8.10 Female Reproductive System Disorders
Abnormal Vaginal Bleeding
Abnormal vaginal bleeding refers to very heavy menstrual flow during menses, bleeding between menstrual cycles, or menses that lasts more than seven days. It also refers to bleeding that happens before puberty or after menopause. Very heavy bleeding during menses and/or bleeding that lasts more than seven days is called menorrhagia. For example, women with menorrhagia may bleed enough to soak through one or more tampons or sanitary pads every hour.[1]
Hormone imbalance is a common cause of abnormal bleeding referred to as dysfunctional uterine bleeding. Dysfunctional uterine bleeding commonly occurs in teenagers or women approaching menopause or the absence of menstruation when an egg is not released from the ovaries as it should (anovulation). Anovulation is a common condition for teenagers who recently started their menstrual cycles, as well as for women approaching menopause. When anovulation occurs, extended estrogen release causes the endometrial lining of the uterus to continue to grow until it gets too thick. When this thickened lining is shed during menstruation, it causes the bleeding to be very heavy. A hormonal imbalance can also cause the body not to know when to shed the lining, causing irregular bleeding or “spotting” between periods.[2]
Abnormal vaginal bleeding can also be caused by uterine fibroids (benign growths in the uterus), conditions related to pregnancy, and cancer of the uterus or cervix. Diagnostic testing includes pelvic ultrasounds and procedures such as endometrial biopsy or hysteroscopy. Treatment is based on the cause of the abnormal bleeding and may include medications, dilation and curettage (D&C), endometrial ablation, or hysterectomy. Endometrial ablation is a procedure that destroys the endometrial lining of the uterus to reduce or stop heavy menstrual bleeding. Medications and medication-secreting devices used to treat dysfunctional uterine bleeding are birth control pills and intrauterine devices (IUDs).[3]
Bacterial Vaginosis
Bacterial vaginosis (BV) is a condition in female clients where normal Lactobacillus flora of the vagina is replaced by multiple anaerobic species of bacteria. Clients can be asymptomatic or have increased vaginal discharge with a fishy smell. They are also at higher risk for STI. Risk factors for BV include multiple, new, or female sex partners; douching; menstruation; copper-containing IUDs; herpes simplex 2; and lack of condom use. Male circumcision and hormonal contraception may reduce the incidence of BV in females.[4]
Treatment of BV with metronidazole or clindamycin helps decrease symptoms and infection. Women should refrain from sex or use condoms during treatment. Female clients should avoid douching because it does not relieve symptoms and may contribute to BV relapse. Treatment of male partners is not effective in decreasing recurrence in females.[5]
Cancer
Common cancers affecting the female reproductive system include breast, cervical, ovarian, and endometrial.
Breast Cancer
Breast cancer occurs when breast cells mutate and become cancerous cells that multiply and form tumors. There are different kinds of breast cancer, depending on which cells in the breast turn into cancer. Most breast cancers begin in the ducts (called invasive ductal carcinoma) or lobules (called invasive lobular carcinoma). There are also other kinds of breast cancer. Breast cancer can spread outside the breast to other parts of the body through blood and lymph vessels. When breast cancer spreads to other parts of the body, it is said to have metastasized.[6]
People of both genders who have a strong family history of breast cancer or inherited changes in BRCA1 and BRCA2 genes have a high risk of getting breast cancer. See Figure 8.30[7] for an illustration of signs of breast cancer. Warning signs of breast cancer include the following[8]:
- New lump in the breast or armpit.
- Thickening or swelling of part of the breast.
- Irritation or dimpling of breast skin.
- Redness or flaky skin in the nipple area or the breast.
- Pulling in of the nipple or pain in the nipple area.
- Nipple discharge other than breast milk, including blood.
- Any change in the size or the shape of the breast.
- Pain in any area of the breast.

The American Cancer Society recommends a mammogram every year for most women starting at age 45.[9] A mammogram is a radiographic image of breast tissue that can detect signs of cancer, often before a lump is felt. People suspected of having breast cancer or those at high risk may have additional diagnostic tests, such as the following[10]:
- Breast ultrasound: A breast ultrasound uses sound waves to make images, called sonograms, of areas inside the breast.
- Diagnostic mammogram: If an area of the breast looks abnormal on a screening mammogram, a diagnostic mammogram is performed to get a more detailed X-ray of the breast.
- Breast magnetic resonance imaging (MRI): A breast MRI is a kind of body scan that uses a magnet linked to a computer. The MRI scan makes detailed pictures of areas inside the breast.
- Biopsy: Tissue, fluid, and/or lymph nodes are removed by a health care provider and sent to a laboratory to be examined under a microscope. There are different kinds of biopsies, such as a fine-needle aspiration, sentinel lymph node biopsy, core biopsy, or open biopsy.
Breast cancer is treated in several ways, depending on the type of breast cancer and if it has spread in the body. People with breast cancer often receive more than one kind of treatment. Treatments may include the following[11]:
- Surgery: There are different types of surgery, depending on how far the cancer has spread in the breasts, lymph nodes, and surrounding tissue.
- Breast-conserving surgery: Breast-conserving surgery removes the cancer and some normal tissue around it, but not the breast itself. This type of surgery may also be called lumpectomy, partial mastectomy, segmental mastectomy, quadrantectomy, or breast-sparing surgery.
- Total mastectomy: Total mastectomy removes the breast that has cancer and some of the lymph nodes in the armpit. This procedure is also called a simple mastectomy.
- Modified radical mastectomy: The whole breast that has cancer and most of the lymph nodes surrounding the breast are removed.
- Chemotherapy: Specific medications are prescribed by physicians to shrink or kill specific types of cancer cells. Chemotherapy may be given as pills or administered intravenously, depending on the type of medication prescribed.
- Hormonal therapy: Special medications are used to block cancer cells from getting the hormones they need to grow.
- Targeted therapy: Targeted therapy works with the body’s immune system to help it fight cancer cells or to control side effects from other cancer treatments.
- Radiation therapy: Radiation therapy uses high-energy rays (similar to X-rays) to kill the cancer cells.
Doctors from different specialties often work together to treat breast cancer. Surgeons perform operations. Medical oncologists are physicians who specialize in the treatment of cancer with medication. Radiation oncologists are physicians who specialize in the treatments of cancer with radiation.
Cervical Cancer
Cervical cancer is mostly caused by the human papillomavirus (HPV). HPV is passed from one person to another during sexual contact. HPV causes cervical cells to change into abnormal cells (called dysplasia), which over time can become cancer. Cervical cancer is highly curable when found and treated early. Early cervical cancer does not cause symptoms, so routine PAP smears are recommended to screen for cancer. Most women between the ages of 21 and 65 should have a PAP smear every three to five years, depending upon their risk factors.[12]
The Papanicolaou smear, commonly referred to as a PAP smear, is a cytological study that screens for cancer in the cervix before symptoms even occur. During a PAP smear, a health care provider inserts a speculum into the client’s vagina to allow visualization of the cervix and obtains samples of cervical cells for laboratory analysis. An HPV test is also typically performed during a PAP smear to check for infection with high-risk types of HPV that cause cancer.[13]
There are several types of abnormal cells that may be found on PAP smears. For example, low-grade squamous intraepithelial lesions (LSIL) refer to slightly abnormal changes that are usually caused by an HPV infection that require additional diagnostic testing. High-grade squamous intraepithelial lesions (HSIL) refer to abnormal cervical cells that could become cancer if not treated. Adenocarcinoma in situ means an advanced lesion (i.e., area of abnormal tissue) was found in the tissue of the cervix and requires a biopsy.[14]
Additional diagnostic testing, such as a colposcopy, is performed for abnormal cell changes on PAP smears. A colposcopy is a procedure in which a lighted, magnifying instrument called a colposcope is used to visually examine the cervix and potentially remove tissue for biopsy.[15]
Treatment for cervical cancers often includes excisional or ablative treatments[16]:
- Cold knife conization: A scalpel or laser knife is used to remove a cone-shaped section of abnormal tissue in the cervix. This procedure is done at the hospital and requires general anesthesia.
- Loop electrosurgical excision procedure (LEEP): Electrical current is passed through a thin wire loop to remove abnormal tissue in the cervix. Local anesthesia is used to numb the area, so this procedure can be performed in the health care provider’s office.
- Cryotherapy: A special cold probe is used to destroy abnormal tissue by freezing it. This procedure is done in the health care provider’s office. It takes only a few minutes and usually does not require anesthesia.
- Laser therapy: A laser (narrow beam of intense light) is used to destroy abnormal tissue. This procedure is done at the hospital, and general anesthesia is used.
Endometrial Cancer
The most common type of uterine cancer is endometrial cancer. A common symptom of endometrial cancer is postmenopausal vaginal bleeding.[17]
Diagnostic testing for endometrial cancer includes a transvaginal ultrasound and endometrial sampling. Endometrial sampling is the removal of tissue from the endometrium by a health care provider who inserts a brush, curette, or thin, flexible tube through the cervix and into the uterus. The tool is used to gently scrape a small amount of tissue from the endometrium and then remove the tissue samples. A pathologist views the tissue under a microscope to look for cancer cells. Alternatively, dilation and curettage (D&C) or hysteroscopy may be performed.[18]
If endometrial cancer is diagnosed, additional diagnostic tests are performed to see if the cancer has spread to other parts of the body, including chest X-rays, CT scans, MRIs, and PET scans. Treatment for endometrial cancer may include surgery, such as a hysterectomy, bilateral oophorectomy, and lymph node dissection. A lymph node dissection is a surgical procedure in which the lymph nodes are removed from the pelvic area, and a sample of tissue is examined under a microscope by a pathologist for signs of metastatic cancer. This procedure is also called lymphadenectomy. Other treatments include radiation therapy, chemotherapy, hormone therapy, and targeted therapy.[19]
Ovarian Cancer
Ovarian cancer is cancer that grows in the tissues of the ovary. Ovarian cancer has few symptoms other than possible pain and/or swelling in the pelvic area, so it often metastasizes before it is diagnosed. Some types of ovarian cancer are caused by mutations in genes called BRCA1 or BRCA2, so women who have a family history of ovarian cancer are at an increased risk. Other types of ovarian cancer are caused by metastatic cancer from other sites, such as breast, cervical, or colon cancer. Some women who have an increased risk of ovarian cancer may choose to have an oophorectomy to remove healthy ovaries as a preventative measure.[20]
Diagnostic tests for ovarian cancer include blood tests, a transvaginal ultrasound, or CT scans. After ovarian cancer has been diagnosed, additional diagnostic tests, such as an MRI or PET scans, are done to determine if cancer cells have spread within the ovaries or to other parts of the body. Treatment may include surgery, such as a hysterectomy, salpingo-oophorectomy, or omentectomy. An omentectomy is removal of tissue in the peritoneum that contains blood vessels, nerves, lymph vessels, and lymph nodes. The peritoneum is the tissue that lines the abdominal wall and covers most of the organs in the abdomen. Additional treatments may include chemotherapy, targeted therapy, radiation therapy, and immunotherapy.[21]
Endometriosis
Endometriosis is a chronic disease in which tissue similar to the lining of the uterus (endometrium) grows outside the uterus, causing chronic inflammation and scarring. Scarring can cause adhesions and fibrosis within the pelvis and other parts of the body such as the bladder and bowel. See Figure 8.31[22] for an illustration of endometriosis. Endometriosis can start during a female’s first menstrual period and last until menopause. The cause of endometriosis is unknown, and there is no way to prevent or cure it.[23]
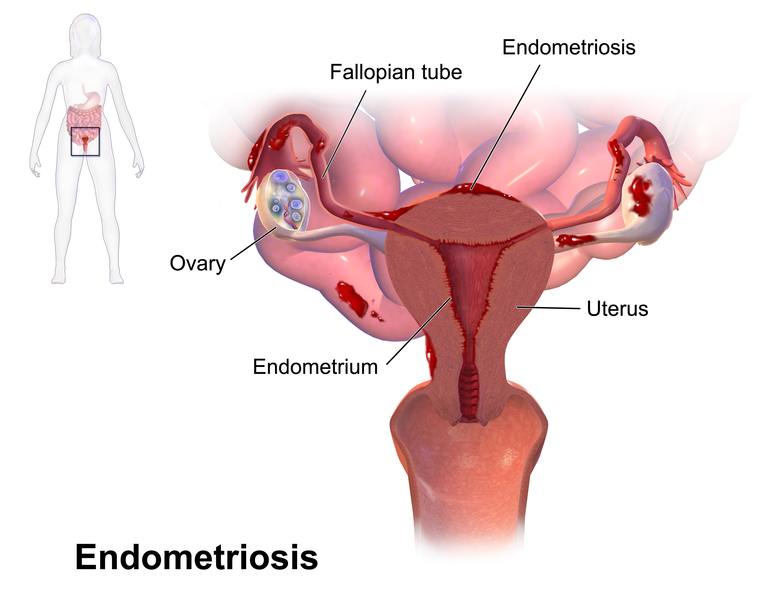
Symptoms of endometriosis include severe pain during periods, sexual intercourse, bowel movements, and urination, as well as chronic pelvic pain. Some clients have heavy bleeding during or between periods. Additional symptoms include abdominal bloating, nausea, fatigue, depression, anxiety, and infertility. Because symptoms are varied, it may be difficult for a client to be diagnosed with endometriosis. Endometriosis can affect quality of life due to pain, fatigue, depression, and infertility. Endometriosis may be diagnosed using ultrasound, MRI, laparoscopy, or surgery.[24]
Treatment focuses on symptom control and may include the following[25]:
- Non-steroidal anti-inflammatory drugs (NSAIDs) for pain and inflammation
- Contraceptives and hormonal GnRH-analogues
- Surgery to remove endometriosis lesions, scar tissue, and adhesions
Nurses can encourage clients with symptoms of endometriosis to seek medical treatment. Clients may also find it helpful to attend support groups for emotional health as they cope with this chronic, painful disease.
Ovarian Cyst
An ovarian cyst is a fluid-filled sac in the ovary. The two most common types of ovarian cysts are follicle cysts and corpus luteum cysts. In a normal menstrual cycle, an ovary releases an ovum (egg) each month. The ovum grows inside a tiny sac called a follicle that breaks open to release the egg. Follicle cysts form when the follicle doesn’t break open to release the egg, causing it to continue growing into a cyst. Follicle cysts often have no symptoms and typically resolve in one to three months.
During normal ovulation, after the follicle breaks open and releases the egg, the empty follicle sac shrinks into a mass of cells called a corpus luteum. Corpus luteum cysts form if the empty follicle sac doesn’t shrink as it should but instead reseals itself and builds up with fluid. Most corpus luteum cysts go away after a few weeks, but they can grow to ten centimeters (four inches) wide and cause pain. They may also bleed or cause the ovary to twist, requiring surgery such as a laparoscopy or a laparotomy[26]:
- Laparoscopy: During this surgery, the physician makes a very small incision above or below the umbilicus (navel) and inserts instruments with a camera to look inside the pelvic area and remove the cyst, which is then sent to a pathology lab for analysis. This type of surgery is typically performed for smaller cysts that appear benign (i.e., not cancerous) on the ultrasound.
- Laparotomy: A laparotomy is typically performed for large cysts or those that are suspicious on ultrasound as cancerous. This surgery uses a larger incision in the abdomen to remove the cyst, and then the cyst is sent to a pathology lab for analysis.
Pelvic Inflammatory Disease
Pelvic inflammatory disease (PID) is a spectrum of inflammatory disorders of a female client’s reproductive system, including endometritis (inflammation of the inner lining of the uterus), salpingitis (inflammation of the Fallopian tubes), tubo-ovarian abscess (collection of pus in the Fallopian tubes and/or ovaries), and/or pelvic peritonitis (inflammation of the tissues lining the lower abdomen and organs). PID may be caused by organisms such as those that cause gonorrhea, chlamydia, bacterial vaginosis, and others. Additional risk factors are placement of an IUD, especially in the first three weeks after insertion, having multiple sex partners or a sex partner who has multiple sex partners, being sexually active prior to age 25, and douching. Having PID puts a client at risk for developing it again.[27],[28]
Clients can prevent PID by avoiding intercourse or using a condom correctly each time to prevent STIs or being mutually monogamous with a sex partner. This means each person in the sexual relationship has sex only with that one partner. Symptoms of PID range from none to lower abdominal pain; fever greater than 101 degrees Fahrenheit; foul-smelling unusual vaginal discharge; pain and/or bleeding with intercourse or between periods; and burning with urination. PID can be difficult to diagnose due to vague and limited symptoms. No single lab, historical, or physical finding accurately diagnoses PID, but most clients with PID have mucopurulent cervical drainage and WBCs in vaginal fluid. Therefore, diagnosis is based mainly on symptoms. Because PID may be missed, it is better to initiate antimicrobial medication in cases of PID to prevent adverse effects than to miss a case.[29],[30]
Clients with PID experience the most optimal outcomes when they begin treatment early. While STIs and PID can be treated with antibiotics, this may not undo any damage to the reproductive system that occurred prior to treatment. If sexually active and younger than 25, clients should be tested yearly for chlamydia and gonorrhea and treated for STIs to prevent progression to PID. Nurses should teach clients and their partners to finish the full antibiotic course prescribed for PID, even if symptoms are relieved. Clients and partners should abstain from intercourse until antibiotics are finished, and they are free from symptoms to prevent reinfection. An IUD does not need to be removed if a client experiences PID unless they show no clinical improvement by 72 hours of initiating treatment. Research of non-hormonal IUDs has not shown any PID benefit of removing an IUD.[31],[32]
Treatment of PID is important due to potential serious complications, such as scar tissue that can block Fallopian tubes and increased risk for ectopic pregnancy. Ectopic pregnancy occurs when a fertilized egg implants outside the uterus. An ectopic pregnancy is not viable and puts the mother at risk of Fallopian tube rupture and subsequent hemorrhage. Clients with PID are also at risk for infertility and long-term pelvic and abdominal pain.[33],[34]
Polycystic Ovary Syndrome
Polycystic ovary syndrome (PCOS) is a condition characterized by hormone imbalances, ovulatory dysfunction, and multiple ovarian cysts (i.e., small sacs of fluid). Fluid-filled cysts containing immature eggs are called follicles. Instead of releasing an egg during ovulation, the follicles (cysts) build up and enlarge. See Figure 8.32[35] for an illustration of PCOS.
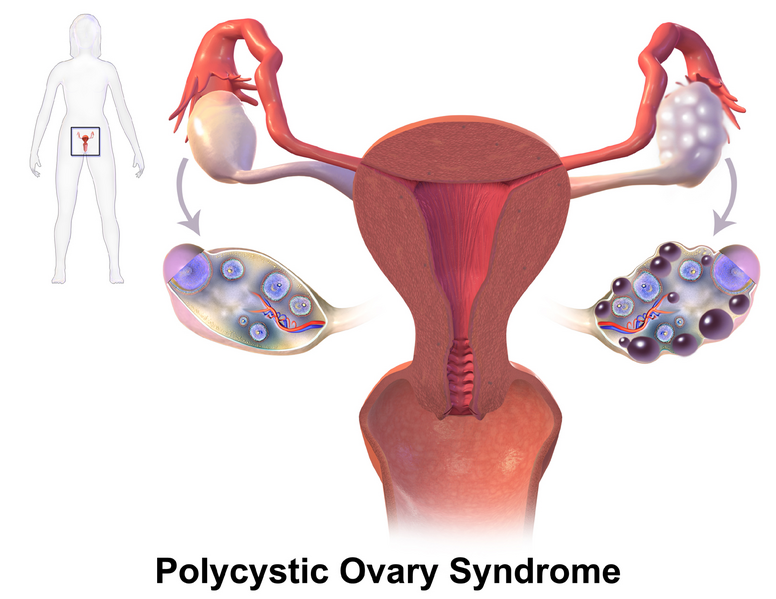
PCOS has no known cause, but it is associated with obesity and excessive insulin production. Common symptoms of PCOS include oligomenorrhea, amenorrhea, polymenorrhea, and enlarged ovaries due to multiple cysts or follicles. High levels of androgen hormones associated with PCOS can cause hirsutism or excess facial and body hair. PCOS can also cause infertility.[36]
PCOS is diagnosed with blood tests and a transvaginal ultrasound. Treatments for PCOS include birth control pills to control menstrual cycles, diabetes medications to reduce insulin resistance, and medication to promote ovulation.
Premenstrual Syndrome
Premenstrual syndrome (PMS) is a collection of physical and emotional symptoms that occur in female clients in one to two weeks prior to menstruation. This is due to falling estrogen and progesterone hormone levels between ovulation and menses that begin to rise again at the start of a period. To be classified as PMS, symptoms need to occur at this time of the menstrual cycle. Severity of symptoms in clients can range from little to none, up to debilitating enough to miss school or work. Those at highest risk of PMS have high stress, a history of depression or postpartum depression, or a family history of depression. PMS is likely to increase in the ages of the 30s-40s and during perimenopause, and end with menopause, due to hormonal changes.[37],[38]
Physical symptoms of PMS may include the following[39],[40]:
- Swollen or tender breasts
- Constipation or diarrhea
- Bloating or a gassy feeling
- Pelvic cramping
- Headache or backache
- Clumsiness
- Lower tolerance for noise or light
- Acne
- Weight gain
Emotional or mental symptoms of PMS may include the following[41],[42]:
- Irritability or hostile behavior
- Feeling tired
- Sleep problems (sleeping too much or too little)
- Appetite changes or food cravings
- Trouble with concentration or memory
- Tension or anxiety
- Depression, feelings of sadness, or crying spells
- Mood swings
- Less interest in sex
PMS is diagnosed based on the timing of symptoms that occur between five days prior to and four days after the start of a period for at least three cycles in a row that interfere with enjoying daily life. PMS can exacerbate health problems that have some symptom overlap such as depression, anxiety, irritable bowel syndrome, bladder pain syndrome, and myalgic encephalomyelitis/chronic fatigue syndrome. PMS may also worsen asthma, allergies, and migraines.[43],[44]
PMS treatments can be pharmacologic and nonpharmacologic. To relieve or prevent symptoms, nurses can encourage clients to do the following[45],[46]:
- Participate in aerobic exercise most days
- Eat a healthy diet by limiting sugar, salt, alcohol, and caffeine in the two weeks prior to a period
- Get adequate sleep (approximately eight hours per night)
- Use positive coping strategies and stress management techniques, such as meditation or yoga
- Stop smoking
Pharmacologic interventions for PMS include the following[47],[48]:
- Over-the-counter pain relievers for cramps, headaches, backaches, or breast tenderness such as naproxen, ibuprofen, or aspirin.
- Hormonal birth control may help PMS symptoms but make other symptoms worse.
- Antidepressants or antianxiety medications for emotional symptoms.
- Diuretics for breast tenderness and bloating.
- Calcium for fatigue, cravings, and depression.
- Vitamin B6 for moodiness, irritability, forgetfulness, bloating, and anxiety.
- Magnesium has had mixed results in research. It may help with premenstrual migraines.
- Polyunsaturated fatty acids (omega-3 and omega-6) may help reduce cramps and other symptoms.
- Herbal supplements of black cohosh, chasteberry, and evening primrose oil have shown mixed results for effectiveness. Clients should review herbal supplements with their provider.
Premenstrual Dysphoric Disorder
Premenstrual dysphoric disorder (PMDD) is a disorder that affects about 5% of menstruating females. It has similar symptoms as premenstrual syndrome (PMS) but is more serious. PMDD causes severe irritability, depression, or anxiety in the week or two before the menstrual cycle, and these issues go away two to three days after menstruation starts. Symptoms can include the following[49]:
- Lasting irritability or anger that may affect other people
- Feelings of sadness or despair, or even thoughts of suicide
- Feelings of tension or anxiety
- Panic attacks
- Mood swings or crying often
- Lack of interest in daily activities and relationships
- Trouble thinking or focusing
- Tiredness or low energy
- Food cravings or binge eating
- Trouble sleeping
- Feeling out of control
- Physical symptoms, such as cramps, bloating, breast tenderness, headaches, and joint or muscle pain
Women with PMDD require medications and other treatments such as the following[50]:
- Antidepressants called selective serotonin reuptake inhibitors (SSRIs) that increase serotonin levels in the brain
- Birth control pills to help regulate hormone levels
- Over-the-counter pain relievers, such as ibuprofen, naproxen, or aspirin, to help relieve physical symptoms
- Stress management and relaxation techniques
- Healthy lifestyle changes, such as healthy food choices across the food groups, cutting back on salty and sugary foods, and getting more physical activity
Prolapse
A prolapse is the displacement of an organ or anatomic structure from its normal position. A uterine prolapse is the downward displacement of the uterus into the vagina. A uterine prolapse occurs when the pelvic floor muscles and ligaments stretch and weaken until they no longer provide enough support for the uterus. As a result, the uterus slips down into or protrudes out of the vagina. Uterine prolapse most often affects people after menopause who have had one or more vaginal deliveries. Surgery may be required to treat the prolapse.[51]
An anterior vaginal prolapse, also known as a cystocele or a protrusion of the bladder, is when the bladder drops from its usual position in the pelvis into the vagina. Anterior vaginal prolapse occurs when the pelvic floor becomes weak or if too much pressure is put on the pelvic floor. This can happen over time, during vaginal childbirth, or with chronic constipation, violent coughing, or heavy lifting. Surgery may be required to treat the prolapse.[52]
A posterior vaginal prolapse, also known as a rectocele or rectal prolapse, is when the rectum protrudes into the vagina.
Toxic Shock Syndrome (TSS)
Toxic shock syndrome (TSS) can be caused by toxin-producing Staphylococcus aureus or Group A Streptococcus pyogenes and is associated with super-absorbency tampon or menstrual cup use. Symptoms typically have sudden onset and include fever, hypotension, sunburn-like rash, and end-organ damage. Prodromal symptoms of malaise, chills, myalgias, headache, pharyngitis, and nausea/vomiting may precede sepsis and organ dysfunction. A macular rash occurs followed by full thickness peeling in one to two weeks. The client may also have a strawberry tongue, vaginal mucosa alterations, and disorientation.[53] See Figure 8.33[54] for an image of a strawberry tongue.
![]“PCOS_%28Part_2%29.png” by BruceBlaus is licensed under CC BY 4.0 Photo showing a person with a strawberry tongue](https://wtcs.pressbooks.pub/app/uploads/sites/48/2024/10/Strawberry__Tonue-614x1024.jpg)
Nurses can provide the following health teaching to help prevent TSS[55],[56]:
- Wash hands prior to touching tampons, menstrual cups, diaphragms, and contraceptive caps, and do not leave them in longer than recommended.
- Change tampons every four hours.
- Use the lightest absorbency tampon possible.
- Only use super-absorbency tampons when menstrual flow is heavy.
- Alternate between tampons and pads.
Uterine Fibroid
A uterine fibroid is a benign tumor in the muscular wall of the uterus in women. See Figure 8.34[57] for an illustration of fibroids.
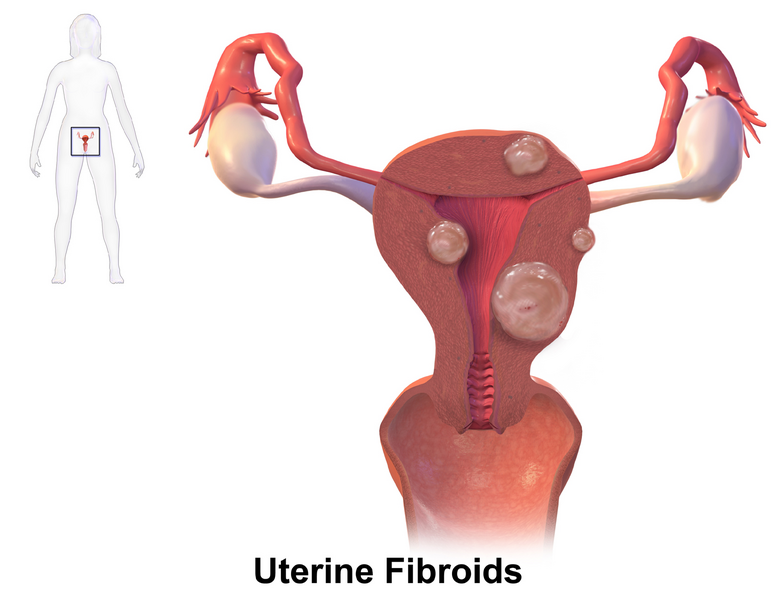
The cause of fibroids is unknown. Symptoms of uterine fibroids are as follows[58]:
- Dysmenorrhea
- Menorrhagia
- Metrorrhagia
- A feeling of fullness in the lower abdomen
- Frequent urination
- Dyspareunia
- Lower back pain
- Reproductive problems, such as infertility, multiple miscarriages, or early labor
Symptomatic uterine fibroids may be treated with birth control pills or medications to shrink the fibroids. For women with fibroids with moderate or severe symptoms, several types of surgery may be used to treat them[59]:
- Myomectomy: Surgery that removes fibroids without taking out healthy tissue of the uterus. This surgery is best for women who wish to have children after treatment. It can be major surgery (involving cutting into the abdomen) or performed with laparoscopy or hysteroscopy.
- Hysterectomy: Surgery to remove the uterus when fibroids are large, if the woman is experiencing very heavy bleeding, or if the woman is near menopause or does not want future pregnancy.
- Endometrial ablation: The lining of the uterus is removed or destroyed to control very heavy bleeding. This can be done using several methods such as a laser, wire loops, electric current, microwaves, freezing, and other methods. This procedure usually is considered minor surgery and can be done on an outpatient basis or in a doctor’s office. A woman cannot have future pregnancies after this procedure.
- Myolysis: A needle is inserted into the fibroids, guided by laparoscopy, and electric current or freezing is used to destroy the fibroids.
- Uterine fibroid embolization (UFE) or uterine artery embolization (UAE): A thin tube is threaded into the blood vessels that supply blood to the fibroid, and then tiny plastic particles are injected into the blood vessels to block the blood supply to the fibroid. The lack of blood supply causes the fibroid to shrink.
Vulvovaginal Candidiasis
Vulvovaginal candidiasis (VVC) is a common fungal infection caused by Candida albicans that causes pruritus, vaginal soreness, dyspareunia, dysuria, redness, and abnormal curd-like vaginal discharge. Uncomplicated VVC and is diagnosed based on signs and symptoms and/or a culture of the vaginal discharge that shows yeast.[60]
Treatment for VVC includes antifungal medications administered orally or as a vaginal cream or suppository. Nurses should teach clients that antifungal creams and suppositories can weaken latex condoms or diaphragms. If VVC occurs during pregnancy, clients should only use topical antifungal medications because oral medication is associated with spontaneous abortion and congenital anomalies. If clients self-treat with over-the-counter medications but symptoms do not improve or recur within two months, they should see a health care provider because the symptoms may be caused by an alternative problem.[61]
VVC is not an STI, and research indicates no benefit in treating sexual partners. However, some male sexual partners may have symptoms of balanitis such as erythema, irritation, and penile pruritus. They can also use topical antifungal medication to relieve these symptoms.[62]
Female clients can benefit from knowing what actions help and/or irritate the vulvovaginal area. See Table 8.10 for activities to promote and avoid to promote vulvovaginal health.
Table 8.10. Teaching Topics to Promote Vulvovaginal Health[63]
| Teaching Topics | Rationale |
|---|---|
| Wipe from front to back. | Prevents anal bacteria from infecting vagina and urethra. |
| Cleanse perineal area once daily with a mild soap. | Removes urine, discharge, and feces that can promote fungal growth. |
| Avoid tight-fitting clothing and underwear. | Increases temperature and moisture that can promote fungal growth. |
| Avoid douching, vaginal deodorants, essential oils, bubble baths, creams, or washing excessively. | Affect normal flora and may cause irritation and itching. |
| Avoid removing pubic hair. | Can cause lacerations where pathogens may enter. |
| Avoid using bidets. | May promote movement of E. coli from the anus into the vagina and urethra. |
- Family Doctor. (2023). Abnormal uterine bleeding. American Academy of Family Physicians. https://familydoctor.org/condition/abnormal-uterine-bleeding ↵
- Family Doctor. (2023). Abnormal uterine bleeding. American Academy of Family Physicians. https://familydoctor.org/condition/abnormal-uterine-bleeding ↵
- Family Doctor. (2023). Abnormal uterine bleeding. American Academy of Family Physicians. https://familydoctor.org/condition/abnormal-uterine-bleeding ↵
- Centers for Disease Control and Prevention. (2021). Sexually transmitted infections treatment guidelines: Bacterial vaginosis. https://www.cdc.gov/std/treatment-guidelines/bv.htm ↵
- Centers for Disease Control and Prevention. (2021). Sexually transmitted infections treatment guidelines: Bacterial vaginosis. https://www.cdc.gov/std/treatment-guidelines/bv.htm ↵
- Centers for Disease Control and Prevention. (2023). What is breast cancer? https://www.cdc.gov/cancer/breast/basic_info/what-is-breast-cancer.htm ↵
- “En_Breast_cancer_illustrations.png” by Morning2k for the National Institutes of Health is licensed in the Public Domain. ↵
- Centers for Disease Control and Prevention. (2023). What is breast cancer? https://www.cdc.gov/cancer/breast/basic_info/what-is-breast-cancer.htm ↵
- American Cancer Society. (2023). Breast cancer. https://www.cancer.org/cancer/types/breast-cancer/screening-tests-and-early-detection/american-cancer-society-recommendations-for-the-early-detection-of-breast-cancer.html ↵
- Centers for Disease Control and Prevention. (2023). What is breast cancer? https://www.cdc.gov/cancer/breast/basic_info/what-is-breast-cancer.htm ↵
- National Cancer Institute. (2023). Breast cancer treatment - (PDQ) patient version. National Institutes of Health. https://www.cancer.gov/types/breast/patient/breast-treatment-pdq#_185 ↵
- National Cancer Institute. (2021). Understanding cervical changes: A health guide. National Institutes of Health. https://www.cancer.gov/publications/patient-education/understanding-cervical-changes ↵
- National Cancer Institute. (2021). Understanding cervical changes: A health guide. National Institutes of Health. https://www.cancer.gov/publications/patient-education/understanding-cervical-changes ↵
- National Cancer Institute. (2021). Understanding cervical changes: A health guide. National Institutes of Health. https://www.cancer.gov/publications/patient-education/understanding-cervical-changes ↵
- National Cancer Institute. (2021). Understanding cervical changes: A health guide. National Institutes of Health. https://www.cancer.gov/publications/patient-education/understanding-cervical-changes ↵
- National Cancer Institute. (2021). Understanding cervical changes: A health guide. National Institutes of Health. https://www.cancer.gov/publications/patient-education/understanding-cervical-changes ↵
- National Cancer Institute. (2023). Endometrial cancer screening (PDQ) - patient version. National Institutes of Health. https://www.cancer.gov/types/uterine/patient/endometrial-screening-pdq ↵
- National Cancer Institute. (2023). Endometrial cancer screening (PDQ) - patient version. National Institutes of Health. https://www.cancer.gov/types/uterine/patient/endometrial-screening-pdq ↵
- National Cancer Institute. (2023). Endometrial cancer screening (PDQ) - patient version. National Institutes of Health. https://www.cancer.gov/types/uterine/patient/endometrial-screening-pdq ↵
- National Cancer Institute. (2022). Ovarian, epithelial, fallopian tube, and primary peritoneal cancer treatment (PDQ®)– patient version. National Institutes of Health. https://www.cancer.gov/types/ovarian/patient/ovarian-epithelial-treatment-pdq ↵
- National Cancer Institute. (2022). Ovarian, epithelial, fallopian tube, and primary peritoneal cancer treatment (PDQ®)– patient version. National Institutes of Health. https://www.cancer.gov/types/ovarian/patient/ovarian-epithelial-treatment-pdq ↵
- “Blausen_0349_Endometriosis.png” by Blausen.com staff (2014). “Medical gallery of Blausen Medical 201” is licensed under CC BY 3.0 ↵
- World Health Organization. (2023). Endometriosis. https://www.who.int/news-room/fact-sheets/detail/endometriosis ↵
- World Health Organization. (2023). Endometriosis. https://www.who.int/news-room/fact-sheets/detail/endometriosis ↵
- World Health Organization. (2023). Endometriosis. https://www.who.int/news-room/fact-sheets/detail/endometriosis ↵
- Office on Women's Health. (2021). Ovarian cysts. https://www.womenshealth.gov/a-z-topics/ovarian-cysts ↵
- Centers for Disease Control and Prevention. (2023). About pelvic inflammatory disease. https://www.cdc.gov/pid/about/index.html ↵
- Centers for Disease Control and Prevention. (2021). Sexually transmitted infections treatment guidelines: Pelvic inflammatory disease (PID). https://www.cdc.gov/std/treatment-guidelines/pid.htm ↵
- Centers for Disease Control and Prevention. (2023). About pelvic inflammatory disease. https://www.cdc.gov/pid/about/index.html ↵
- Centers for Disease Control and Prevention. (2021). Sexually transmitted infections treatment guidelines: Pelvic inflammatory disease (PID). https://www.cdc.gov/std/treatment-guidelines/pid.htm ↵
- Centers for Disease Control and Prevention. (2023). About pelvic inflammatory disease. https://www.cdc.gov/pid/about/index.html ↵
- Centers for Disease Control and Prevention. (2021). Sexually transmitted infections treatment guidelines: Pelvic inflammatory disease (PID). https://www.cdc.gov/std/treatment-guidelines/pid.htm ↵
- Centers for Disease Control and Prevention. (2023). About pelvic inflammatory disease. https://www.cdc.gov/pid/about/index.html ↵
- Centers for Disease Control and Prevention. (2021). Sexually transmitted infections treatment guidelines: Pelvic inflammatory disease (PID). https://www.cdc.gov/std/treatment-guidelines/pid.htm ↵
- “PCOS_%28Part_2%29.png” by BruceBlaus is licensed under CC BY 4.0 ↵
- Mayo Clinic. (2022). Polycystic ovary syndrome (PCOS). https://www.mayoclinic.org/diseases-conditions/pcos/symptoms-causes/syc-20353439 ↵
- Office on Women’s Health. (2021). Premenstrual syndrome (PMS). https://www.womenshealth.gov/menstrual-cycle/premenstrual-syndrome ↵
- MedlinePlus [Internet]. (2024). Premenstrual syndrome. https://medlineplus.gov/premenstrualsyndrome.html ↵
- Office on Women’s Health. (2021). Premenstrual syndrome (PMS). https://www.womenshealth.gov/menstrual-cycle/premenstrual-syndrome ↵
- MedlinePlus [Internet]. (2024). Premenstrual syndrome. https://medlineplus.gov/premenstrualsyndrome.html ↵
- Office on Women’s Health. (2021). Premenstrual syndrome (PMS). https://www.womenshealth.gov/menstrual-cycle/premenstrual-syndrome ↵
- MedlinePlus [Internet]. (2024). Premenstrual syndrome. https://medlineplus.gov/premenstrualsyndrome.html ↵
- Office on Women’s Health. (2021). Premenstrual syndrome (PMS). https://www.womenshealth.gov/menstrual-cycle/premenstrual-syndrome ↵
- MedlinePlus [Internet]. (2024). Premenstrual syndrome. https://medlineplus.gov/premenstrualsyndrome.html ↵
- Office on Women’s Health. (2021). Premenstrual syndrome (PMS). https://www.womenshealth.gov/menstrual-cycle/premenstrual-syndrome ↵
- MedlinePlus [Internet]. (2024). Premenstrual syndrome. https://medlineplus.gov/premenstrualsyndrome.html ↵
- Office on Women’s Health. (2021). Premenstrual syndrome (PMS). https://www.womenshealth.gov/menstrual-cycle/premenstrual-syndrome ↵
- MedlinePlus [Internet]. (2024). Premenstrual syndrome. https://medlineplus.gov/premenstrualsyndrome.html ↵
- Office on Women's Health. (2021). Premenstrual dysphoric disorder (PMDD). https://www.womenshealth.gov/menstrual-cycle/premenstrual-syndrome/premenstrual-dysphoric-disorder-pmdd ↵
- Office on Women's Health. (2021). Premenstrual dysphoric disorder (PMDD). https://www.womenshealth.gov/menstrual-cycle/premenstrual-syndrome/premenstrual-dysphoric-disorder-pmdd ↵
- Mayo Clinic. (2022). Uterine prolapse. https://www.mayoclinic.org/diseases-conditions/uterine-prolapse/symptoms-causes/syc-20353458 ↵
- Mayo Clinic. (2023). Anterior vaginal prolapse. https://www.mayoclinic.org/diseases-conditions/cystocele/symptoms-causes/syc-20369452 ↵
- Ross, A., & Shoff, H. W. (2023). Toxic shock syndrome. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK459345/ ↵
- “PCOS_%28Part_2%29.png” by BruceBlaus is licensed under CC BY 4.0 ↵
- NHS. (2023). Toxic shock syndrome. https://www.nhs.uk/conditions/toxic-shock-syndrome/ ↵
- Boston Children’s Hospital. (n.d.). Toxic shock syndrome. https://www.childrenshospital.org/conditions/toxic-shock-syndrome ↵
- “Uterine_Fibroids.png” by BruceBlaus is licensed under CC By 4.0 ↵
- Office on Women's Health. (2021). Uterine fibroids. https://www.womenshealth.gov/a-z-topics/uterine-fibroids ↵
- Office on Women's Health. (2021). Uterine fibroids. https://www.womenshealth.gov/a-z-topics/uterine-fibroids ↵
- Centers for Disease Control and Prevention. (2024). Candidiasis. https://www.cdc.gov/candidiasis/about/index.html ↵
- Centers for Disease Control and Prevention. (2024). Candidiasis. https://www.cdc.gov/candidiasis/about/index.html ↵
- Centers for Disease Control and Prevention. (2024). Candidiasis. https://www.cdc.gov/candidiasis/about/index.html ↵
- Graziottin, A. (2024). Maintaining vulvar, vaginal and perineal health: Clinical considerations. Women's Health, 20:17455057231223716. doi: 10.1177/17455057231223716. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10894559/ ↵
Any vaginal bleeding that occurs outside of the normal menstrual cycle, such as bleeding between periods, after sex, or after menopause.
Abnormally heavy or prolonged menstrual bleeding.
Abnormal uterine bleeding not associated with a physical condition such as pregnancy, infection, or cancer. It is often due to hormonal imbalances.
The natural cessation of menstrual periods for 12 consecutive months, marking the end of a woman's reproductive years.
Unpredictable menstrual bleeding that occurs more frequently, less frequently, or at irregular intervals. It may be a symptom of hormonal changes, medical conditions, or side effects of certain medications.
A medical procedure used to destroy the lining of the uterus (endometrium) to reduce or stop heavy menstrual bleeding.
Small, T-shaped devices inserted into the uterus to prevent pregnancy. IUDs can be hormonal or non-hormonal (copper) and provide long-term contraception.
A common vaginal infection caused by an imbalance in the natural bacteria found in the vagina. Symptoms include discharge, odor, and discomfort.
When breast cells mutate and become cancerous cells that multiply and form tumors.
The spread of cancer from its original site to other parts of the body, such as the bones, liver, or lungs.
A radiographic image of breast tissue that can detect signs of cancer, often before a lump is felt.
A breast ultrasound uses sound waves to make images, called sonograms, of areas inside the breast.
A type of mammogram used to investigate suspicious breast changes, such as a lump, pain, or unusual appearance on a screening mammogram.
A non-invasive imaging test that uses powerful magnets and radio waves to create detailed images of the breast.
A medical procedure in which a small sample of tissue is taken from the body for examination under a microscope to diagnose conditions such as cancer.
A surgical procedure that removes the cancerous tissue from the breast while preserving as much of the breast as possible. It is also known as a lumpectomy.
A surgical procedure in which the entire breast is removed to treat or prevent breast cancer. The underlying muscles and lymph nodes are left intact.
A surgical procedure that removes the entire breast, including some of the lymph nodes under the arm, but leaves the chest muscles intact. It is used to treat more advanced breast cancer.
Specific medications are prescribed by physicians to shrink or kill specific types of cancer cells.
Special medications are used to block cancer cells from getting the hormones they need to grow.
Targeted therapy works with the body’s immune system to help it fight cancer cells or to control side effects from other cancer treatments.
Uses high-energy rays (similar to X-rays) to kill the cancer cells.
Caused by the human papillomavirus (HPV).
A group of viruses that can cause genital warts and are linked to cancers of the cervix, anus, penis, and throat. Some strains of HPV can be prevented with vaccines.
A screening test in which cells are collected from the cervix and examined under a microscope to detect precancerous or cancerous changes.
A medical instrument used to widen the vaginal opening during gynecological exams to allow for inspection of the cervix and vagina.
A test used to detect the presence of human papillomavirus (HPV) in cervical cells. It is often done in conjunction with a Pap smear to screen for cervical cancer.
A term used to describe mild abnormalities in the cells on the surface of the cervix, often caused by HPV infection.
A term used to describe more severe abnormalities in cervical cells that are more likely to progress to cervical cancer if left untreated.
A type of pre-cancerous lesion in which glandular cells in the cervix have abnormal growth patterns. It can potentially develop into cervical cancer if not treated.
A procedure in which a colposcope (a special magnifying device) is used to closely examine the cervix, vagina, and vulva for signs of disease. It is often performed after an abnormal Pap test.
A surgical procedure in which a cone-shaped piece of abnormal tissue is removed from the cervix using a scalpel. This is often done to diagnose or treat precancerous conditions of the cervix.
A procedure that uses a thin wire loop charged with an electric current to remove abnormal tissue from the cervix. It is commonly used to treat precancerous changes in the cervix.
A treatment that uses extreme cold to freeze and destroy abnormal tissue. In reproductive health, it can be used to treat precancerous conditions of the cervix.
A procedure that uses a laser (a narrow beam of intense light) to destroy abnormal tissue. It is used in various treatments, including for abnormal cervical tissue, and typically requires general anesthesia when performed in a hospital setting.
A type of cancer that begins in the lining of the uterus (endometrium). It is the most common type of uterine cancer, often detected early due to abnormal vaginal bleeding.
A procedure in which a health care provider removes a small amount of tissue from the lining of the uterus (endometrium) using a brush, curette, or thin tube inserted through the cervix. The sample is then examined for signs of disease.
A surgical procedure in which lymph nodes are removed from an area, such as the pelvis, and examined for signs of metastatic cancer. This is often done to stage certain cancers, such as ovarian or endometrial cancer.
The surgical removal of one or more lymph nodes, often performed as part of cancer treatment or staging to determine if cancer has spread to the lymphatic system.
A type of cancer that begins in the tissues of the ovary. It can be difficult to detect early and often causes vague symptoms like bloating, pelvic pain, and abdominal discomfort.
A surgical procedure to remove part or all of the omentum, which is a layer of fatty tissue in the peritoneum that contains blood vessels, nerves, and lymph nodes. This procedure is often performed in the treatment of ovarian cancer.
The thin layer of tissue that lines the inside of the abdomen and covers most of the abdominal organs. It helps support the organs and contains blood vessels, nerves, and lymphatic vessels.
A chronic condition in which tissue similar to the lining of the uterus (endometrium) grows outside the uterus, often on the ovaries, fallopian tubes, or other pelvic organs. This can cause pain, inflammation, and infertility.
A fluid-filled sac that forms on or inside the ovary. Most ovarian cysts are benign and go away on their own, but some may cause pain or other symptoms and require treatment.
A minimally invasive surgical procedure in which a thin, lighted tube (laparoscope) is inserted through a small incision in the abdomen to examine the pelvic organs. It can be used for both diagnosis and treatment.
A surgical procedure in which a large incision is made in the abdomen to gain access to the abdominal and pelvic organs. It is often performed to diagnose or treat various medical conditions, including cancers.
An infection of the female reproductive organs, often caused by STIs like chlamydia or gonorrhea. It can result in infertility, ectopic pregnancy, and chronic pelvic pain.
Inflammation of the fallopian tubes, usually caused by infection. It is commonly associated with PID and can lead to infertility if untreated.
A collection of pus in or around the fallopian tubes and ovaries, typically resulting from a severe pelvic infection such as PID. This is a medical emergency requiring prompt treatment.
Inflammation of the peritoneum, the tissue lining the lower abdomen and surrounding the internal organs, often caused by infection. It can be a complication of PID or other pelvic infections.
A relationship in which both partners agree to have sexual relations only with each other. This type of relationship can reduce the risk of sexually transmitted infections (STIs).
A pregnancy in which the fertilized egg implants and begins to grow outside the uterus, most commonly in the fallopian tubes. This is a medical emergency that can be life-threatening if not treated.
A condition that causes women to not ovulate or to ovulate irregularly.
A condition in which women develop excessive hair growth in areas where men typically grow hair, such as the face, chest, and back. It is often caused by elevated androgen levels, as seen in conditions like PCOS.
A group of physical, emotional, and behavioral symptoms that occur in the one to two weeks before a woman's menstrual period. Common symptoms include mood swings, bloating, fatigue, and irritability. The symptoms typically resolve with the start of menstruation.
A severe form of PMS characterized by extreme mood changes, such as depression, irritability, and anxiety, along with physical symptoms like bloating and breast tenderness.
A condition in which an organ or tissue falls or slips from its normal position, usually due to weakening or damage to the supporting muscles or tissues.
A condition where the uterus descends from its normal position into the vaginal canal due to weakened pelvic muscles and ligaments, often caused by childbirth, aging, or other factors that weaken pelvic support.
This occurs when the walls of the vagina lose their support and either bulge or protrude through the vaginal opening.
A condition where the bladder bulges into the vagina, often due to weakened pelvic muscles, which can lead to urinary incontinence.
A condition in which the rectum bulges into the vaginal wall due to weakened pelvic muscles.
A rare but life-threatening condition caused by toxins produced by certain strains of bacteria, most commonly Staphylococcus aureus. It is often associated with the use of tampons or wound infections. Symptoms include high fever, rash, low blood pressure, and organ failure.
Non-cancerous growths that develop in or on the uterus, also known as leiomyomas or myomas. Fibroids can cause heavy menstrual bleeding, pain, and pressure in the pelvis, but many women with fibroids have no symptoms.
A surgical procedure to remove uterine fibroids while preserving the uterus. It is often recommended for women who wish to maintain fertility.
A surgical procedure that involves the removal of the uterus. It can be performed for various medical conditions, including fibroids, endometriosis, or cancer. Once performed, menstruation stops, and pregnancy is no longer possible.
A minimally invasive procedure that involves the destruction of fibroids using heat, cold, or electric current, causing the fibroid tissue to shrink.
A non-surgical procedure used to treat fibroids by blocking the blood supply to the fibroids, causing them to shrink. Small particles are injected into the uterine arteries during this procedure to cut off blood flow to the fibroid.
Similar to uterine fibroid embolization; a procedure where the uterine arteries are embolized (blocked) to treat various conditions, including fibroids, by cutting off the blood supply to abnormal tissue.
Also known as a yeast infection, VVC is a common fungal infection of the vulva and vagina caused by the overgrowth of Candida species. Symptoms include itching, burning, and a thick, white vaginal discharge.

