12.6 Congenital Conditions
Some infants have signs of congenital conditions soon after birth. This section will describe common congenital conditions.
Hydrocephalus
Hydrocephalus is a congenital condition caused by excessive cerebrospinal fluid (CSF) that puts pressure on the brain. CSF is clear fluid that protects and cushions the brain and spine. It flows through the ventricles of the brain and reabsorbs into the bloodstream. The body continuously makes and reabsorbs CSF. However, if the ventricles do not drain properly, CSF builds up and puts pressure on the brain. Symptoms of hydrocephalus in an infant are as follows[1]:
- Rapid increase in head size
- Unusually large head
- Bulging fontanelle
- Vomiting
- Difficulty sucking or feeding
- Sleepiness
- Irritability
- Sunset eyes (i.e., eyes are turned and fixed downward or do not turn outward)
- Seizures
In newborns, hydrocephalus may be caused by a genetic condition or deformities in the brain, spine, or spinal cord such as spina bifida. Other causes of hydrocephalus are intracranial bleeding from premature birth or brain swelling as a result of maternal infection, such as rubella.[2],[3]
Hydrocephalus is treated surgically. A shunt may be placed to drain the CSF from the brain to the chest or abdomen where it is reabsorbed.[4],[5]
View the Hydrocephalus Association’s image of ventriculoatrial and ventriculoperitoneal shunt placement.
A second option is endoscopic third ventriculostomy (ETV), where a surgical opening is made to divert excess CSF out of the brain. The procedure may also use cauterization to decrease the amount of brain tissue producing CSF.[6],[7]
Postoperatively, the client undergoing surgery for hydrocephalus requires routine monitoring by the health care provider. Parents must also monitor the child for signs of increasing CSF that may occur if the shunt should become blocked due to mechanical failure or infection.[8],[9]
The success of surgical treatment varies from person to person, with some people recovering completely after treatment with a good quality of life. Many people diagnosed with hydrocephalus benefit from rehabilitation therapies from an interdisciplinary team of medical professionals, rehabilitation specialists, and educational experts. Long-term issues for clients with hydrocephalus may include learning challenges, vision deficits, short-term memory or executive functioning loss, and chronic headaches.[10],[11]
Spina Bifida
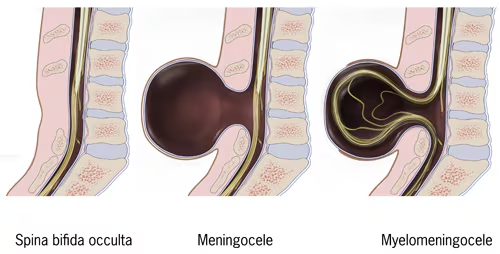
Spina bifida is a neural tube defect where the spine does not form or close correctly during fetal development in utero. It can occur anywhere along the spine, and its severity ranges from mild to severe based on the resulting damage to the spinal cord and/or nerves. The three most common types of spina bifida are spina bifida occulta, meningocele, and myelomeningocele. See Figure 12.31[12] for an image of the types of spina bifida. Spina bifida occulta is the mildest form that does not cause disabilities because the spine has a small gap but there is no opening or abnormal formation of the spine. Meningocele is a sac that protrudes through the opening, but no nerves are included, so only minor disabilities may result. Myelomeningocele is the most severe form and includes nerves protruding through the gap along with the sac, causing severe disabilities. The effects depend on where the myelomeningocele forms on the spine and includes decreased sensation below the level where it forms, as well as leg paralysis or difficulty with bowel or bladder control. Clients are also at risk for injuries and burns in areas of decreased sensation, as well as urinary tract infections if the bladder is affected.[13]
The cause of spina bifida is unknown, although insufficient intake of folic acid by the pregnant client may be a contributing factor. Other risk factors during pregnancy are overheating, poorly controlled diabetes, and certain medications. Pregnant clients may elect to have a screening blood test called a quad screen that includes checking levels of alpha fetoprotein. A high level of alpha fetoprotein may indicate spina bifida. Prenatal ultrasounds of the fetus may also indicate spina bifida.[14]
Treatment for spina bifida is tailored to each client according to their affected body systems and may include orthopedic, urological, and neurological treatments. Surgery may be performed on the fetus during gestation or within the first few days after birth to close the opening in the spine and decrease the impact on the child’s future function. Many clients with spina bifida have a latex allergy. Parents should avoid using latex pacifiers or nipples in newborns with spina bifida. Infants with spina bifida are at increased risk for hydrocephalus so signs of increased CSF pressure should be monitored. Physical therapists can help treat infants with spina bifida soon after birth by teaching parents how to perform leg exercises on the infant to increase their strength and flexibility. Some infants require braces to help support them as they learn to crawl and walk..[15]
Read more information about spina bifida in the “Congenital and Genetic Disorders” section of the “High-Risk Newborn Care” chapter.
Down Syndrome
Down syndrome (Trisomy 21) is a genetic condition that affects brain and body development due to an extra chromosome number 21. It is the most common chromosome problem diagnosed in the United States, with over 5,700 babies born annually with Down syndrome. Children with Down syndrome experience developmental delays but can lead healthy lives with support.[16]
Physical features of Down syndrome at birth include a flattened face and bridge of the nose, almond-shaped eyes that slant up, and a tongue that protrudes. Other signs include a short neck; small ears, hands, and feet; a single palmar crease on the hands; poor muscle tone; loose joints; and shorter than average length. Congenital heart defects, hearing loss, and obstructive sleep apnea may occur, as well as vision deficits, thyroid issues, gastroesophageal reflux, or a weakened immune system.[17],[18] See Figure 12.32[19] for an image of a child with Down syndrome.

The cause of Down syndrome is unknown. Although maternal age of 35 years or older increases the risk of Down’s syndrome, over half of newborns with Down syndrome are born to clients younger than 35.
Prenatal blood and ultrasound screening can indicate the risk of the fetus having Down syndrome, but they are not diagnostic. Chorionic villus sampling and amniocentesis are procedures used to accurately diagnose Down syndrome during the first or second trimesters.[20]
Treatment for children with Down syndrome depends on the severity of their condition. Early intervention for developmental delays starting soon after birth creates the best outcomes, including physical, occupational, and speech therapy.[21] Additional treatments for clients with Down syndrome and are described in Table 12.6.
Table 12.6. Conditions Associated With Down Syndrome and Evaluations and Treatments[22]
| Associated Conditions | Evaluation and Treatment |
|---|---|
| Cardiac |
|
| Eyes: Nearsightedness or cataracts |
|
| Hearing loss and ear infections |
|
| Immune deficiency and infections |
|
| Hypothyroidism |
|
| Anemia, polycythemia, leukemia |
|
| Misshapen bones in upper spine |
|
| Sleep disorders |
|
| Periodontal disease |
|
| Epilepsy |
|
| Structural gastrointestinal problems or digestive problems such as gastroesophageal reflux or Celiac disease |
|
| Anxiety, depression, and/or attention deficit hyperactivity disorder (ADHD) |
|
Nurses can support families of children with Down syndrome by referring them to resources and support groups from the National Association for Down Syndrome.
Read additional information at the National Association for Down Syndrome website.
Clubfoot
Clubfoot is a congenital condition where the lower leg and foot turns inward and downward. The extremity may be rigid or flexible. True clubfoot is genetic, whereas positional clubfoot is caused by abnormal positioning of the foot while the fetus is developing in the womb. Maternal smoking, diabetes, and alcohol use increase the risk for clubfoot. See Figure 12.33[23] for an image of clubfoot.[24]

Club foot is diagnosed by a health care provider during a physical exam at birth, or it may be detected on a prenatal ultrasound. Clubfoot may occur concurrently with spina bifida or developmental hip dysplasia. Treatment includes serial casting to remodel the soft tissue, which means casts are routinely changed, approximately five to nine times. The casts gradually realign the foot in a process that is similar to untwisting a twisted towel. After serial casting, braces with a boot and bar are used to space the feet about shoulder width apart. See Figure 12.34[25] for an image of clubfoot braces. Bracing starts after the final cast until about four years of age to maintain the correction obtained by casting.[26]

Developmental Hip Dysplasia
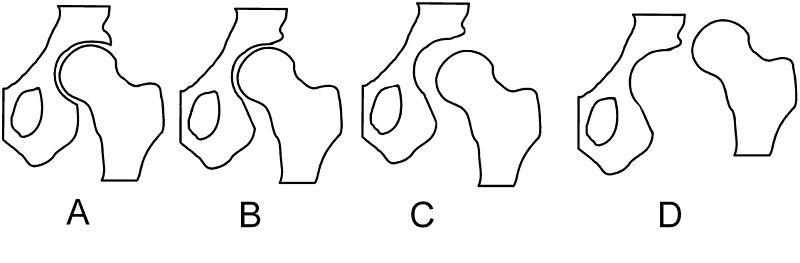
Developmental dysplasia of the hip (DDH) refers to several hip abnormalities, including neonatal instability, acetabular or femoral dysplasia, and hip subluxation. Females are at higher risk for DDH and hip dislocation. DDH is caused by a combination of genetic, environmental, and mechanical factors. Maternal hormones of estrogen and progesterone must be in balance or high levels of estrogen promote dislocation. Mechanical factors include positioning of the newborn’s femur in the acetabulum, with abduction of the leg contributing to correct joint development. Breech presentation and swaddling after birth with the legs adducted interfere with hip development.[27] See Figure 12.35[28] for different types of misalignments of the femoral head to the acetabulum in hip dysplasia.
Health care providers perform the Barlow and Ortolani maneuvers during physical examination of newborns and infants to detect DDH. During these maneuvers, the provider flexes the infant’s legs and adducts the knees while checking if the head of the femur dislocates away from the acetabulum. Outward pressure is then applied to the knees to abduct the legs and replace the head of the femur in the acetabulum. These maneuvers are considered positive if the provider feels a click with subluxation or dislocation or a click with reduction of the dislocation.[29]
Early detection and treatment of DDH prior to the age of six months creates the best outcomes for the client, with later detection typically leading to more extensive surgery. Untreated DDH contributes to hip arthritis and pain with hip arthroplasty required as an adult. A Pavlik harness is an effective treatment to maintain an abducted position of the infant’s legs to keep the head of the femur close to the acetabulum. See Figure 12.36[30] for an image of an infant wearing a Pavlik harness to help the head of the femur and acetabulum develop correctly while allowing some leg movement. The provider may choose to wait and observe four to six weeks before applying the Pavlik harness because some hips stabilize on their own. Drawbacks of the Pavlik harness are difficulty with breastfeeding, car seat use, and bathing.[31],[32]

View a supplementary YouTube video[33] on physical assessments for developmental hip dysplasia: How to Test for Newborn Hip Dysplasia by N. Gold | OPENPediatrics.
Cleft Lip and Palate
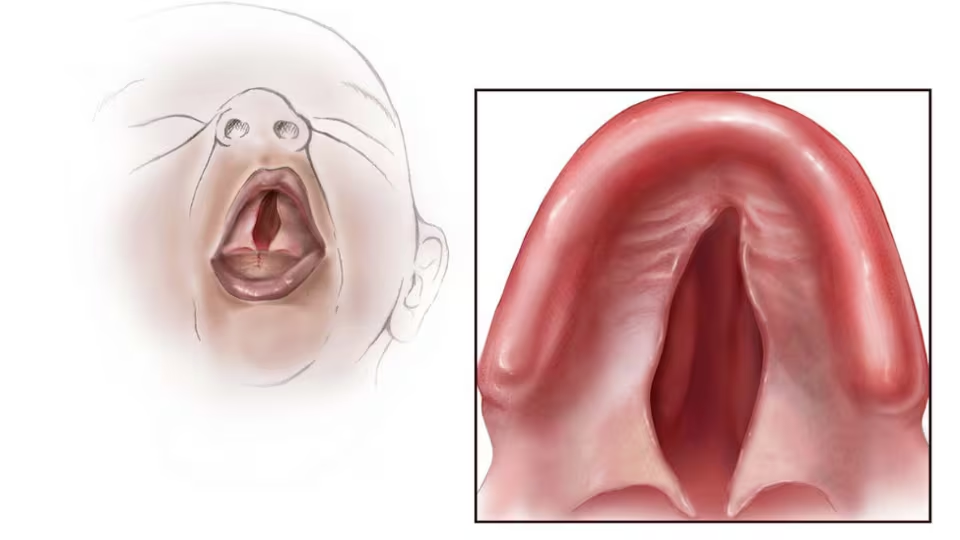
As a fetus develops in the uterus, it begins with a split in the hard palate (i.e., roof of the mouth) and on each side of the center of the upper lip. Around Week 6 to 11 of gestation, the cleft usually closes. However, if it doesn’t close properly, the infant is born with a cleft lip and/or cleft palate. Cleft lip can be one-sided, centered, or bilateral and range from a small slit to an opening up into the nose. These deformities can result in difficulty eating, breathing, speaking, or hearing, as well as abnormal tooth development and ear infections. Cleft lip and palate can be caused by genetic factors; gestational diabetes; or maternal intake of alcohol, tobacco, Accutane, or seizure medication during pregnancy. Diagnosis may be made during a prenatal ultrasound or upon physical examination after birth.[34],[35] See Figure 12.37[36] for an illustration of cleft lip and 12.38[37] for an illustration of cleft palate.

Treatment involves many members of the multidisciplinary team. Because cleft lip and cleft palate may have a genetic component that causes additional health conditions, families are referred for genetic counseling to determine the extent of congenital conditions and future needs of the infant. Infants may have one or multiple surgeries to repair cleft lip by the age of one and cleft palate by the age of 18 months. Until the repairs are completed, the infants and toddlers require assistance with feeding, speaking, and hearing from a nutritionist, speech pathologist, and audiologist. The cleft interferes with sucking because the newborn has difficulty making a seal on a nipple, and the milk can move into the nose or airway, putting them at risk for aspiration and increasing the work of feeding that can lead to fatigue. Nurses teach parents different techniques to try to help the infant latch on the nipple. Alternative methods of feeding with syringes, cups, soft nipples, or spoons may work, and the infant needs careful monitoring to make sure food intake is sufficient. After surgery, infants require special attention to feeding because sucking puts pressure on surgical incisions. Nurses teach parents/caregivers to report signs of aspiration or low weight gain.[38],[39]
Infants may require treatment by a pediatric dentist and/or orthodontist for tooth alignment and early intervention for lip formation. The orthodontist can make a mold or tape the lips to help shape them.[40] With treatment, most children do well and lead a healthy life. Nurses can refer parents/caregivers to parent-to-parent support groups to assist with coping.
Read additional information in the “Cleft Lip & Cleft Palate” section of the “Other Childhood Disorders” chapter.
Read additional information about support groups on the CDC’s Cleft Lip/Palate web page.
Congenital Heart Defects
Congenital heart defects can range from asymptomatic to severe defects requiring surgical intervention.
Detailed information about congenital heart defects is discussed in the “Congenital Heart Defects” chapter.
- National Institute of Neurological Disorders and Stroke. (n.d.). Hydrocephalus. https://www.ninds.nih.gov/health-information/disorders/hydrocephalus ↵
- National Institute of Neurological Disorders and Stroke. (n.d.). Hydrocephalus. https://www.ninds.nih.gov/health-information/disorders/hydrocephalus ↵
- Hydrocephalus Association. (2023). Shunt systems. https://www.hydroassoc.org/shunt-systems/ ↵
- National Institute of Neurological Disorders and Stroke. (n.d.). Hydrocephalus. https://www.ninds.nih.gov/health-information/disorders/hydrocephalus ↵
- Hydrocephalus Association. (2023). Shunt systems. https://www.hydroassoc.org/shunt-systems/ ↵
- National Institute of Neurological Disorders and Stroke. (n.d.). Hydrocephalus. https://www.ninds.nih.gov/health-information/disorders/hydrocephalus ↵
- Hydrocephalus Association. (2023). Shunt systems. https://www.hydroassoc.org/shunt-systems/ ↵
- National Institute of Neurological Disorders and Stroke. (n.d.). Hydrocephalus. https://www.ninds.nih.gov/health-information/disorders/hydrocephalus ↵
- Hydrocephalus Association. (2023). Shunt systems. https://www.hydroassoc.org/shunt-systems/ ↵
- National Institute of Neurological Disorders and Stroke. (n.d.). Hydrocephalus. https://www.ninds.nih.gov/health-information/disorders/hydrocephalus ↵
- Hydrocephalus Association. (2023). Shunt systems. https://www.hydroassoc.org/shunt-systems/ ↵
- “Typesofspinabifida.jpg” by unknown author for Centers of Disease Control and Prevention (CDC) is in the Public Domain. ↵
- Centers for Disease Control and Prevention. (2024). About spina bifida. https://www.cdc.gov/spina-bifida/about/index.html ↵
- Centers for Disease Control and Prevention. (2024). About spina bifida. https://www.cdc.gov/spina-bifida/about/index.html ↵
- Centers for Disease Control and Prevention. (2024). About spina bifida. https://www.cdc.gov/spina-bifida/about/index.html ↵
- Centers for Disease Control and Prevention. (2024). Down syndrome. https://www.cdc.gov/birth-defects/about/down-syndrome.html ↵
- Centers for Disease Control and Prevention. (2024). Down syndrome. https://www.cdc.gov/birth-defects/about/down-syndrome.html ↵
- Down Syndrome Association of Central Ohio. (n.d.). How nurses can help new parents. [PDF]. https://dsaco.net/wp-content/uploads/How-Nurses-Can-Help-New-Parents.pdf ↵
- “child-7245915_1920.jpg” by Zachtleven fotografie from Pixabay is licensed under CC0 ↵
- Centers for Disease Control and Prevention. (2024). Down syndrome. https://www.cdc.gov/birth-defects/about/down-syndrome.html ↵
- National Down Syndrome Society. (n.d.). Early intervention. https://ndss.org/resources/early-intervention ↵
- National Institute of Child Health and Human Development. (n.d.). Down syndrome. https://www.nichd.nih.gov/health/topics/downsyndrome ↵
- “Pied_bot,_varus_équin_(bilateral).jpg” by Brachet Youri is licensed under CC BY-SA 3.0 ↵
- Barrie, A., & Varacallo, M. (2023). Clubfoot. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK551574/ ↵
- “botas.jpg” by Dolmanrg is licensed under CC BY-SA 4.0 ↵
- Barrie, A., & Varacallo, M. (2023). Clubfoot. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK551574/ ↵
- Bakarman, K., Alsiddiky, A. M., Zamzam, M., Alzain. K. O., Alhuzaimi, F. S., & Rafiq, Z. (2023). Developmental dysplasia of the hip (DDH): Etiology, diagnosis, and management. Cureus, 15(8), e43207. https://pubmed.ncbi.nlm.nih.gov/37692580/ ↵
- “Hip_dysplasia_-_schematic.jpg” by Londenp at nl.wikipedia is licensed under CC BY-SA 3.0 ↵
- Bakarman, K., Alsiddiky, A. M., Zamzam, M., Alzain. K. O., Alhuzaimi, F. S., & Rafiq, Z. (2023). Developmental dysplasia of the hip (DDH): Etiology, diagnosis, and management. Cureus, 15(8), 43207. https://pubmed.ncbi.nlm.nih.gov/37692580/ ↵
- “Saeugling_mit_angelegter_spreizhose.jpg” by Thiemo Schuff is licensed under CC BY-SA 3.0 ↵
- Bakarman, K., Alsiddiky, A. M., Zamzam, M., Alzain. K. O., Alhuzaimi, F. S., & Rafiq, Z. (2023). Developmental dysplasia of the hip (DDH): Etiology, diagnosis, and management. Cureus, 15(8), e43207. https://pubmed.ncbi.nlm.nih.gov/37692580/ ↵
- Cook, K. A., Schmitt, M., Ingram, M., Larson, J. E., Burgess, J., & Janicki, J.A. (2019). Pavlik Harness initiation on Barlow positive hips: Can we wait? Journal of Orthopaedics, 16(5), 378–381. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6495102/ ↵
- OPENPediatrics. (2018, July 11). How to test for newborn hip dysplasia by N. Gold | OPENPediatrics [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=Qy3uSkDhMZs ↵
- Centers for Disease Control and Prevention. (2024). Cleft lip/Cleft palate. https://www.cdc.gov/birth-defects/about/cleft-lip-cleft-palate.html ↵
- Walker, N. J., Anand, S., & Podda, S. (2023). Cleft lip. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK482262/ ↵
- “Untitled-design-12” by unknown author at Centers for Disease Control and Prevention (CDC) is in the Public Domain. ↵
- “Untitleddesign26” by unknown author at Centers for Disease Control and Prevention (CDC) is in the Public Domain. ↵
- Walker, N. J., Anand, S., & Podda, S. (2023). Cleft lip. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK482262/ ↵
- Phalke, N., & Goldman, J. J. (2023). Cleft palate. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK563128/ ↵
- National Institute of Dental and Craniofacial Research. (2021). Cleft lip & palate. https://www.nidcr.nih.gov/health-info/cleft-lip-palate ↵
A congenital condition caused by excessive cerebrospinal fluid (CSF) that puts pressure on the brain.
A neural tube defect where the spine does not form or close correctly during fetal development in utero.
A genetic condition that affects brain and body development due to an extra chromosome number 21.
A congenital condition where the lower leg and foot turns inward and downward.
Refers to several hip abnormalities, including neonatal instability, acetabular or femoral dysplasia, and hip subluxation.

