Chapter 7: Pharmacology
Jay Steuer
7.1 Introduction
On a busy highway at rush hour, EMR Dana Chen arrived first at a rollover crash. The driver was pinned in his seat, pale and sweating profusely. While assessing him, Dana noticed a medical alert bracelet: “Diabetic – Insulin Dependent.” Recognizing the signs of severe hypoglycemia, she quickly administered oral glucose paste. Within minutes, the patient’s confusion lifted, and his vital signs stabilized—all before the ambulance even arrived.
This is the critical role pharmacology plays in emergency medical response. As an EMR, you are often the first medical professional on scene, making your pharmacological knowledge vital. The medications you administer in those first minutes can dramatically affect a patient’s outcome.
Why This Matters Most for EMRs
You are the first line of defense in medical emergencies. Whether it’s administering aspirin for a potential heart attack, epinephrine for anaphylaxis, or naloxone for opioid overdose, your pharmacological decisions in those initial moments set the course for all subsequent treatment. This chapter doesn’t just teach you about medications—it prepares you to make decisions that save lives. Because when you are first on scene, patients aren’t just counting on medical help—they are counting on you.
Learning Objectives
- Understand safe medication administration.
- Identify medications within the EMR scope of practice.
- Determine appropriate indications for use.
- Recognize and address polypharmacy risks.
7.2 Understanding Medications
Drug Name and Dosage
The foundation of any medication consideration begins with accurately identifying each drug’s name and dosage. This includes both generic and brand names (e.g., “acetaminophen” versus “Tylenol”), as patients may reference them differently. Dosage information specifies the strength (e.g., “500 mg”) and frequency (e.g., “every 6 hours as needed”), which helps EMRs determine if a patient is taking appropriate amounts or is at risk for overdose. For example, finding that a patient takes “Warfarin 5 mg daily” immediately alerts the EMR to potential bleeding risks during trauma care (Open RN Pharmacology, 2023).
Route of Administration
Understanding how a medication enters the patient’s system is critical for assessing its effects and potential interactions. Common routes include oral (PO), sublingual (SL), inhaled (INH), intramuscular (IM), and intravenous (IV). Each route affects drug absorption rates and bioavailability. For instance, sublingual nitroglycerin acts within minutes for chest pain, while oral medications may take much longer. An EMR must consider whether a patient’s current administration method could influence their condition, such as an asthma patient improperly using an inhaler, and adjust treatment accordingly (National Association of Emergency Medical Technicians [NAEMT], 2022).
Purpose of Medication
Knowing why a patient takes each medication provides insight into their medical history and current health status. For example, a patient taking metformin likely has diabetes, while sertraline suggests managed depression or anxiety. This information helps EMRs anticipate potential complications; a diabetic patient may experience hypoglycemia, while someone on antidepressants could be at risk for serotonin syndrome if given certain medications. Documenting the purpose (e.g., “for atrial fibrillation” or “to prevent blood clots”) creates a clearer clinical picture and guides emergency interventions (U.S. National Library of Medicine, 2022).
Allergies and Adverse Reactions
Documented allergies and past adverse reactions (e.g., rashes, anaphylaxis, or gastrointestinal effects) are among the most urgent components of a medication profile. EMRs must verify allergies before administering any drug, as even common medications like aspirin can trigger life-threatening reactions. Contraindications can be more important than indications, but are often less emphasized or recognized.
Operational Considerations
Effective medication management extends beyond clinical administration to encompass storage integrity, expiration monitoring, and meticulous documentation. EMRs must ensure medications remain within specified temperature ranges and replace expired supplies promptly. Legal documentation should capture precise administration times, observed effects, and any protocol deviations, while clear communication during patient handoff ensures continuity of care. Note that an adverse side effect or reaction does not indicate an error. Each medication administration is a risk/benefit decision. Some patients will experience an adverse reaction. The reporting of these reactions enhances the application and helps define future use of the medication. These operational practices collectively enhance patient safety and treatment efficacy in dynamic prehospital environments.
Medication Safety: The 6 Rights of Medication
Review the “Rights” of medication administration with every patient every time.
- Right Patient
Prescribed for this person.
Situation requires this medication.
Caution when treating more than one patient at a time. - Right medication/indication
Correct medication for the situation per protocol or medical control contact.
Confirm medication with partner as required. - Right route
Medications may have multiple routes possible. - Right dose
Dose for the situation.
Modifications for age, weight, or other considerations.
Dose may change based on the route chosen.
Caution if the vial contains multiple doses. - Right time
Check expiration date.
If indicated, give repeat dose at correct time. - Right documentation
Record the response to medication, including any adverse effects.
Condition and vital signs before and after medication administration.
Complete the patient care report.
7.2 Essential Medications in the EMR Scope of Practice
EMRs operate with a carefully selected pharmacological arsenal designed to address life-threatening conditions in unpredictable prehospital environments. The medications authorized for EMR administration meet stringent criteria, including rapid action for critical conditions, favorable safety profiles, and straightforward administration methods suitable for field use (American Heart Association [AHA], 2023). These pharmacological tools empower EMRs to initiate life-saving interventions during the crucial minutes before advanced medical support arrives. The medications permitted or required for each level of EMS provider can vary by state. Confirm your scope of practice and agency treatment guidelines before attempting to administer medications.
Oxygen: The Foundation of Respiratory Support
As the most fundamental medication in emergency care, oxygen therapy serves as the first-line intervention for hypoxia and respiratory distress. EMRs typically administer oxygen via non-rebreather masks, delivering 60-90% fraction of inspired oxygen (FiO2) at greater than 15 liters per minute (LPM) for severely compromised patients, or nasal cannulas providing 24-44% FiO2 at 1-6 LPM for more stable cases (National Association of Emergency Medical Technicians [NAEMT], 2022). Special consideration must be given to chronic obstructive pulmonary disease (COPD) patients, where excessive oxygen may precipitate dangerous hypercapnia. Proper storage and handling are equally crucial, as oxygen cylinders require secure mounting and regular inspection to ensure medical-grade purity and prevent contamination.
Safe Handling of Oxygen
Preparation
- Use appropriate body substance isolation.
- Oxygen cylinders must be handled carefully since the contents are under high pressure.
- Selection of a delivery device will depend on the patient’s condition.
- Regulators reduce the cylinder’s pressure to a safe level and regulate the flow of gas in liters per minute.
Administration
- Identify cylinder by color, correct pin code, and 100% USP marking.
- Remove protective cap or tape.
- Quickly open and close the cylinder valve to “crack” so as to remove any impurities which may have accumulated on the mating surfaces between the tank and regulator.
- Attach regulator and flowmeter, and ensure a leak proof seal.
- Turn on the cylinder and check the pressure gauge to ensure adequate pressure.
- Attach the appropriate delivery device to the flowmeter.
- Adjust flow control to deliver the recommended level.
- Fit delivery device to patient.
- Check adequacy of flow to patient.
Discontinuation
- Remove the oxygen delivery device from the patient.
- Shut off the cylinder and bleed regulator.
- Return flow meter control to “off” position.
View the following supplementary YouTube videos to learn more:
EMT Oxygen Administration
Oxygen Administration: Non Re-breather Mask
Device Flow Rates and Oxygen Percentage
| Device | Flow Rate | Oxygen Percentage |
|---|---|---|
| Nasal Cannula | Flow Rate: 1-6 L/min | FiO2: 24% to 44% |
| Simple Mask | Flow Rate: 5-10 L/min | FiO2: 28% to 50% |
| Non-Rebreather Mask | Flow Rate: 10 to 15 L/min | FiO2: 60-90% |
| Bag Valve Mask | Flow Rate: 15 L/min | FiO2: 100% |
Safety With Oxygen Therapy
Oxygen therapy supports life, but it also supports fire. While there are many benefits to oxygen therapy, there are also many hazards.
Oxygen Therapy Safety Guidelines
- Remember that oxygen is a medication.
- Store oxygen cylinders correctly.
- When using oxygen cylinders, store them upright, chained, or in appropriate holders so that they will not fall.
- Full oxygen tanks should be stored separately from partially full or empty oxygen tanks.
- Use tank holders appropriately.
- When transporting a patient, proper tank holders must be used.
- Do not allow smoking near the oxygen devices.
- Oxygen supports combustion. No smoking is permitted around any oxygen delivery devices.
- Keep oxygen cylinders away from heat sources.
- Keep oxygen delivery systems at least 5 feet from any heat source.
- Check for electrical hazards in the home prior to use.
- Determine that electrical equipment in the room or home is in safe working condition.
- A small electrical spark in the presence of oxygen will result in a serious fire.
- The use of a gas stove, kerosene space heater, or smoker is unsafe in the presence of oxygen.
- Avoid items that may create a spark (e.g., electrical razor, hair dryer, synthetic fabrics that cause static electricity, or mechanical toys) with nasal cannula in use.
- Petroleum-based lubricants should not be used on the lips or around the nasal cannula.
- Check levels of oxygen in portable tanks.
- Check oxygen levels of portable tanks before transporting a patient to ensure that there is enough oxygen in the tank.
- The EMS standard is to replace oxygen tanks at 500-1000 PSI per policy.
Albuterol: Bronchospasm Rescue
Nebulized albuterol (2.5mg/3mL) provides targeted relief for reactive airway diseases through selective beta-2 adrenergic stimulation. Adrenergic stimulation is related to adrenaline in the fight-or-flight response. It would open bronchioles to increase air flow. While generally effective, EMRs should monitor for rare paradoxical bronchospasm and recognize when treatment failure suggests status asthmaticus requiring advanced intervention (National Asthma Education and Prevention Program, 2021). Proper administration requires functioning nebulizer equipment and an oxygen source, emphasizing the importance of regular equipment checks.
- Category:
- Albuterol is a short-acting beta-2 agonist.
- Mechanism of Action:
- Albuterol stimulates beta 2-adrenergic receptors in the smooth muscle of bronchi and bronchioles producing bronchodilation.
- Beta-1 receptors can also be inadvertently stimulated, causing tachycardia.
- Indications:
- Short-acting albuterol is used to prevent or treat bronchospasms in people with asthma, reversible obstructive airway disease, or exercise-induced bronchospasm.
- Considerations:
- Monitor respiratory rate, oxygen saturation, and lung sounds before and after administration.
- Side Effects/Adverse Effects:
- Beta-2 agonists can cause muscle tremor, excessive cardiac stimulation, and CNS stimulation.
Equipment
Metered Dose Inhaler (MDI)

Assist Administration of an MDI
- Place the medication canister into the inhaler and remove the end cap.
- Shake inhaler.
- Prime inhaler with one compression if not recently used.
- Direct the patient to place the mouthpiece of the MDI in their mouth making a seal with their lips.
- Have the patient exhale completely, and then push down on the canister, and have the patient then breathe in slowly for 3-5 seconds. Take as big a breath as possible.
- Try to hold the inhalation for up to 10 seconds.
- Release the mouthpiece and exhale.
- Administer oxygen and repeat if dosage is more than one puff.
Administer Albuterol via Nebulizer
- Determine Medication Rights.
- Assemble nebulizer, load Albuterol solution, and have patient hold nebulizer.
- Administer Albuterol Sulfate 2.5 mg in 3.0 mL via nebulizer (1 unit dose).
- Set oxygen flow rate of 6-8 LPM to establish nebulized medication mist.
- Patient to place mouthpiece and close lips to seal.
- Encourage the patient to breathe more deeply about every 10 breaths.
- Treatment may last 5-15 minutes.
- Reassess the patient.
- After the initial dose, if symptoms persist, a second and third dose may be given.
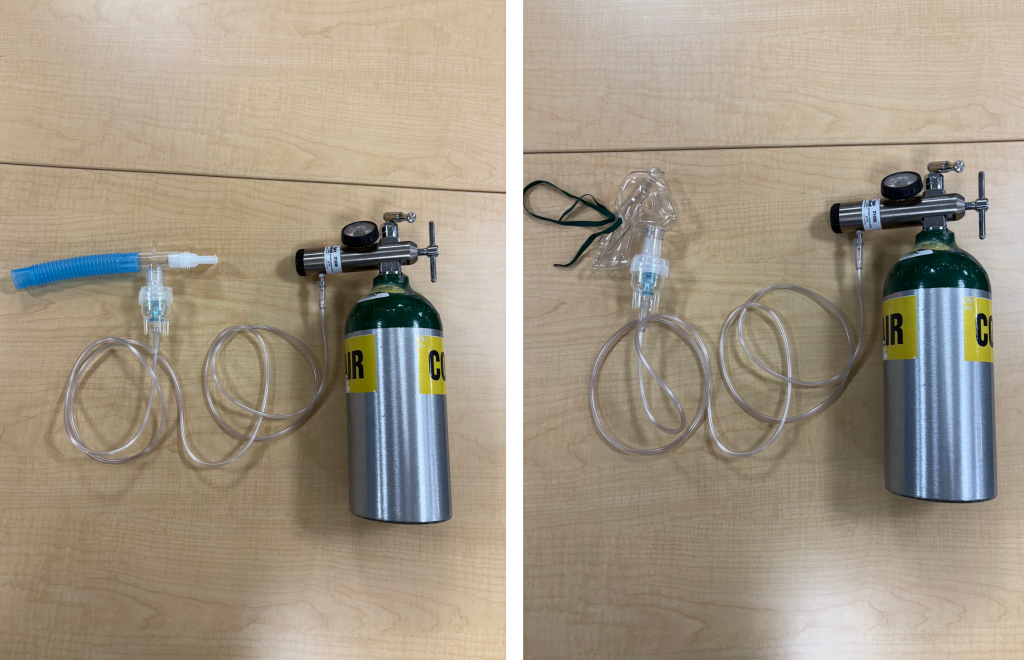
Figure 7.2 Nebulizer and Mask attachments
View the following YouTube video for a technique demonstration (first four minutes of video):
A note about combining oxygen sources, as in switching a patient from high flow oxygen on a non-rebreather mask to a nebulizer treatment. Recognize that the oxygen flow for the nebulizer must be kept at 6-8 LPM. Increasing to higher flow will be wasting medication by expelling it out beyond the patient. The correct method to increase oxygenation while administering a nebulizer treatment is to add a nasal cannula. This will also require a second oxygen source.
Epinephrine: The Anaphylaxis Lifeline
Epinephrine auto-injectors (typically 0.3 mg for adults and 0.15 mg for children) provide rapid reversal of severe allergic reactions through combined alpha-1 and beta-2 adrenergic effects. The medication’s vasoconstrictive action counters dangerous hypotension while its bronchodilatory effect relieves airway obstruction (World Allergy Organization, 2022). Proper technique involves intramuscular injection into the anterolateral thigh, which can be performed through clothing if necessary. EMRs may be asked to assist with administration if the patient is attempting to use their own auto-injector, or administer a dose from stock. You must remain vigilant as a second dose is often required if no improvement is seen in 5 minutes.
- Category:
- Adrenergic (also referred to as catecholamines) that stimulates the beta- and alpha-receptors on the target cell.
- Mechanism of Action:
- Epinephrine acts on both alpha- and beta-adrenergic receptors and is used in several routes, including intravenously, subcutaneously, intramuscularly, and inhalation.
- Epinephrine decreases vasodilation and decreases vascular permeability through its alpha-adrenergic receptor action.
- Through its action on beta-adrenergic receptors, epinephrine causes bronchial smooth muscle relaxation and helps alleviate bronchospasm, wheezing, and dyspnea that may occur during anaphylaxis.
- Indications:
- Epinephrine is used for severe allergic reactions and anaphylaxis.
- Considerations:
- Administer with caution to the elderly and those with preexisting cardiovascular disease.
- Monitor vitals (blood pressure, heart rate, and respiratory rate) and cardiovascular and respiratory systems closely.
- Side Effects/Adverse Effects:
- Common side effects include hypertension and tachycardia.
Epinephrine Auto-Injector Administration
- Determine the Medication Rights (Adult dose 0.3 mg, pediatric dose 0.15 mg if under 66 pounds/30 kg/ 8 years of age or per protocol.)
- Remove auto-injector from protective carrier tube.
- Confirm the medication is clear and colorless and not expired.
- If possible, identify the vastus lateralis thigh muscle and cleanse the area in an outward circular motion.
- Grip the auto-injector in your fist (Keep fingers and thumb clear of auto-injector ends.)
- Place the auto-injector at 90 degrees to the injection site.
- Remove the end cap to activate the auto-injector.
- Grip the patient’s leg to stabilize.
- Firmly press and hold the auto-injector into thigh until there is an audible click. (The needle will automatically retract after injection)
- Remove auto-injector and massage area for 10 seconds to assist with medication absorption.
- Dispose auto-injector in a sharp’s container.
- Apply bandage over the injection site.
- Monitor for improvement in symptoms. May repeat in 5 minutes or per protocol.
View the following YouTube video for a technique demonstration (between 11:30 – 13:30 minute mark):
Aspirin: The Cardiac First Response
The 324 mg chewable aspirin dose represents a cornerstone intervention for suspected acute coronary syndromes. This is usually in the form of four 81 mg tablets. Its mechanism of irreversible platelet inhibition begins within 30 minutes of administration, making early intervention critical (AHA, 2023). This intervention has been incorporated in various emergency medical dispatch programs, and the patient may have already taken the aspirin before your arrival. If not, EMRs must verify the absence of aspirin allergies or active bleeding before administration. A true allergy with wheezing, swelling, or anaphylaxis must be differentiated from the patient being told to avoid aspirin due to interactions with other medications or stomach upset. Next you should instruct the patient to chew the tablets thoroughly to accelerate buccal absorption. Note that if a patient self-administered enteric coated aspirin without chewing it thoroughly, the dose should be repeated with chewable tablets. Documentation should include precise administration time and dose, as this information proves vital for subsequent hospital care.
- Category
- Anti-platelet, analgesic, antipyretic, anti-inflammatory medication.
- Mechanism of Action
- Inhibits platelet activation and aggregation.
- Indications
- Cardiac chest pain or myocardial infarction.
- Considerations
- Chewable aspirin is used due to its rapid absorption.
- Side-Effects/Adverse Effects
- Increases risk of bleeding.
Aspirin Administration
- Determine Medication Rights.
- Adult dose is typically 324 mg or four 81 mg chewable tablets.
- May be two to four 81 mg tablets per protocol.
- Allow the patient to place one or all of the tablets in their mouth (Caution that it is common for an anxious patient to drop the tablet(s).)
- Remind them to chew the tablets, instead of directly swallowing.
- The patient may have a small sip of water to clear the taste out of their mouth if they request it.
Nitroglycerin: Coronary Vasodilation

Sublingual nitroglycerin (0.4mg) has potent vasodilatory effects. The EMR will encounter patients who use this medication for chest pain. The medication reduces cardiac workload through venous pooling and coronary artery dilation, but carries absolute contraindications including systolic blood pressure below 90 mmHg or 30 mmHg below baseline, extreme bradycardia below 50 bpm, or tachycardia above 100 bpm in the absence of heart failure, and recent phosphodiesterase-5 inhibitor (trade names such as Viagra or Cialis) use (AHA, 2010). Proper administration involves placing the medication under the tongue, followed by close monitoring for both therapeutic effect (pain relief) and potential adverse effects (hypotension). Note that nitroglycerin degrades rapidly, so if a patient is using older medication, they may see little to no effects.
- Category:
- Antianginal, Vasodilation
- Mechanism of Action:
- Nitroglycerin relieves angina by relaxing vascular smooth muscle, resulting in vasodilation
- Indications:
- Nitroglycerine is used to relieve angina due to coronary artery disease, during times of an acute attack, or prophylactically
- Considerations:
- Patients using sildenafil (Viagra) or similar medications for erectile dysfunction in the previous 24-48 hours may not take nitroglycerin as this may result in a dangerous drop in blood pressure.
- Nitroglycerin is contraindicated in clients who have severe anemia, increased intracranial pressure, hypersensitivity, or circulatory failure.
- EMS treatment guidelines restrict nitroglycerin use when BP is less than 90-100 mmHg. Consult your agency guidelines
- Side Effects/Adverse Effects:
- Hypotension, palpitation, headache, weakness, sweating, flushing, nausea, vomiting, or dizziness
- Health Teaching and Health Promotion:
- Patients should allow medication to dissolve under their tongue
- May take up to one tablet every 5 minutes or up to three sublingual tablets within 15 minutes to relieve chest pain
- Special Considerations:
- Patients should sit during administration to decrease the risk of injury due to the possibility of hypotension, dizziness, and weakness
- Nitroglycerin decomposes when exposed to heat or light, so it should be stored in the original, airtight glass container.
Nitroglycerin Assisted Administration
- The patient requests assistance with their own medication.
- Determine Medication Rights.
- Obtain vital signs to identify any contraindications.
- Don gloves prior to handling medication.
- Remove 1 tablet from the bottle and place or assist the patient to place under their tongue.
Caution that it is common for an anxious patient to drop the tablet.
Coach against chewing or swallowing the tablet. - Allow to dissolve.
- Recheck level of chest pain and vital signs in 3-5 minutes.
- Patients are typically instructed to take up to three tablets.
- Consult protocols or medical control for further dosing.
Clinical Integration: Cardiac Emergency Protocol
You are responding to a 58-year-old male with chest pain who has taken his prescribed nitroglycerin as directed for three doses, but his pain continues. His vital signs include a BP of 148/92, and SpO2 of 92%. The EMR initiates nasal cannula oxygen at 4L/min, improving oxygenation to 98%. After verifying no contraindications, the responder administers 324 mg chewable aspirin (four 81 mg tablets) with documentation at 09:32. Throughout the intervention, the EMR prepares for potential complications by monitoring vital signs and having an AED accessible (AHA, 2023).
Oral Glucose: Hypoglycemia Reversal
Oral glucose gel (15-25 g) offers rapid correction of diabetic emergencies through direct buccal absorption. This route proves particularly valuable for patients with altered mental status (American Diabetes Association, 2023). Safety precautions include proper patient positioning and confirmation of intact gag reflex to prevent aspiration and careful reassessment of blood glucose levels following administration. When commercial glucose gel is not available, sugar-containing liquids may serve as alternatives, though with less predictable absorption rates. The safest way to administer regular liquids is to allow the patient to hold the container and drink. If they cannot control the container, they probably cannot protect their airway.
Always keep hypoglycemia in mind for anyone with altered mental status, especially those who have been labeled as “just drunk.” On the other side, hypoglycemia should be responding to treatment within about 15 minutes. If not, there are many other reasons for altered mental status that must be considered.
Oral Glucose Administration
- Simply letting the patient ingest the gel from the tube themselves is the safest choice.
- If they require assistance, placing gel on a tongue blade and applying it to their inner cheek is an alternative.
- Strict airway-monitoring is necessary.
- As their mental status improves, they should be able to increase their participation in their own care.
View the following supplementary YouTube video on oral glucose for hypoglycemia in EMS: EMT/Paramedic Medication Notecards || Oral Glucose
Naloxone for Opioid Overdose
Opioid misuse and exposure remains a major public health problem in the United States. In 2021, over nine million people misused opioids, and there were 80,411 fatal opioid-involved overdoses—a 61.3% increase from 2019. Naloxone has become a common antidote not only for EMS providers, but also for law enforcement, public health workers, teachers, family members, and citizens. Naloxone (brand name Narcan) is now available in all 50 states. Transitioning the delivery of naloxone from an intravenous or intramuscular route to a nasal spray increased the safety of those administering treatment with the avoidance of accidental needle-stick injuries.

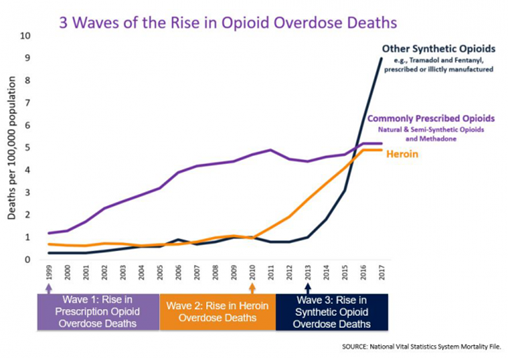
The rise in opioid overdose deaths can be outlined in three distinct waves. See the figure below for a graphic representation of the waves of opioid deaths.
Recognizing the signs and symptoms of opioid overdose is crucial in EMS. Appropriate treatment with airway management is key. You have the advantage of being trained in airway support maneuvers to provide optimal recovery while administering the appropriate dose of naloxone. Simply administering large doses of naloxone may precipitate acute opioid withdrawal, which causes other medical issues. It is to your advantage to avoid inducing withdrawal and the associated combativeness.
Similar to considerations in altered mental status and hypoglycemia discussed above, if your interventions are not progressing as expected, you will need to evaluate other causes for altered mental status and expand your treatment.
Naloxone (Narcan)
- Mechanism of Action:
- Naloxone reverses analgesia and the CNS and respiratory depression caused by opioid agonists.
- It competes with opioid receptor sites in the brain and, thereby, prevents binding with receptors or displaces opioids already occupying receptor sites.
- Indications:
- Naloxone is indicated for the complete or partial reversal of opioid depression, including respiratory depression induced by natural and synthetic opioids.
- Depressed mental status.
- Depressed respiratory status.
- Pinpoint pupils.
- Evidence of illicit drug use, especially injection drugs.
- Considerations:
- Naloxone is safe for all ages.
- Side Effects/Adverse Effects:
- Adverse effects include tremors, sweating, hypertension, nausea, and vomiting.
Abrupt reversal of opioid effects in persons who are physically dependent on opioids may precipitate an acute withdrawal syndrome, which may include, but not limited to, the following signs and symptoms: body aches, fever, sweating, runny nose, sneezing, piloerection (goose bumps), yawning, weakness, shivering or trembling, nervousness, restlessness or irritability, diarrhea, nausea or vomiting, abdominal cramps, increased blood pressure, ventricular tachycardia or fibrillation, or pulmonary edema which may result in death.
View the following supplementary YouTube video to learn more about Naloxone:
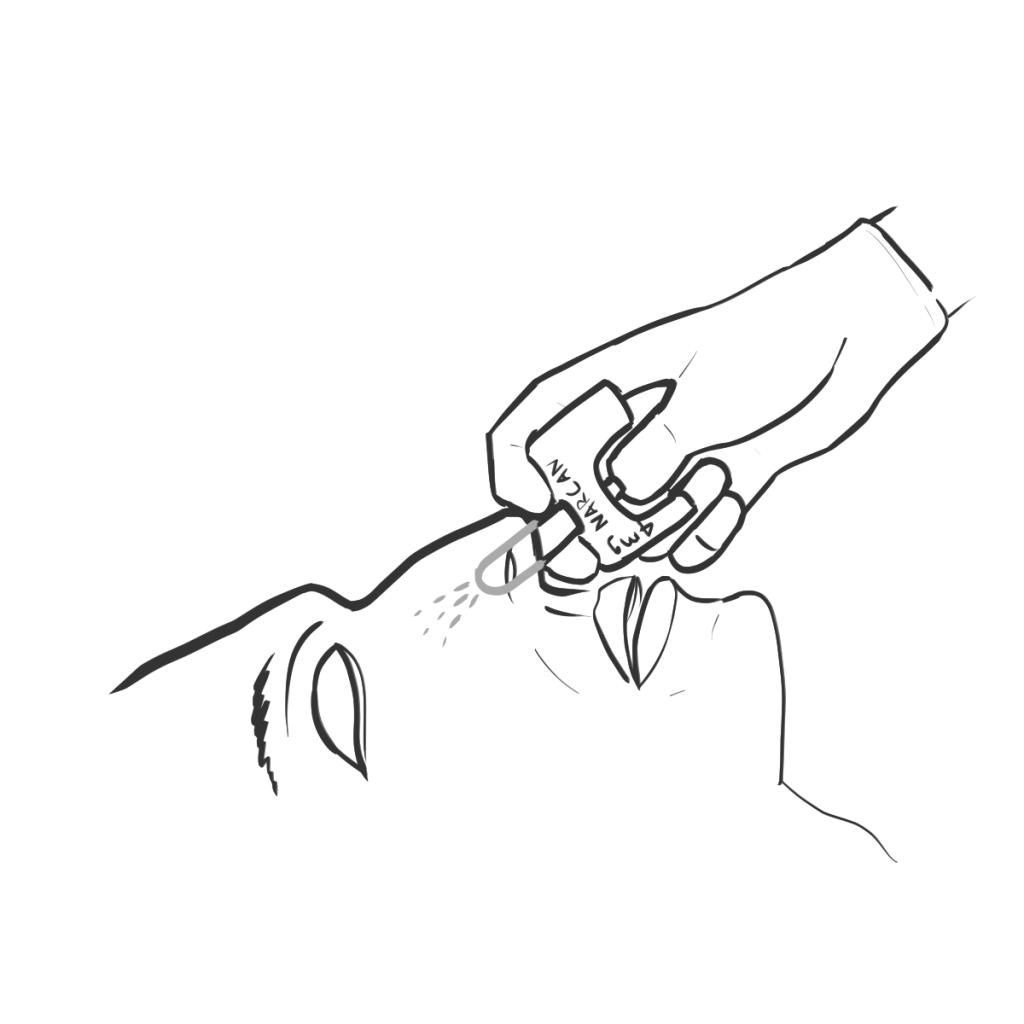
Administration of Intranasal Naloxone
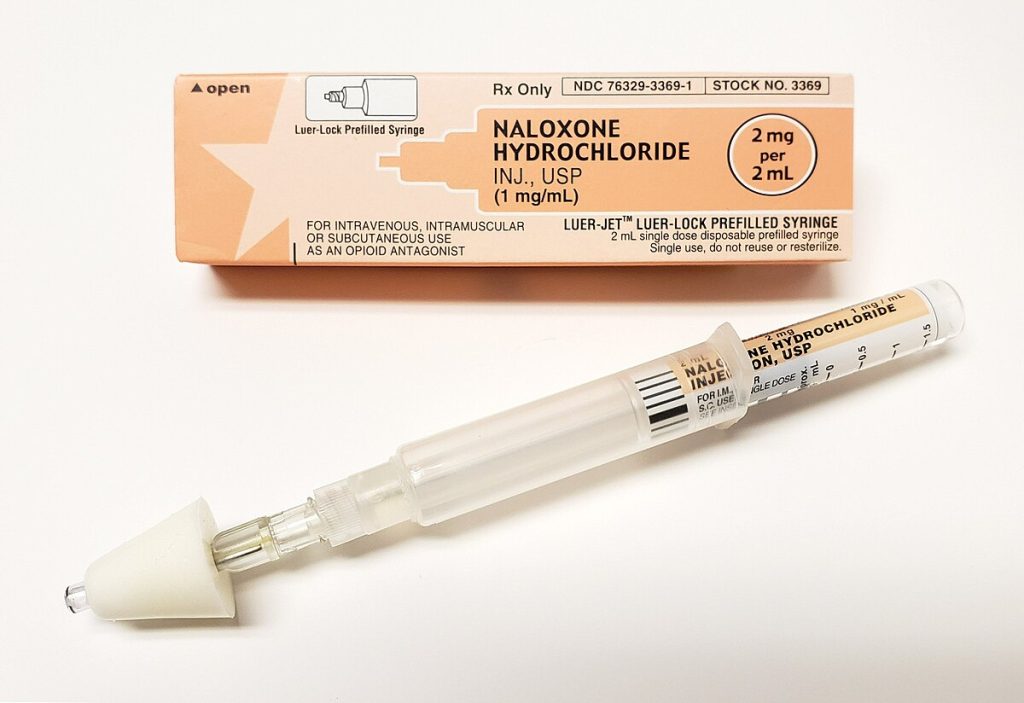
The recommended concentrations of naloxone for EMS use are 2 mg per 2 ml prefilled syringe which may be attached to a nasal atomizer device or the over-the-counter available 4 mg per 0.1 ml single dose nasal spray. The main difference is that the prefilled syringe is titratable and the nasal spray is not. The 4 mg dose may precipitate acute withdrawal.
- The Prefilled Naloxone Syringe
-
- Determine Medication Rights.
- Attention to cardiopulmonary support as needed.
- Airway maneuvers.
- CPR.
- BSI/PPE required.
- Expect a significant change in your patient.
- Skin and mucous membrane exposure.
- Expect to decontaminate appropriately afterwards.
- Assemble the prefilled syringe.
- Attach a nasal administration device.
- Note: Recommended to add 0.1 ml bubble to syringe prior to administration to improve nasal mist delivery.
- Dose 0.5-1 mg (0.5-1 ml) per nostril.
- May repeat in 5 minutes.
-
View the following supplementary resource for more information (selecting link will download the presentation):
Antidote Auto-injector

Some EMS systems are involved in military response or accessing the Strategic National Stockpile of medications. Nerve agent antidote is part of the stockpile. This auto-injector has progressed over the decades from the Mark 1 device to the Antidote Treatment Nerve Agent Autoinjector (ATNAA) or trade name DuoDote. Additional training is required to utilize these medications. Administration is similar to using an epinephrine auto-injector.
Isopropyl Alcohol for Inhalation to Decrease Nausea
For decades, postoperative recovery area staff have known that the smell of rubbing alcohol (isopropyl alcohol) decreases nausea and vomiting. It was a practice passed down, but not studied until the 1990s. The mechanism of action is unclear, as there are many triggers for nausea and vomiting. The reported success rates vary and the effect is often temporary. However, isopropyl alcohol swabs are readily available in medical settings and are inexpensive. Often this is seen as an option to decrease nausea while obtaining more definitive medication.
Administering Isopropyl Alcohol for Inhalation
- Determine Medication Rights.
- Open an isopropyl alcohol swab.
- Direct patient to hold it close to their nose, at a distance of 1-2 cm.
- Direct patient to take three deep breaths through their nose.
- Patient may choose to continue as they wish.
- Provide additional isopropyl alcohol swabs.
- Address further treatment plans as needed.
Activated Charcoal for Ingestions

Activated charcoal is an antidote for certain oral ingestions. It is mostly only used under the direction of Poison Control or the patient’s physician, with the family or caregivers having it available. Once used routinely, important limitations and contraindications have been identified. The patient must be alert and have a controlled airway to avoid aspiration, as vomiting is common. Activated charcoal is only effective for certain medications or chemicals, and to be effective it must be administered within 1 hour of the ingestion, before the substance leaves the stomach and moves into the small intestine. Donning extra PPE is recommended for anyone coming into contact with activated charcoal, as it is messy.
Commonly dispensed in bottles of 25 or 50 grams, the dose will be determined by the ordering healthcare provider. It is a thick, grainy solution that must be shaken to mix the charcoal. Some brands are flavored with a cherry additive. Otherwise, it is recommended to mix with a dark, sweet liquid, such as cola or chocolate milk.
7.3 Clinical Indications and Contraindications for EMR-Administered Medications
Clinical Decision-Making in Emergency Pharmacology
A structured approach to medication administration begins with comprehensive patient assessment. In allergic reactions, the EMR must distinguish between rash and true anaphylaxis with airway compromise before epinephrine administration. Epinephrine administration requires vigilance, particularly in patients with pre-existing hypertension or cardiovascular disease. While life-saving for anaphylaxis, its potent vasoconstrictive effects may exacerbate hypertensive crises or precipitate cardiac ischemia in vulnerable patients. The EMR must balance these risks against the life-threatening nature of anaphylaxis, where delayed administration carries greater mortality risk than potential cardiovascular complications.
Special Population Considerations
Pediatric patients require additional safeguards in medication administration. Dose calculations based on weight must be verified, with special attention to decimal placement and unit conversions. Many EMS systems utilize length-based resuscitation tapes or precalculated dosing charts to minimize errors.
Geriatric patients present unique challenges due to altered pharmacokinetics and frequent polypharmacy. Medication effects may be prolonged or intensified, requiring careful monitoring after administration. EMRs should maintain particular caution with sedating medications in elderly patients due to increased fall risk.
Quality Improvement and Error Prevention
Effective medication safety systems incorporate multiple safeguards including:
- Independent double-checks.
- Standardized concentration systems.
- Clear labeling and storage practices.
- Regular competency assessments.
- Nonpunitive error reporting systems.
These measures work collectively to reduce the risk of medication errors while maintaining the rapid response capability essential in EMS (Prehospital Emergency Care, 2023).
7.4 Polypharmacy Risks Across the Lifespan: A Clinical Perspective for EMS Providers
The Growing Burden of Polypharmacy in Emergency Care
Polypharmacy represents a growing public health concern that significantly impacts EMS. Defined as the concurrent use of five or more medications, this phenomenon affects patients of all ages but manifests differently across developmental stages. For EMS providers, understanding these age-specific risks is crucial for accurate patient assessment and safe medication administration in prehospital settings.
Pediatric Vulnerabilities: When Small Bodies Meet Multiple Medications
In pediatric populations, polypharmacy risks primarily stem from dosing complexities and off-label medication use. Children’s developing physiology processes medications differently than adults, with variations in absorption, distribution, metabolism, and excretion that change throughout growth stages. Emergency providers must be particularly vigilant about weight-based dosing calculations, as errors in decimal placement or unit conversion can lead to dangerous under- or overdosing. The National Association of EMS Physicians emphasizes the importance of using length-based resuscitation tapes rather than visual estimates when determining pediatric medication doses. Additionally, many children receive over-the-counter medications before EMS arrival that may interact with emergency treatments, making thorough medication history-taking essential.
Geriatric Polypharmacy: When Treatment Becomes the Threat
Geriatric patients face perhaps the most significant consequences of polypharmacy due to age-related physiological changes and multiple chronic conditions. The American Geriatrics Society Beers Criteria identifies several classes of medications that pose special risks for older adults, including benzodiazepines (sedatives), anticholinergics (found in cough and allergy medications), and certain cardiovascular medications. These substances can contribute to falls, cognitive impairment, and hospitalizations when prescribed inappropriately or combined dangerously. EMS providers should pay particular attention to medication-related delirium, which often mimics other acute conditions but requires different management approaches. The CDC notes that nearly 40% of adults over 65 take five or more prescription medications, with many taking supplements or over-the-counter drugs that further complicate their medication profiles.
Obstetric Considerations: Protecting Two Patients with One Regimen
Pregnant patients present unique polypharmacy challenges due to fetal vulnerability and maternal physiological adaptations. The U.S. Food and Drug Administration’s pregnancy risk categories, while being replaced by more detailed labeling requirements, still provide valuable guidance for emergency medication decisions. Many commonly used emergency medications carry potential risks that must be balanced against maternal benefits.
From Recognition to Action: Practical Strategies for EMS Providers
Practical strategies for EMS providers include maintaining heightened awareness of medication-related presentations, documenting complete medication histories including supplements and recreational substances, and clearly communicating polypharmacy concerns during patient handoffs. While prehospital providers typically don’t adjust long-term medications, recognizing and reporting potentially dangerous combinations constitutes an important patient safety intervention. System-level improvements like pediatric and geriatric-specific protocols can further enhance polypharmacy recognition and management in emergency medical services.
References
2023 American Geriatrics Society BEERS Criteria Update Expert Panel. (2023). American Geriatrics Society 2023 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. Journal of the American Geriatrics Society, 71(7), 2052-2081. https://doi.org/10.1111/jgs.18372
Amaya, S., Kalsotra, S., Tobias, J. D., & Olbrecht, V. A. (2023). Clinical experience with the use of inhaled isopropyl alcohol to treat nausea and vomiting: A narrative review. Saudi Journal of Anaesthesia, 17(3), 383–390. https://pmc.ncbi.nlm.nih.gov/articles/PMC10435785/
American Academy of Pediatrics. (2023). Pediatric medication safety in emergency settings. Pediatrics, 151(2), e2022059591.
American Diabetes Association. (2023). Standards of medical care in diabetes-2023. Diabetes Care, 46(Supplement_1). https://diabetesjournals.org/care/issue/46/Supplement_1
American Heart Association. (2023). Advanced cardiovascular life support provider manual.
American Red Cross. (2017). Emergency medical response. https://www.redcross.org/content/dam/redcross/training-services/course-fact-sheets/EMR-Textbook-2017-LoRes-111017.pdf
Board on Health Sciences Policy; Health and Medicine Division; National Academies of Sciences, Engineering, and Medicine. (2016). 2, The strategic national stockpile: Origin, policy foundations, and federal context. In The Nation’s Medical Countermeasure Stockpile: Opportunities to Improve the Efficiency, Effectiveness, and Sustainability of the CDC Strategic National Stockpile: Workshop Summary. National Academies Press (US). https://www.ncbi.nlm.nih.gov/books/NBK396378/
Bruun, H., Milling, L., Mikkelsen, S. et al. (2022). Ethical challenges experienced by prehospital emergency personnel: A practice-based model of analysis. BMC Medical Ethics 23(80). https://doi.org/10.1186/s12910-022-00821-9
Cardona, V., Ansotegui, I. J., Ebisawa, M., El-Gamal, Y., Fernandez Rivas, M., Fineman, S., Gellar, M., Gonzalez-Estrada, A., Borges, M. S., Senna, G., Sheikh, A., Tanno, L. K., Thong, B. Y., & Turner, P. (2022). Anaphylaxis guidance. World Allergy Organization Journal, 13(10). https://doi.org/10.1016/j.waojou.2020.100472
Centers for Disease Control and Prevention. (2023). Overdose prevention. https://www.cdc.gov/overdose-prevention/index.html
DeNicola, P. (2024). Aspirin in the prehospital setting. JEMS. https://www.jems.com/patient-care/cardiac-resuscitation/aspirin-in-the-prehospital-setting/
Drug Enforcement Administration. (n.d.). Controlled substances act. United States Drug Enforcement Administration. https://www.dea.gov/drug-information/csa
Ernstmeyer, K., & Christman, E. (Eds.). (2023). Nursing pharmacology 2e. Open RN. https://wtcs.pressbooks.pub/pharmacology2e/
Ernstmeyer, K., & Christman, E. (Eds.). (2023). Nursing skills 2e. Open RN. https://wtcs.pressbooks.pub/nursingskills/
Institute for Safe Medication Practices. (2023). Implement strategies to prevent persistent medication errors and hazards. ISMP Medication Safety Alert! Acute Care, 28(6).
https://www.ismp.org/sites/default/files/newsletter-issues/20230323.pdf
Hanlon, J. & Schmader, K. E. (2022). The medication appropriateness index: A clinimetric measure. Psychotherapy and Psychosomatics, 91(2), 78–83. https://doi.org/10.1159/000521699
Hegenbarth, M. A., & American Academy of Pediatrics Committee on Drugs. (2008). Preparing for pediatric emergencies: Drugs to consider. Pediatrics, 121(2), 433–443. https://doi.org/10.1542/peds.2007-3284
JEMS. (2023). Best practices for medication management in EMS. Journal of Emergency Medical Services, 48(4), 32–38.
Kumar, N., Fatima, M., Ghaffar, S., Subhani, F., & Waheed, S. (2023). To resuscitate or not to resuscitate? The crossroads of ethical decision-making in resuscitation in the emergency department. Clinical and Experimental Emergency Medicine, 10(2), 138-146. https://doi.org/10.15441/ceem.23.027
Kuzel, A. R., & Kuhl, E. A. (2023). EMS medical director legal issues and liability. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK597344/
Leonard, J. (2024). Can you use an expired inhaler? Medical News Today. https://www.medicalnewstoday.com/articles/321163
Lindblad, A. J., Ting, R., & Harris, K. (2018). Inhaled isopropyl alcohol for nausea and vomiting in the emergency department. Canadian family physician Medecin de famille canadien, 64(8), 580. https://pmc.ncbi.nlm.nih.gov/articles/PMC6189884/
Lincoln, E. W., Reed-Schrader, E., & Jarvis, J. L. (2023). EMS quality improvement programs. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK536982/
Lowrie, L. N., Duncan, L., Samuels, D. A., Ablah, E., & Ofei-Dodoo, S. (2023). Prehospital clinical decision-making for medication administration for behavioral emergencies. Kansas Journal of Medicine, 16(2), 189–193. https://doi.org/10.17161/kjm.vol16.20261
Ma, X., Xiaokaiti, Y., Lei, H., Liu, W., Xu, J., Sun, Y., Zhao, X., Pu, X., & Zhai, S. (2017). Epinephrine inhibits vascular hyperpermeability during platelet-activating factor- or ovalbumin-induced anaphylaxis. RSC Advances, 7(83), 52762–52771. https://doi.org/10.1039/c7ra09268g
Mansour, O., Russo, R. G., Straub, L., Bateman, B. T., Gray, K. J., Huybrechts, K. F., & Hernández-Díaz, S. (2024). Prescription medication use during pregnancy in the United States from 2011 to 2020: Trends and safety evidence. American Journal of Obstetrics and Gynecology, 231(2), 250.e1–250.e16. https://doi.org/10.1016/j.ajog.2023.12.020
McDermott, C., & Collins, N. C. (2012). Prehospital medication administration: A randomised study comparing intranasal and intravenous routes. Emergency Medicine International, 2012, 476161. https://doi.org/10.1155/2012/476161
Naas, C. J., Nickel, L. B., Aufderheide, T. P. & Weston, B. W. (2025). Disparities in emergency medical services termination of resuscitation practices for patients with out-of-hospital cardiac arrest. Prehospital Emergency Care, 1-24. https://doi.org/10.1080/10903127.2025.2487135
National Asthma Education and Prevention Program Coordinating Committee. (2021). 2020 focused updates to the asthma management guidelines. U.S. Department of Health and Human Services. https://www.nhlbi.nih.gov/resources/2020-focused-updates-asthma-management-guidelines
National Center for Ethics in Health Care. (2023). Policy. U.S. Department of Veteran Affairs. https://www.ethics.va.gov/policy.asp
National Heart, Lung, and Blood Institute. (2021). How to Use a Metered-Dose Inhaler. https://www.nhlbi.nih.gov/sites/default/files/publications/How-to-Use-a-Metered-Dose-Inhaler_21-HL-8165.pdf
National Kidney Foundation. (n.d.). Safe medication use with chronic kidney disease.
https://www.kidney.org/kidney-topics/safe-medication-use-chronic-kidney-disease
Newmark, J. (2019). Therapy for acute nerve agent poisoning. Neurology Clinical Practice, 9(4), 337–342. https://pmc.ncbi.nlm.nih.gov/articles/PMC6745742/
PediPec. (2025). Preparing for pediatric emergencies: Drugs to consider. https://www.pedistat.com/blog/preparing-for-pediatric-emergencies
Redlener, M., & Jarvis, J. (2023). 2023 new national EMS quality alliance measure set: Tools for EMS to operationalize evidence based care. National EMS Quality Alliance. https://www.nemsqa.org/assets/2023%20NEW%20National%20EMS%20Quality%20Alliance%20Measure%20Set%20Tools%20for%20EMS%20to%20Operationalize%20Evidence%20Based%20Care%20Webinar%20Slides%209.5.23.pdf
Silberman, J. (2023). Activated Charcoal. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK482294/
Simon, S. T., Kini, V., Levy, A. E., & Ho, P. M. (2021). Medication adherence in cardiovascular medicine. BMJ (Clinical research ed.), 374(n1493). https://doi.org/10.1136/bmj.n1493
Substance Abuse and Mental Health Services Administration. (2020). Key substance use and mental health indicators in the United States: Results from the 2019 National Survey on Drug Use and Health (HHS Publication No. PEP20-07-01-001, NSDUH Series H-55). Center for Behavioral Health Statistics and Quality. https://www.samhsa.gov/data/sites/default/files/reports/rpt29393/2019NSDUHFFRPDFWHTML/2019NSDUHFFR090120.htm
Tariq, R. A., Vashisht, R., & Sinha, A., et al. (2024). Medication dispensing errors and prevention. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK519065/
US Davis PSNet Editorial Team. (2024). Medication reconciliation. Agency for Healthcare Research and Quality & US Department of Health and Human Services. https://psnet.ahrq.gov/primer/medication-reconciliation
U.S. Department of Health and Human Services. (2023). EMS ethical decision-making.
https://www.ems.gov/standards.html
U.S. Food and Drug Administration. (2014). Expiration dating and stability testing for human drug products. https://www.fda.gov/inspections-compliance-enforcement-and-criminal-investigations/inspection-technical-guides/expiration-dating-and-stability-testing-human-drug-products
U.S. Food and Drug Administration. (2023). Pregnancy and lactation labeling final rule.
https://www.fda.gov/drugs/labeling-information-drug-products/pregnancy-and-lactation-labeling-drugs-final-rule
Van Wilder, L., Devleesschauwer, B., Clays, E., Pype, P., Vandepitte, S., & De Smedt, D. (2022). Polypharmacy and health-related quality of life/psychological distress among patients with chronic disease. Preventing Chronic Disease, 19:220062. http://dx.doi.org/10.5888/pcd19.220062
Welter, C., Roschel, K., Schneider, S., Marson, C., & Stammet, P. (2022). Impact of ambient temperature on 5 emergency drugs aboard an emergency medical car over a 1-year period. Annals of Emergency Medicine, 80(4), 358-363. https://doi.org/10.1016/j.annemergmed.2022.05.001
Wisconsin Department of Health. (2014). 2014 EMR naloxone presentation [PPT]. https://www.dhs.wisconsin.gov/ems/training/2014emrnaloxoneppt.pptx
Wisconsin Department of Health. (2023). Wisconsin EMS protocols [PDF]. https://www.dhs.wisconsin.gov/publications/p02875.pdf
Images:
Figure 7.1: “Ventolin® HFA (Albuterol Sulfate) Inhaler.jpg” by MisterNarwhal is licensed under CC BY-SA 4.0
Figure 7.2: “neb_mask_oxygen” by Mark Schwartz, Chippewa Valley Technical College is licensed under CC BY-NC 4.0
Figure 7.3: “Nitroglycerin (1).JPG” by Intropin is licensed under CC BY 3.0
Figure 7.4: “31579570334_91f027440c_k” by VCU Capital News Service is licensed under CC BY-NC 2.0
Figure 7.5: “Narcan_Administration” by Eldridge Misnomer is licensed under CC BY-SA 4.0
Figure 7.6: “3 Waves of the Rise of Opioid Overdose Deaths” by National Vital Statistics System, CDC is licensed under CC0
Figure 7.7: “Naloxone_6_(Cro,His,Rot)” by Intropin (Mark Oniffrey) is licensed under CC BY-SA 4.0
Figure 7.8: “AutoinjectorMarkI” by USGov is in the Public Domain.
Figure 7.9: “CharcoalPO” by James Heilman, MD is licensed under CC BY-SA 3.0
Videos:
HealthONE EMS. (2015, June 3). EMT oxygen administration [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=zmpqn7SEjLY&t=158s
San Diego Miramar EMT Program. (2020, February 25). Oxygen administration: non re-breather mask [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=ysxH_ZJCHao
WCTCFire&EMS. (2012, August 11). EMS Skills – BLS medication preparation and administration [Video]. YouTube. CC BY 4.0 https://www.youtube.com/watch?v=0SIG0N65yN
Lights Sirens Action EMS. (2019, December 2). EMT/Paramedic medication notecards || Oral Glucose [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=jtHPiucoZ6E
SAMHSA. (2018, September 25). What is Naloxone? [Video]. YouTube. Public Domain. https://www.youtube.com/watch?v=RcAaZQQqd50

