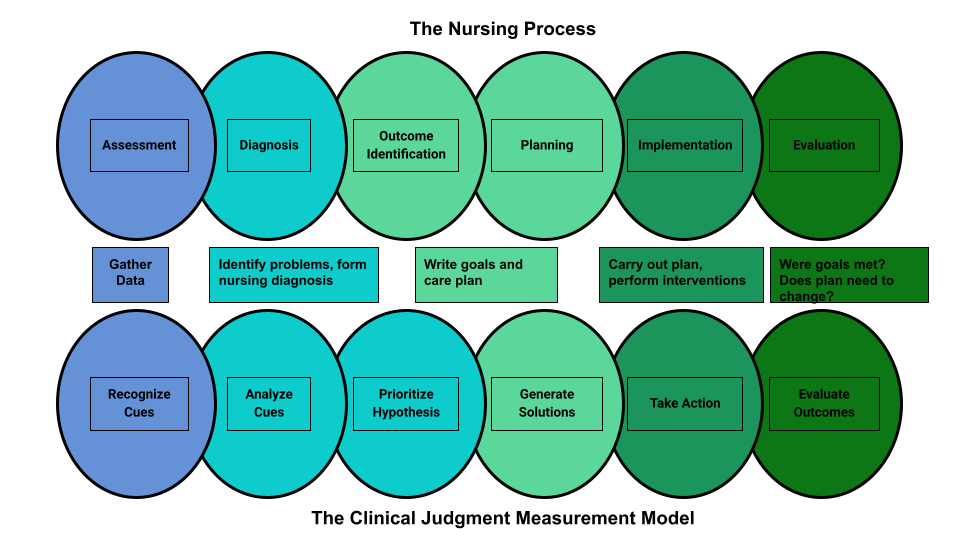
A new edition of the NCLEX was released in 2023 that includes “Next Generation” questions. The Next Generation NCLEX (NGN) uses evolving case studies and other types of test questions based on the new NCSBN Clinical Judgment Measurement Model (NCJMM) to evaluate how well a candidate can think critically and use clinical judgment when providing safe nursing care. The NCJMM complements the nursing process but uses different terminology in exam questions while assessing the candidate’s clinical judgment. This terminology includes recognize cues, analyze cues, prioritize hypotheses, generate solutions, take actions, and evaluate outcomes. See Table 2.8a for a comparison of the clinical judgment model and the nursing process.
Table 2.8a. NCSBN Clinical Judgment Model and the Nursing Process[4],[5]
| NCSBN Clinical Judgment Skill | Description | Corresponding Stage of the Nursing Process |
|---|---|---|
| Recognize Cues | What data is clinically significant?
Determining what client findings are significant, most important, and of immediate concern to the nurse (i.e., identifying “relevant cues”). |
Assessment |
| Analyze Cues | What does the data mean?
Analyzing data to determine if it is “expected” or “unexpected” or “normal” or “abnormal” for this client at this time according to their age, development, and clinical status. Making a clinical judgment concerning the client’s “human response to health conditions/life processes, or a vulnerability for that response”; also referred to as “forming a hypothesis.” |
Diagnosis
(Analysis of Data) |
| Prioritize Hypotheses | What hypotheses should receive priority attention?
Ranking client conditions and problems according to urgency, complexity, and time. |
Planning |
| Generate Solutions | What should be done?
Planning individualized interventions that meet the desired outcomes for the client; may include gathering additional assessment data. |
Outcome Identification and Planning |
| Take Action | What will I do now?
Implementing interventions that are safe and most appropriate for the client’s current priority conditions and problems. |
Implementation |
| Evaluate Outcomes | Did the interventions work?
Comparing actual client outcomes with desired client outcomes to determine effectiveness of care and making appropriate revisions to the nursing care plan. |
Evaluation |
View Figure 2.14[6] for an illustration comparing the nursing process and the NCSBN Clinical Judgment Measurement Model.
Read more about the NCSBN Clinical Judgment Model and the Next Generation NCLEX at the Clinical Judgment Measurement Model web page.
The following subsections will describe how a nurse uses the nursing process and the clinical judgment model to promote healthy lifestyle behaviors. Stages of the National Council of State Board of Nursing (NCSBN) Clinical Judgment Model are indicated in parentheses.
Assessment (Recognize Cues)
Nurses assess a client’s current lifestyle behaviors to develop a plan for promoting healthy lifestyle choices that reduce modifiable risk factors for disease and injury. Assessment can take many forms, including physical assessment, observation, interviewing, and the use of reliable assessment tools.
Subjective Data
Clients can provide lifestyle-related information in response to questions posed by the nurse. Below are examples of questions and prompts the nurse may ask to gain better insights into a client’s current behaviors:
- Do you smoke? If so, how much?
- Share your typical daily dietary intake.
- Describe your current physical activity level.
- How much alcohol do you consume on a daily/weekly/monthly basis?
- How would you describe your current mental health?
- How many hours of sleep do you get a night?
- Do you feel rested when you wake up in the morning?
- Describe your sleep hygiene habits.
- Are you up-to-date with your vaccinations?
- Are you up-to-date with your recommended health screenings?
Objective Data
During the physical assessment, the nurse can gather measurable data that provides information relevant to a healthy lifestyle:
- Weight
- Height
- BMI
- Waist circumference
- Vital signs (blood pressure, heart rate, respiratory rate, pulse oximetry)
- Pain
FANTASTIC Lifestyle Assessment Questionnaire
The FANTASTIC Lifestyle Assessment Questionnaire (FLAQ) is a tool that was developed in 1983 to evaluate the lifestyle behaviors of individuals to determine how they might affect an individual’s health. The tool can be used to assess a variety of factors related to a healthy lifestyle. The acronym “FANTASTIC” is used for the nine dimensions that are addressed in the assessment, including Family and friends, Activity, Nutrition, Tobacco and toxins, Alcohol and other substances, Sleep and stress, Type of personality, Introspection, and Control of health. For each dimension, clients are asked to describe their behavior. For example, for the family and friends dimension, clients rate if they have someone to talk to about important things, ranging from “almost never” to “almost always.” In a similar manner, they are asked to rate their ability to sleep well and feeling rested from “almost never” to “almost always.” Based on the answers to the 25 questions, a score is calculated that categorizes clients on a range from excellent lifestyle to needing improvement. The tool allows the provider and the client to identify areas in which improvements can be made and then work together to develop a plan to change those behaviors.[7]
Diagnosis (Analyze Cues)
After collecting assessment data, the nurse identifies risk factors, unhealthy behaviors, and areas of opportunity to change behavior and reduce risk. The nurse selects appropriate nursing diagnoses from a current care-planning resource based on the client’s specific needs. In addition to the nursing diagnoses of Deficient Knowledge and Readiness for Enhanced Knowledge discussed in the “Teaching and Learning” chapter, Table 2.8b summarizes additional NANDA nursing diagnoses related to teaching about healthy lifestyles.
Table 2.8b. NANDA Nursing Diagnoses Related to Teaching About Healthy Lifestyles[9]
| Nursing Diagnosis | Definition | Selected Defining Characteristics |
|---|---|---|
| Ineffective health maintenance behaviors | Management of health knowledge, attitudes, and practices underlying health actions that are unsatisfactory for maintaining or improving well-being or preventing illness and injury. |
|
| Ineffective health self-management | Unsatisfactory handling of symptoms, treatment regimen, and lifestyle changes associated with living with a chronic condition. |
|
| Readiness for enhanced health self-management | Pattern of handling symptoms, treatment regimen, consequences and lifestyle changes inherent in living with a chronic condition, which can be strengthened. | Desires to enhance:
|
| Readiness for enhanced exercise engagement | Pattern of attention to physical activity characterized by planned, structured, repetitive body movements, which can be strengthened. | Desires to enhance:
|
| Readiness for enhanced sleep pattern | Pattern of natural, periodic suspension of relative consciousness which can be strengthened. |
|
Outcome Identification (Generate Solutions)
Nurses collaboratively set goals and identify outcome criteria with clients based on their values, cultural beliefs, and preferences. An overall goal related to health maintenance is, “The client will effectively maintain their health.”
SMART outcome criteria need to be specific, measurable, achievable, realistic, and time oriented. Sample SMART outcome criteria related to promoting healthy lifestyles are as follows:
- The client will participate in moderate intensity exercise for 150 minutes every week within one month.
- The client will achieve a BMI between 18.5 and 24.9 within six months.
Planning (Generate Solutions)
Interventions are collaboratively selected with clients to help them achieve their identified goals and outcome criteria. Providing health teaching and emotional support are the main nursing actions when assisting clients in making behavior change.
For example, when helping clients achieve their goals to increase physical activity, sample planned nursing interventions may include the following:
- The nurse will help the client identify perceived and actual barriers to participating in regular exercise.
- The nurse will teach the client how to calculate their optimal heart rate.
- The nurse will teach the client how to assess their pulse during exercise.
- The nurse will teach the client how exercise is part of a weight management program.
Implementation (Take Action)
During the implementation stage, the nurse considers if the planned teaching topics are still safe and appropriate based on the client’s current priority conditions and problems. For example, if the client is currently experiencing symptoms of intermittent dizziness, suggested exercises may be modified to be in a seated position to reduce the risk of falls.
Evaluation (Evaluate Outcomes)
During the evaluation phase, the nurse compares actual client outcomes with the previously established SMART outcomes to determine the effectiveness of the interventions. If the SMART outcomes are not met by the established timelines, the nurse makes appropriate revisions to the nursing care plan.
For example, the nurse evaluates the client’s progress toward the previously established SMART outcome, “Within one month, the client will participate in moderate intensity exercise for 150 minutes every week.” If the client has not met this outcome, the nurse assesses potential barriers with the client for meeting this goal and then revises the health teaching or outcome as indicated.
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- “The Nursing Process” by Kim Ernstmeyer at Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- National Council of State Boards of Nursing. (2024). NCLEX. https://www.ncsbn.org/nclex.htm ↵
- NCSBN. (n.d.). NCSBN clinical judgment measurement model. https://www.ncsbn.org/14798.htm ↵
- Ignativicius, V., & Silvestri, L. (2022). Preparing for the Next-Generation NCLEX (NGN): A “how-to” step-by-step faculty resource manual. Elsevier. [PDF]. https://evolve.elsevier.com/education/wp-content/uploads/sites/2/NGN_FacultyGuide_Final.pdf ↵
- “Nursing Process and NCJMM” by Tami Davis is licensed under CC BY 4.0 ↵
- Batista, P., Neves-Amado, J., Pereira, A., & Amado, J. (2023). FANTASTIC lifestyle questionnaire from 1983 until 2022: A review. Health Promotion Perspectives, 13(2), 88-98. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10439457/ ↵
- Pedley, L. (n.d.). Fantastic lifestyle checklist. Integral Coaching. [PDF]. https://cpb-ca-c1.wpmucdn.com/myriverside.sd43.bc.ca/dist/6/45/files/2014/01/Fantastic-Lifestyle-Checklist-Fillable-1smptgc.pdf ↵
- Herdman, T. H., Kamitsuru, S., & Lopes, C. T. (Eds.). (2024). Nursing diagnoses: Definitions and classification, 2024-2026 (13th ed.). Thieme. ↵
A critical thinking model based on a systematic approach to client-centered care.
Mnemonic reflecting an easy way to remember the ANA Standards and the nursing process.

