Chapter 17: EMS Operations
Ryan Skabroud, EdD
17.1 Introduction
This chapter will prepare the Emergency Medical Responder (EMR) to understand emergency services operations. Upon completion of this chapter the EMR should be able to recognize safety hazards and safely conduct patient care in a variety of operational environments.
17.2 Field Operations
Learning Objectives
- Describe safety precautions to be taken while working at scenes on and near roadways.
- Describe the major phases of an ambulance call and the EMR’s responsibilities during each phase
- Describe post-run actions that should be taken to reduce the spread of infection
- Describe privileges afforded to responders operating emergency vehicles and the precautions that must be observed
- Describe appropriate use of emergency warning devices
On Jan. 4, 2008, Chippewa County Sheriff’s Department Deputy Jason Zunker was struck by a vehicle while he was setting up flares and cones at the scene of a semi-trailer fire on Highway 53 south of Bloomer, according to the Wisconsin State Patrol. Zunker died the next day at the age of 31 from head injuries sustained as a result of the incident. While he was wearing his department issued winter jacket, he was not wearing his department issued reflective vest.
Safety Precautions for Responders On Or Near Roadways
The work environment for Emergency Medical Responders (EMRs) is a dynamic environment with constantly changing conditions. Working on and near roadways is no exception as the 2008 incident in Chippewa county Wisconsin presents. Responders need to be monitoring the scene for safety hazards when enroute to a call, when arriving to the scene, and constantly when working at the scene. Ideally, a roadway would be shut down and the traffic hazard eliminated, but this is not always the most desirable solution to the problem, so it requires using other forms of hazard reduction strategies such as establishing control areas at an emergency scene, creating physical barriers between the hazard and the responders, or using Personal Protective Equipment (PPE) to reduce hazard exposure.
[Need to add this reference link:
https://wisconsindot.gov/Documents/about-wisdot/who-we-are/dtsd/bto/etcsmguidelines2016.pdf
EMRs may be arriving at a roadway incident in their personal vehicles or an authorized emergency vehicle like an ambulance or rescue squad. The vehicle can be used as a form of notification about the emergency scene to traffic and as a protection barrier for the patient and responders. The vehicle can be parked before the incident with emergency lighting devices activated to alert travelers to the emergency incident. Additionally, by positioning the vehicle before the incident, the vehicle assists in providing a physical barrier between the traffic and the incident scene. This can help protect the responders, the patient, and the well-meaning passerby that gives too much attention to the incident and not enough attention to staying on the roadway.
Authorized emergency vehicles are equipped with multiple colors of flashing, rotating, or oscillating lights. These assist in increasing visibility of the vehicle to permit travel time to react to the incident, potentially slow down, and/or change lanes of travel. Authorized emergency vehicles are also frequently equipped with bright colored graphics and reflective material to increase visibility when the emergency lighting is not activated. There is a Federal Standard, the KKKK-A-1822F standard that defines the requirements for emergency lighting and the use of the Star of Life emblem. Also, Wisconsin Transportation Administrative Code Chapter 309 (Trans. 309) defines some of the exterior lighting and marking requirements for ambulances such as the requirement for a 4” of reflective striping around each side of the ambulance. Also, Trans. 309 requires at least 6” lettering of “Ambulance” or “Rescue Squad” to be on each side and the rear of the ambulance. These letters do not need to be reflective, but it is preferred.

While the benefits of using vehicles to assist responders have been presented, the responder also needs to be aware that their parked vehicles also create additional distractions and hazards for travelers on the roadway. Wisconsin statute 346.03 defines the requirements for when an authorized emergency vehicle is stopped, standing, or parked on a roadway to help protect both the emergency responders and the other travelers on the roadway.
When exploring the hierarchy of risk controls, using PPE is the least desirable method to protect from hazards as they require the wearer to be within the hazardous environment (CDC, 2024). However, the ever-changing emergency environment creates a situation where it is difficult to remove all potential hazards. So, emergency responders should consider PPE for the various work environments and hazards they may be exposed to. The PPE for roadway incidents will include a reflective vest or jacket meeting the requirements of the Federal Highway Administration’s Worker Visibility Rule. This rule was enacted to help protect those working at emergency incidents and those traveling through the scene.
Major Phases of an Ambulance Call
An ambulance call is a complicated process. When examining it from the untrained eye, it seems like a superhuman feat that is accomplished by people possessing abilities above many others. While we may feel superhuman at times, the process is complex but can be broken down into more manageable phases to assist in preparing for the call and completing each incident response effectively. Prior to a request for service call being initiated, the EMR should be mentally and physically preparing themselves and their equipment. If working “on-shift”, the EMR should be dressed for the weather of the day and demonstrating proper personal hygiene. They should perform an ambulance and equipment inspection at the beginning of their shift to ensure their equipment is all stocked, maintained, and in ready-to-use condition should a patient need it. Many EMRs work in volunteer or paid-on-call services that do not have personnel “on-shift” to perform a daily inspection. These services may elect to perform monthly or weekly checks of their vehicle and equipment in addition to restocking any used supplies after each call.
With the EMR, their vehicle, and their equipment ready for whatever the community may need or the day may face, they are ready to be in service to receive dispatch requests for service. The dispatch information is one of the first steps for assisting the EMR in developing their patient impression of what this call is going to entail. At the time of dispatch, the EMR needs to record the address of the incident, patient chief complaint or nature of the call, and any specific instructions dispatch provides such as where to locate the patient, already identified scene hazards, or response instructions. After accurately gathering this information, the EMR or crew can respond. If there are questions about the information, now is the time to clarify it with dispatch; it does not benefit the patient to have the ambulance headed to an incorrect address or without the proper equipment and resources.

While responding to the incident each EMR needs to ensure they are traveling safely and operate their vehicle with due regard for all others on the roadway. While driving, it is important to maintain a sense of situational awareness and provide attention to the task at hand. Ideally, there will be multiple crew members so the driver can focus on driving and the other team members can assist with road hazard identification, navigation, or preparing for scene arrival and the patient encounter. The importance of traveling safely cannot be understated. The responders are not able to provide care if they get into an accident and never arrive on scene, or worse, if they are injured or others are injured requiring additional emergency resources to come to their aid.
As mentioned earlier, Wisconsin statute 346 explains what an authorized emergency vehicle is and what exemptions authorized vehicles are provided within the statutes. The statutes also emphasize that these statute exemptions still require the emergency vehicle driver to operate with due regard for all on the roadway. Privately owned personal vehicles may, or may not, meet the requirements for being an authorized emergency vehicle. If the vehicle does not meet the requirements for being an authorized emergency vehicle, the vehicle and driver do not have an exemption from standard traffic laws and must follow all typical traffic laws.
It is recommended that each organization have a Standard Operating Procedure (SOP) or other protocol to assist in determining what patient complaints or incident types allow the emergency vehicle driver to exercise the statutory driving exemptions. Many organizations use a dispatch screening process to gather additional information about the incident and categorize the patient’s injury or illness to determine what level of response should occur. This provides objective information on how the emergency team should respond. If the criteria for exercising authorized emergency vehicle exemptions is met, Wisconsin statutes do permit the vehicle to stop, stand, or park against traffic laws if the emergency visual warning lights are activated.
Then, when using both the visual warning lights and the audible siren, the authorized emergency vehicle may proceed past a red or stop signal or stop sign, but only after slowing down as may be necessary for safe operation. Also, they may exceed the speed limit, and/or disregard regulations governing direction of movement or turning in specified directions. Note that these last exemptions do require both the visual warning lights and the audible warning siren to be activated to exercise the exemption and department SOP may have additional restrictions.
When arriving at the scene, position the vehicle to protect the scene if this is a roadway incident. Turn the front wheels away from the incident scene. This ensures that if the responder’s vehicle is rear-ended and forced forward that it will move away from the scene instead of into it. If the incident is not a roadway incident, consider patient loading and the need for other additional resources at the scene and position and park (stage) the vehicle accordingly. Before exiting the vehicle, scan the scene for hazards like leaking fuel, electrical hazards, traffic, or fire. When accessing the patient(s) consider the potential need for additional resources and maintain situational awareness as you develop your first impressions of the patient and scene.
In the event the incident does not result in transporting a patient, you will have discretionary time to ensure safe backing or repositioning of the emergency as you return to service, so use it. Consider the need for any supplies that might need to be stocked prior to returning to service. Consider a hypoglycemic diabetic patient that used your supply of glucose, then refused transport. It may be desired to ensure your equipment is resupplied before returning to service as the next call may be another hypoglycemic diabetic patient and you would not be prepared to care for the patient. Consult your local protocols for guidance on when to return to service.
View the following YouTube videos for two examples of how EMRs spend their shifts, noting how they spend down time:
If the incident results in a patient transport to the hospital, your agency may have guidance to specify when emergency vehicle exemptions are used, and the patient is transported using emergency lights and sirens. The driver of the ambulance will frequently need to reset the odometer to track transport mileage, or use a mapping application, and notify dispatch of the transport destination. If the patient condition changes while transporting to the hospital, it may necessitate redirecting to a closer facility and dispatch should again be notified of the change in destination facility.
While transporting, it is common practice to provide a patient care report to the receiving hospital. This assists the hospital staff in preparing for the incoming patient and calling upon any additional resources that they feel might be needed such as stroke alert team or a trauma surgical team. Ideally the patient care report is provided by the EMS provider attending to the patient so the driver can focus on the task of driving. However, with an extremely critical patient, the EMR in the patient compartment may be busy providing care and may ask the driver to share a brief report with the receiving hospital.
When arriving at the destination hospital, the driver should notify dispatch. Most hospitals have an ambulance parking area that is easily accessible for larger vehicles and protected from Wisconsin’s weather. The driver should park the vehicle in a location that allows for ease in accessing the rear of an ambulance for patient removal. If in a garage and the patient’s condition permits, consider taking the time to close garage doors to protect the patient from the weather and onlookers prior to unloading them from the ambulance. The patient is then unloaded from the ambulance and transported to the designated hospital area with a patient care update report provided at the time of transfer to the hospital staff.

The ambulance crew should discuss when to return to service as they may need supplies, or the ambulance or equipment may need disinfection. The crew should consult with each other and follow any local protocols for returning to service. Also, when returning to the station from a call, the crew needs to abide by all traffic laws. When returned to the station, they should resupply the ambulance with any equipment that was used, damaged, or found missing while on the previous call. Consumables like oxygen and medications should be checked to ensure the ambulance still has an adequate supply. Also, any equipment that may have been exposed to potentially infectious agents should be cleaned. Last, as the saying goes, the call is not over until the report is submitted so the patient care report should be completed and submitted according to local protocol.
Post Run Actions
In addition to resupply and patient care report documentation, proper cleaning and disinfection needs to occur. If the EMR has potential infection agents on themselves or their clothing, their personal disinfection becomes the priority over the vehicle or equipment. The EMR may need to change clothing and/or shower to prepare themselves to return to service. Also, if an exposure to potentially infectious body fluids occurred during the call, be sure to inform your supervisor and the destination hospital staff.
Just as PPE is used for providing patient care, PPE should be used when cleaning equipment to include eye protection from splashes. There are several cleaning chemicals used for cleaning and disinfecting EMS vehicles and equipment. Review the specific chemical instructions to ensure it is safe to use on the surface to be disinfected (such as clothing or fabric EMS jump bags). Then, also review what protections the user needs to have to use the chemical such as gloves, glasses, or goggles. Last, each chemical will have a different amount of time that it needs to be exposed to a surface to adequately disinfect. So, review the directions and ensure that you are allowing for adequate disinfection.
17.3 Ambulance Operations
Learning Objectives
- Describe common equipment locations on an ambulance
- Demonstrate warning devices on an ambulance
- Demonstrate ambulance maintenance
- Demonstrate ambulance cot operations
- Demonstrate common equipment locations on an ambulance
14-years after he was paralyzed while responding to a July, 2003 car crash, an EMT from the Mosinee Fire Department has died. Matt Deicher suffered his paralyzing injuries when his ambulance overturned on I-39 while Matt was working in the patient care compartment. He and his crew were rushing a motor vehicle collision patient to the hospital at the time of the ambulance roll over. A police accident report noted excessive speed, poor weather conditions, and bad tires as contributing factors in the crash that left Deicher without feeling below his neck. The patient they were transporting died in the ambulance roll over.
Warning Devices on an Ambulance
As discussed earlier, each agency should develop protocols for when emergency warning devices are used and when the Wisconsin statutory exemptions are exercised. Emergency lighting does increase visibility of the emergency vehicle to help increase awareness for others in the area. However, these emergency lights do require substantial electricity to power them. Because of this increased power draw on the vehicle’s electrical system, most emergency vehicles use a device called a load sequencer to power on and power down emergency lighting systems over a few second sequence instead of adding and dropping the electrical demand all at once. This helps increase reliability and reduce wear on the vehicle’s electrical system components.
Once in the driver or passenger seat of the ambulance or other authorized emergency vehicle, the EMR switches for each series of emergency lights can be found, usually on the center console. If the vehicle has a load sequencer, there typically is a switch titled “master” or “emergency master”. In the situation of a load sequencer or “emergency master switch”, each individual emergency light switch can be left in the “on” position. Then, just the “emergency master” switch can be turned on when the emergency lighting system is desired. The load sequencer will power on the individual light circuits as vehicle power becomes available. Conversely, when desiring to turn off the emergency lights, the user can just turn off the “emergency master” switch and the individual circuits will power down.
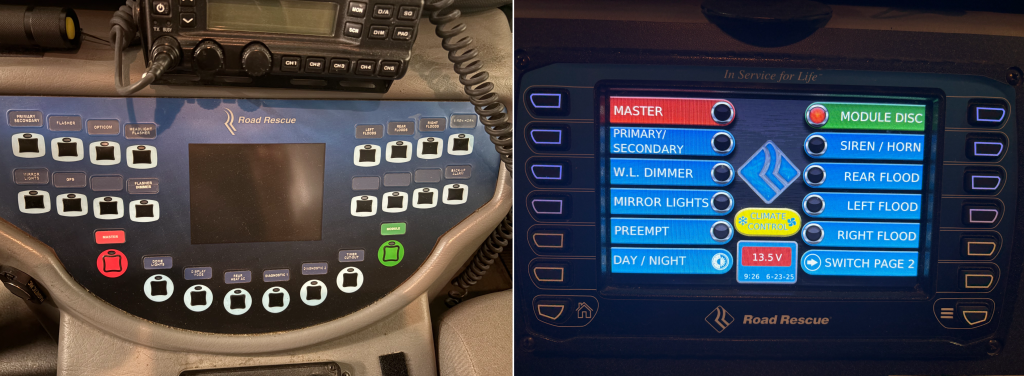
If the vehicle does not have an emergency master switch, the user will need to power on each of the individual emergency lighting switches. If time permits, it would be ideal to wait a second between powering each switch to allow the vehicle’s electrical system to compensate for the added demand; this is accomplishing a similar function to that of a load sequencer. Also, when powering down the emergency lighting system, consider waiting a second between turning off each individual lighting switch, if time permits.
Demonstrate Ambulance Maintenance
Most agencies will have a mechanic to service their emergency vehicles or work with a repair shop to service the vehicles. While the vehicles are mechanically similar to the common passenger cars and trucks used to drive to work each day, they are used in more challenging environments, are much heavier, and are not always driven with the same gentleness. As such, routine maintenance of vehicles is important.
Wisconsin Trans. 309 defines the requirements for an ambulance and the inspection process performed on an ambulance. The form the state’s ambulance inspector uses is called the SP4161 form and is accessible through an internet search or by contacting your local State Patrol office. This form can be useful when performing a thorough ambulance inspection to ensure your vehicle is complaint and ready to render aid to those in need.
View, download, or print a copy of the SP4161 form PDF.
Part of the vehicle rig check may include checking fluid levels including engine oil, transmission fluid, brake fluid, power steering fluid, and windshield washer fluid. The operator should monitor fluid leaks and keeping ambulance bay floors clean can help with this. So, when a vehicle starts experiencing a fluid leak, the operators can quickly identify the leak and monitor the severity of the leak. The process to complete these tasks varies significantly by manufacturer and it will be nearly impossible to describe each possible make, model, and year of emergency vehicle that your agency might have. Because of this, refer to your specific vehicle’s owner’s manual for the process to check these fluid levels. The owner’s manual will also define the fluid and filter replacement schedules to ensure your agency’s emergency vehicles are properly maintained.
Monitoring tire pressure and wear are very important to safe vehicle operation. This is also a task that can be accomplished by the EMR. The Wisconsin Trans. 309 code requires that tires have at least 1/8” of tire tread depth measured in two spots. Tire tread depth gauges can be purchased online or at most tire retailers. The specified pressure for the vehicle’s tires is usually listed on the vehicle inside the driver’s door frame. Maintaining proper tire pressure and tread helps ensure safe vehicle operation.
Demonstrate Ambulance Cot Operations
Ambulance cots have evolved significantly in recent years in an effort to reduce the frequency of back and joint injuries sustained by EMRs when loading and unloading the patient cot. The EMR may have access to manual operating cots, power cots that raise and lower the wheel carriage at the push of a button, or powerlift cots that perform all of the lifting and lowering operations. In addition to the various styles of cots, there are a few primary manufacturers of these cots for EMS. With the different manufacturers, models, and styles, this chapter cannot list the process and safety considerations of each, so the EMR should refer to the owner’s manual for their specific cot make and model for the proper procedures. If the EMR is not able to locate the owner’s manual for their cot, most manufacturers provide this on their website or you should contact their customer service department for a copy.


View the following supplementary YouTube videos to see how these devices are used:
- Lifting Mechanics and How to Operate the Stretcher
- This is a different model of stretcher: Stretcher Use and Movement
- Stryker Stair Chair Tutorial
- This is a different model of stair chair: How Operate the Stairchair (EMT Skill)
- LTC EMS Program’s channel provides skill video demonstrations of tasks like stretcher use and movement.
Demonstrate Common Equipment Locations on an Ambulance
Each emergency vehicle or ambulance will be configured differently; however, it is the EMR’s responsibility to learn the vehicle and where to locate important equipment. For example, an ambulance will have a large oxygen cylinder for providing oxygen therapy to patients during transport. The main oxygen cylinder is most often located behind the driver’s area in a rear compartment. However, if your vehicle has this located elsewhere, it is important to become familiar with its location. Also, smaller oxygen cylinders and delivery devices are frequently located together in an oxygen jump bag with regulator. Each EMR should identify at least one source for a portable oxygen cylinder, regulator, and delivery devices such as nasal cannula or partial rebreather mask on their response vehicle.
An emergency equipment “jump bag” includes much of the equipment the EMR will need to manage the first few minutes of common calls. This allows the EMR to enter a safe scene with the emergency bag and begin assessing and treating the patient while an EMR partner or other responder could acquire more complicated supplies, patient movement equipment, or immobilization devices from the ambulance.
Medical supplies and medications may be kept in the emergency jump bag, or they may be secured on the ambulance. Each agency will have its own process for how they store these items. However, the EMR needs to know where to locate these and should periodically check the medical supplies and medications for potential damage or expiration. Like medical supplies, trauma supplies such as bandages, splints, orthopedic scoop stretchers, long spine boards, or cervical collars will be stored throughout your emergency vehicle. When reading this chapter in class, consider reaching out to someone with your ambulance service to go through your ambulance and help you to locate these items on your primary response vehicle. When working with this individual, ask them to demonstrate the operation of the portable and onboard suction units and the specific cardiac monitor/ AED that your agency uses. If you are not yet affiliated with a service, ask your course instructor if there is an ambulance at the college or training center you would be able to go through to locate these items.
17.4 Incident Management
Learning Objectives
- Explain the purposes for establishment of both the National Incident Management System and Incident Command System
- Identify responsibilities of EMR Units in the Incident Command Structure
- Discuss the responsibilities of state and federal resources in the Incident Command System
National Incident Management System and Incident Command System
The current Wisconsin training curriculum for EMR license requires students to meet the training requirements of FEMA ICS-100 Introduction to the Incident Command System and IS-700 National Incident Management System, an Introduction. EMR instructors will frequently assign these independent study courses as homework to complete outside of class. Students can then provide their completion certificates to your instructor for verification. As such, much of this section may be redundant with the information you completed during these independent study FEMA classes but is included for your quick reference and to reinforce the concepts presented by FEMA.
National Incident Management System (NIMS) is the culmination of more than 40 years of efforts to improve interoperability in incident management. This work began in the 1970s with local, state, and Federal agencies collaborating to create a system called Firefighting Resources of California Organized for Potential Emergencies (FIRESCOPE). Under Homeland Security Presidential Directive #5 (February 2003), the Federal government created the National Incident Management System (NIMS). This system directed the creation of a comprehensive, national approach to incident management. Recognizing the value of these systems, communities across the Nation have adopted NIMS. The most current revision of NIMS was released in October 2017.
NIMS Management Characteristics
The following characteristics are the foundation of incident command and coordination under NIMS and contribute to the strength and efficiency of the overall system:
- Common terminology
- Modular organization
- Management by objectives
- Incident action planning
- Manageable span of control
- Incident facilities and locations
- Comprehensive resource management
- Integrated communications
- Establishment and transfer of command
- Unified command
- Chain of command and unity of command
- Accountability
- Dispatch/deployment
- Information and intelligence management
Common Terminology
NIMS establishes common terminology that allows diverse incident management and support organizations to work together across a wide variety of functions and hazard scenarios. This common terminology covers the following:
- Organizational Functions: Major functions and functional units with incident responsibilities are named and defined. Terminology for incident organizational elements is standard and consistent.
- Resource Descriptions: Major resources including personnel, equipment, teams, and facilities are given common names and are typed to help avoid confusion and to enhance interoperability.
- Incident Facilities: Incident management facilities are designated using common terminology.
Modular Organization
ICS and Emergency Operations Center (EOC) organizational structures develop in a modular fashion based on an incident’s size, complexity, and hazard environment. Responsibility for establishing and expanding ICS organizations and EOC teams ultimately rests with the Incident Commander (or Unified Command) and EOC director. Responsibility for functions that subordinates perform defaults to the next higher supervisory position until the supervisor delegates those responsibilities. As incident complexity increases, organizations expand as the Incident Commander, Unified Command, EOC director, and subordinate supervisors delegate additional functional responsibilities.
Management by Objectives
The Incident Commander or Unified Command establishes objectives that drive incident operations. Management by objectives includes the following:
- Establishing specific, measurable objectives
- Identifying strategies, tactics, tasks, and activities to achieve the objectives
- Developing and issuing assignments, plans, procedures, and protocols for various incident management functional elements to accomplish the identified tasks; and
- Documenting results against the objectives to measure performance, facilitate corrective actions, and inform development of incident objectives for the subsequent operational period.
Incident Action Planning
Coordinated incident action planning guides incident management activities. IAPs represent concise, coherent means of capturing and communicating incident objectives, tactics, and assignments for operational and support activities. Every incident should have an action plan; however, not all incidents need written plans. The necessity for written plans depends on incident complexity, command decisions, and legal requirements. Formal IAPs are not always developed for the initial operational period of no-notice incidents. However, if an incident is likely to extend beyond one
operational period, becomes more complex, or involves multiple jurisdictions and/or agencies, preparing a written IAP becomes increasingly important to maintain unity of effort and effective, efficient, and safe operations. Staff in EOCs also typically conduct iterative planning and produce plans to guide their activities during specified periods, though these are typically more strategic than IAPs.

Manageable Span of Control
Maintaining an appropriate span of control helps ensure an effective and efficient incident management operation. It enables management to direct and supervise subordinates and to communicate with and manage all resources under their control. The type of incident, nature of the task, hazards and safety factors, experience of the supervisor and subordinates, and communication access between the subordinates and the supervisor are all factors that influence manageable span of control. The optimal span of control for incident management is one supervisor to five subordinates; however, effective incident management frequently necessitates ratios significantly different from this. The 1:5 ratio is a guideline, and incident personnel use their best judgment to determine the actual distribution of subordinates to supervisors for a given incident or EOC activation.
Incident Facilities and Locations
Depending on the incident size and complexity, the Incident Commander, Unified Command, and/or EOC director establish support facilities for a variety of purposes and direct their identification and location based on the incident. Typical facilities include the Incident Command Post (ICP), incident base, staging areas, camps, mass casualty triage areas, points-of-distribution, and emergency shelters.
Comprehensive Resource Management
Resources include personnel, equipment, teams, supplies, and facilities available or potentially available for assignment or allocation. Maintaining an accurate and up-to-date inventory of resources is an essential component of incident management.
Integrated Communications
Leadership at the incident level and in EOCs facilitates communication through the development and use of a common communications plan, interoperable communications processes, and systems that include voice and data links. Integrated communications provide and maintain contact among and between incident resources, enable connectivity between various levels of government, achieve situational awareness, and facilitate information sharing. Planning, both in advance of and during an incident, addresses equipment, systems, and protocols necessary to achieve integrated voice and data communications.
Establishment and Transfer of Command
The Incident Commander or Unified Command should clearly establish the command function at the beginning of an incident. The jurisdiction or organization with primary responsibility for the incident designates the individual at the scene responsible for establishing command and protocol for transferring command. When command transfers, the transfer process includes a briefing that captures essential information for continuing safe and effective operations, and notifying all personnel involved in the incident.
Unified Command
When no one jurisdiction, agency or organization has primary authority and/or the resources to manage an incident on its own, Unified Command may be established. In Unified Command, there is no one “commander.” Instead, the Unified Command manages the incident by jointly approved objectives. A Unified Command allows these participating organizations to set aside issues such as overlapping and competing authorities, jurisdictional boundaries, and resource ownership to focus on setting clear priorities and objectives for the incident. The resulting unity of effort allows the Unified Command to allocate resources regardless of ownership or location. Unified Command does not affect individual agency authority, responsibility, or accountability.
Chain of Command and Unity of Command
Chain of command refers to the orderly line of authority within the ranks of the incident management organization. Unity of command means that each individual only reports to one person. This clarifies reporting relationships and reduces confusion caused by multiple, conflicting directives, enabling leadership at all levels to effectively direct the personnel under their supervision.
Accountability
Effective accountability for resources during an incident is essential. Incident personnel should adhere to principles of accountability, including check-in/check-out, incident action planning, unity of command, personal responsibility, span of control, and resource tracking.
Dispatch/Deployment
Resources should be deployed only when appropriate authorities request and dispatch them through established resource management systems. Resources that authorities do not request should refrain from spontaneous deployment to avoid overburdening the recipient and compounding accountability challenges.
Responsibilities of the EMR Units in the Incident Command Structure
The same sections of the traditional ICS structure are used within the EMS System. These sections include operations, logistics, planning, and finance/administration.
Operations Section Chief Responsibilities
The Operations Section Chief is responsible for managing all tactical operations at an incident. The Incident Action Plan (IAP) provides the necessary guidance. The need to expand the Operations Section is generally dictated by the number of tactical resources involved and is influenced by the span of control considerations.
Major responsibilities of the Operations Section Chief are to:
- Assure safety of tactical operations.
- Manage tactical operations.
- Develop the operations portion of the IAP.
- Supervise execution of operations portions of the IAP.
- Request additional resources to support tactical operations.
- Approve release of resources from active operational assignments.
- Make or approve expedient changes to the IAP.
- Maintain close contact with IC, subordinate Operations personnel, and other agencies involved in the incident.
Logistics Section Chief Responsibilities
The Logistics Section Chief provides all incident support needs except for logistics support to air operations. The Logistics Section is responsible for providing:
- Facilities.
- Transportation.
- Communications.
- Supplies.
- Equipment maintenance and fueling.
- Food services (for responders).
- Medical services (for responders).
- All off-incident resources.
Major responsibilities of the Logistics Section Chief are to:
- Provide all facilities, transportation, communications, supplies, equipment maintenance and fueling, food and medical services for incident personnel, and all off-incident resources.
- Manage all incident logistics.
- Provide logistical input to the IAP.
- Brief Logistics Staff as needed.
- Identify anticipated and known incident service and support requirements.
- Request additional resources as needed.
- Ensure and oversee the development of the Communications, Medical, and
- Traffic Plans as required.
- Oversee demobilization of the Logistics Section and associated resources.
Planning Section Chief Responsibilities
The Planning Section Chief is responsible for providing planning services for the incident. Under the direction of the Planning Section Chief, the Planning Section collects situation and resources status information, evaluates it, and processes the information for use in developing action plans. Dissemination of information can be in the form of the IAP, in formal briefings, or through map and status board displays. Major responsibilities of the Planning Section Chief are to:
- Collect and manage all incident-relevant operational data.
- Supervise preparation of the IAP.
- Provide input to the IC and Operations in preparing the IAP.
- Incorporate Traffic, Medical, and Communications Plans and other supporting materials into the IAP.
- Conduct and facilitate planning meetings.
- Reassign personnel within the ICS organization.
- Compile and display incident status information.
- Establish information requirements and reporting schedules for units (e.g., Resources and Situation Units).
- Determine need for specialized resources.
- Assemble and disassemble Task Forces and Strike Teams (or law enforcement Resource Teams) not assigned to Operations.
- Establish specialized data collection systems as necessary (e.g., weather).
- Assemble information on alternative strategies.
- Provide periodic predictions on incident potential.
- Report significant changes in incident status.
- Oversee preparation of the Demobilization Plan.
Finance/Administration Section Chief Responsibilities
The Finance/Administration Section Chief is responsible for managing all financial aspects of an incident. Not all incidents will require a Finance/Administration Section. Only when the involved agencies have a specific need for finance services will the Section be activated. Major responsibilities of the Finance/Administration Section Chief are to:
- Manage all financial aspects of an incident.
- Provide financial and cost analysis information as requested.
- Ensure compensation and claims functions are being addressed relative to the incident.
- Gather pertinent information from briefings with responsible agencies.
- Develop an operating plan for the Finance/Administration Section and fill Section supply and support needs.
- Determine the need to set up and operate an incident commissary.
- Meet with assisting and cooperating agency representatives as needed.
- Maintain daily contact with agency(s) headquarters on finance matters.
- Ensure that personnel time records are completed accurately and transmitted to home agencies.
- Ensure that all obligation documents initiated the incident are properly prepared and completed.
Integration of State and Federal Resources
It is not uncommon for an incident to require working collaboratively with other public safety or private entities. For example, a vehicle collision will probably have local law enforcement responding and possibly a fire department if vehicle stabilization or extrication are required. Then, the state patrol may also come if the incident occurs on an Interstate or other large highway. Vehicle towing companies may come to remove vehicles, and the public works or highway department may need to respond to clean up debris or re-route traffic. EMRs should plan for working collaboratively with others.
Larger incidents may result in Wisconsin Emergency Management (WEM) being deployed or potentially the National Guard to assist in support operations. Also, federal resources such as the Department of Homeland Security (DHS) or the Federal Emergency Management Agency (FEMA) could bring in resources. One thing that is unique about Wisconsin is that it is legally organized as a “home-rule” state. With this, the local incident commander has total control to mobilize or demobilize resources as needed. They also maintain control of the incident unless they elect to transfer command or organize a unified command structure.
When calling upon resources from outside the initial organization, these are frequently termed “mutual aid” resources. They are termed this because there are agreements in place for each agency to be able to call upon the other mutually. A system called Mutual Aid Box Alarm System (MABAS) has grown in recent years. One benefit of MABAS is that it permits each agency to pre-determine the mutual aid resources they desire for each type of incident in advance. This makes requesting additional resources easier for both the Incident Commander and the Dispatcher.
When working with any external agency, whether it is the neighboring first responder team or FEMA, it is important to maintain the principles of the Incident Command System in place. When incidents grow in scope is when the benefits of the ICS really shine. So, be sure to keep the concepts of span of control, communications, and unity of command top of mind when an incident begins to grow in size. Multiple Casualty Incidents (MCI) are one example of a situation where the ICS will likely be implemented to support EMS operations.
17.5 Multiple Casualty Incidents
Learning Objectives
- Describe the principles of triage
- Describe the various triage systems
- Discuss the importance of patient tagging and how to use the system when moving patients from triage to treatment
- Discuss the logistics of triage, treatment, and transport numerous patients from a single incident
- Demonstrate triage based on START or SALT Triage Principles
- Demonstrate the movement of patients following Triage to Treatment
- Demonstrate the movement of patients from Treatment to Transport
- Demonstrate the setup of a Multiple Casualty Scene
Principles of Triage
The implementation of triage is required any time an EMR is in a situation where they have more patients than they can effectively care for themselves. The word origins of the term triage are French, and the word refers to the need “to sort”. Triage is exactly this, it is a process where an EMR will rapidly assess each patient and sort them into various categories depending on their injuries and severity. This helps to ensure that limited resources are most effectively allocated. One could appreciate that a screaming child or having a friend as an injured patient might bias an EMR’s perspective on who should receive care first. However, the process of triage ensures that the allocation of treatment care resources is objective in nature to assist the EMR, with limited resources, make the best judgement quickly and gain the greatest benefit for the most people.

Multiple methods and algorithms exist to provide the framework for initial rapid triage of victims of an incident. Currently, the recommendation in Wisconsin is to utilize a triage algorithm meeting the Model Uniform Core Criteria (MUCC) for MCIs. SALT (Sort, Assess, Lifesaving Interventions, Treatment and/or Transport) triage is an evidence-based system and is MUCC compliant. SALT is endorsed by the State of Wisconsin EMS Advisory Board, Physician Advisory Committee, and State Trauma Advisory Council.
Initial triage should occur as soon as the first arriving EMR is able to begin the process at an MCI incident. This allows the triage EMR to rapidly assess the situation, identify resource needs, and request these resources. The prioritization process is dynamic and may be altered by changes in patient condition, changes in available resources, and scene safety.
Reassessment and re-triage of patient condition should occur at each stage of the treatment and transportation process. So, as soon as a patient is relocated to the treatment area, re-triage should occur. In general, treatment and/or transport should be provided for immediate patients first, then delayed, then minimal. Additional prioritization should be done utilizing EMS clinical judgment.
Triage Systems
As mentioned earlier, there are multiple methods of triage. The three that will be presented in this chapter are START, JumpSTART, and SALT. Your agency will likely adopt one of these, or a related triage model. The START triage acronym stands for Simple Triage And Rapid Treatment. The START model assesses:
- The patient’s ability to walk
- The adult patient’s respiratory status (over 30 or under 30 breaths/minute)
- The adult patient’s perfusion status (radial pulse/ delayed capillary refill)
- The adult patient’s mental status (ability to follow directions)
The START triage model algorithm
Access, download, and print your own copy of the START – Simple Triage And Rapid Treatment PDF
The JumpSTART model and acronym recognized the limitations within the standard START algorithm. When assessing the respiratory rate, ability to follow commands, and the perfusion status, the expected results listed are for a mature and unimpaired adult. A child or infant will have vital signs and clinical findings that are different than an adult. So, the JumpSTART algorithm was designed to provide a triage process for pediatric patients.
The JumpSTART model assesses:
- The patient’s ability to walk
- The spontaneous breathing of the patient
- The patient’s respiratory rate (less than 15 or greater than 45)
- The presence of a palpable pulse
- Patient mental assessment using the AVPU acronym
The JumpSTART triage model algorithm
Access, download, and print your own copy of the JumpSTART Pediatric Multiple Casualty Incident Triage PDF
The third triage model this chapter will discuss is the SALT model and algorithm. The SALT model emerged after identifying some potential opportunities for improvement within the START model. For example, the SALT model assigns a gray color to the expectant triage category instead of black like START and JumpSTART do. These are patients that are still alive but are not expected to survive their injuries with the resources available at the incident scene. The SALT model process:
- Starts with global sorting of all patients
- Those patients that are still/ or with obvious life threats
- Those able to perform purposeful movement, like waving their hand
- Those able to walk
- Then, an individual assessment attempts to perform any LSI
- Control major bleeding
- Open airway, attempt two rescue breaths for children
- Auto inject antidotes
- The presence or absence of breathing?
- Next, examine their ability for all of these criteria
- Obeys commands and makes purposeful movement?
- Has a peripheral pulse?
- Not in respiratory distress?
- Bleeding controlled?
- If the patient meets all of the above criteria, the triage EMR needs to assess if the patient has only minor injuries
- If the patient does not meet all of the above criteria, the triage EMR needs to assess if the patient will likely survive with the currently available treatment resources
The SALT triage model algorithm
Access, download, and print your own copy of the SALT Mass Casualty Triage PDF
Criteria of Patient Tagging (Color System)
The purpose of a triage system is to sort (triage) the numerous patients at a multiple casualty incident. In sorting, there must be end categories or buckets that the goal is to sort the patients into. Each triage model has similar categories and color codes these categories for more rapid identification at an MCI scene.
- Green= Minor/ Minimal
- Patients with relatively minor injuries
- Their condition is not likely to deteriorate over time
- They may be able to assist in their own care, oftentimes termed the walking wounded
- Yellow= Delayed
- Patient’s transport can be delayed
- Includes serious injuries and potentially life threatening injuries, but their condition is not expected to deteriorate over several hours.
- Red= Immediate
- Patient can be helped by immediate intervention and transport
- Condition requires medical attention within the first 60 minutes for survival
- Includes compromises to Airway, Breathing, and Circulation
- Expectant: Black (START) or Gray (SALT)
- Victim unlikely to survive with the severity of their injuries, available care resources, or both
- Provide supportive care as resources are available
- Dead: Black (SALT)
- Patients that have already succumb to their injuries
Moving Patients from Triage to Treatment
Once the patients have received initial triage, they should be moved to the treatment area based on their triage category. The EMRs or others assisting in extricating the patients to the treatment area should start with Red triaged patients, then Yellow, then Green, then Gray/Black. If there are delays in gaining access to a more severe patient, the responder should continue with moving the next category of patient to the treatment area. For example, if a Red patient is trapped in a vehicle and extrication will take a few minutes, the team could begin moving Yellow or Green patients to the treatment area to remain productive. Oftentimes, law enforcement or fire service personnel can assist with extricating patients to the treatment area so the EMS personnel can remain dedicated to triage, treatment, and transporting patients.
Once in the treatment area, re-triage should occur, and the patient should be assigned to whatever category the re-triage assessment assigns as their condition may have deteriorated since initial triage. Within the treatment area, EMS staff should begin treating patients with the resources they have available, starting with those that are triaged the most severe. Then, as patients are transported, treatment will transfer down to the less serious triage categories until all patients have been treated and transported.
Moving Patients from Treatment to Transport
The goal of any MCI is to do the most amount of good for the most patients. As resources arrive at the scene, getting the patients to definitive care is important. So, once triage and treatment resources are adequate and established, the transportation group should be created and begin transporting patients to hospitals based on their severity. The transportation group needs to determine what transport ambulances will take each patient and what hospitals would be best suited for each patient. An MCI can easily overwhelm a small rural hospital. So, transportation should consider this and seek out alternate facilities or consider aeromedical or ALS intercepting resources too. The Wisconsin Department of Health shares the following guidance to assist the transport group:
- Patients with the most immediate need of trauma care should be prioritized for transport to the closest Level 1 or Level 2 trauma center, please refer to trauma triage guidelines.
- In general, Level 3 trauma centers have general and orthopedic surgery, and may have other subspecialities such as neurosurgery. IC should request available resources and capabilities from the Level 3 trauma centers to help guide decisions.
- Level 4 trauma centers can provide stabilization and advanced trauma life support to patients. IC should request available resources and capabilities from Level 4 trauma centers to help guide decisions.
- Preferentially transport pregnant patients to facilities with labor and delivery services.
- Preferentially transport pediatric patients to facilities with inpatient pediatric capability
The treatment group frequently assumes tracking duties, if resources are not adequate to assign someone specifically for tracking. The purpose of tracking is to account for all patients. Tracking will make note of each patient by name or triage tag number, which ambulance transported them, and what facility they were transported to. This is an important step to account for all patients and to assist with the follow up documentation that will be needed for patient care reporting.
Components of a Multiple Casualty Incident
The triage area will be at the location of the patients, or the safest area close to the patients in the event of a fire or other hazardous situation where EMS triage personnel are not able to immediately access the patients. The treatment area should be located close to the incident so extricating patients from the scene to treatment does not create an undue burden. However, the treatment area should be accessible to vehicles, so ambulances are able to also quickly acquire their patient and begin transport. It is not uncommon to have treatment located between the scene and the first open roadway. Treatment areas will oftentimes have large color coded tarps that correspond to the patient’s triage category and color. This assists arriving responders to rapidly identify the most seriously injured patients and render aid or transport. The transport area needs to be accessible for ambulances. So, maintaining an open path for emergency vehicles is important. It is common to have one route into the transport area and a different route out to keep the flow of vehicles moving in a cyclical fashion. Aeromedical rotary wing (helicopter) capabilities and landing zone requirements will be presented in the next section. However, this is one consideration for an MCI event as these resources can rapidly transport patients to specialty care facilities and reduce the burden on local facilities. An MCI incident will have media personnel arriving to share the news about the incident. The Incident Commander should identify a media area. If the incident is a potential crime scene, law enforcement will likely not want the media or others to be within the crime scene and law enforcement can be a useful tool for securing a location for media to effectively work from.
| Checklist | Tasks |
|---|---|
| Arrival | Park vehicle and position yourself and other responders upwind and upgrade and at a safe distance. |
| First-in Report |
|
| Establish Command |
|
| Incident Assessment |
|
| Initial Actions | The first EMS crew is to begin the process of triage and patient care activities as appropriate for the circumstances once area deemed safe to enter |
17.6 Air Medical Operations
Learning Objectives
- Discuss situations when air medical transport should be considered.
- Discuss the advantages and disadvantages of air medical transport
- Describe the safety procedures and guidelines for setting up a landing zone
Consideration of Air Medical Transport

Air medical transport is a great resource and component of the EMS system. Air medical transport may be fixed wing airplanes or rotor wing helicopters. Fixed wing aircraft are more common for long transport to other states or countries. Rotor wing helicopter air medical operations are more common for the EMR as rotor wing aircraft can land in remote areas at improvised landing zones. They provide the benefits of Advanced Life Support care and rapid transport to specialty care facilities. Each agency will have their own criteria for requesting air medical resources; however, the Wisconsin Department of Health provides this guidance for when to consider requesting Helicopter EMS (HEMS):
- High-Risk Auto Crash
- Partial or complete ejection
- Significant intrusion (including roof)
- >12 inches occupant site OR
- >18 inches any site OR
- Need for extrication for entrapped patient
- Death in passenger compartment
- Child (Age 0–9) unrestrained or in unsecured child safety seat
- Vehicle telemetry data consistent with severe injury
- Rider separated from transport vehicle with significant impact (for example, motorcycle, ATV, horse) or reported high speed crash
- Pedestrian/bicycle rider thrown, run over, or with significant impact
- Fall from height > 10 feet (all ages)
- Large animal (rodeo, horse, bull, etc.) related injuries
- Altered mental status or unconsciousness in setting of trauma
- Serious burns or injuries from an explosion
- Any penetrating injury to abdomen, pelvis, chest, neck, or head (gunshot, knife wound, industrial accident)
- Crushing injuries to abdomen, chest, or head
- Drowning patients
- Any incident where signs indicate that a person may be seriously injured, and the reporting party/caller is not able to clearly relay the necessary information
- Any event with three or more critically injured patients
- Seriously ill or injured patient in an inaccessible area
Air medical services can be requested by contacting them directly or by coordinating a request through dispatch. When requesting HEMS, the EMS agency should also request an area fire department or other rescue service to assist with setting up the improvised landing zone. This ensures that EMS personnel can focus on providing patient care while other responders provide landing zone and helicopter safety support.
Advantages and Disadvantages of Air Medical Transport
HEMS comes with its own array of advantages and disadvantages. There is no perfect situation so the EMR should consider the guidance provided earlier for when to request HEMS. Some advantages of HEMS are:
- More rapid transport to specialty care facilities
- Faster
- Fly over roadway congestion
- Provide care resources (ALS) when those resources are not otherwise available
- Staffed with paramedics, nurses, or physicians
- Better patient experience for long transport times between hospitals
- Support transport for geographically isolated areas (Apostle or Washington islands in Wisconsin for examples)
- Additional support resource during MCI events
Some disadvantages to HEMS include:
- Cost to patient is increased
- Weather dependent (blizzards, other severe weather that impacts visibility)
- Potential need to establish an improvised landing zone
- Some flights can be weight dependent
- Safety concerns associated with the helicopter
Set Up a Fully Operational Landing Zone
Requesting HEMS will require establishing an improvised landing zone if a predetermined and established landing zone is not readily accessible. A landing zone commander should be assigned to communicate with the helicopter and manage landing zone setup and safety. When selecting the location for the landing zone, first assess the wind direction. The helicopter would prefer to approach and take off into the wind. So, there should not be any tall obstructions impacting the route into and out of the landing zone. Second, the landing zone should be a flat surface at least 100 feet by 100 feet. The surface should be solid ground, (not a frozen lake) that is not muddy, and does not have tall grass. The landing zone space and surrounding area should be free of unsecured debris that could become airborne as the helicopter approaches and departs. The helicopter can generate winds exceeding 60 miles per hour. So, clean up or secure items that could become airborne. Assess the area for overhead obstacles like power lines, towers, or other objects that may be difficult for the pilot to see and make note of these for the landing zone commander to share with the flight crew before they begin their approach.
When establishing the improvised landing zone, mark each corner with a large traffic cone during the daytime or a small strobe light at nighttime. Establish perimeter control by placing a responder with helmet and eye protection on each side of the landing zone to keep everyone out of the landing zone. After the helicopter lands, do not approach the helicopter, the flight team will approach the ground personnel. If you are tasked with approaching the helicopter to assist with loading the patient, remember the overhead main rotor and tail rotor may still be rotating although not visible. So, stay low and away from these rotors. Also do not shine lights upward or at the helicopter as it is landing as this can obscure the pilot’s vision.
View the following YouTube video to see a considerations and a demonstration for setting up an improvised landing zone: Landing Zone Safety Full Training Final
17.7 Patient Extrication
Learning Objectives
- Discuss how dispatch information can be utilized to anticipate obstacles to patient access
- Discuss the performing a scene size-up of a crash scene and how to utilize those findings for patient assessment
- Describe the role of an EMR while a patient is entrapped within a vehicle
- Explain actions and techniques that may be required to gain access to patients in residential, commercial, or industrial scenes.
- Demonstrate scene size-up on simulated motor vehicle crash scene
- Demonstrate vehicle stabilization techniques
- Discuss the terms and demonstrate the equipment and techniques of the extrication process
Using Dispatch to Anticipate the Scene
As soon as the EMR is dispatched for a vehicle collision, they can begin the mental preparation and planning for the incident. The EMR can be thinking about the exact location (if they are familiar with it), what the weather and road conditions are like, where they might be transporting to if the patient needs a trauma center, what additional resources they might need and where they would request them from. Dispatch may share the number and types of vehicles involved and the number of and severity of patients too, if they have that information. If the incident is occurring in a high volume or higher speed area such as an interstate, it may be advantageous for emergency services to block lanes of traffic or close the roadway to ensure safe operations at the scene.
Scene Size-Up of a Motor Vehicle Collision
When arriving at the incident scene, the EMS personnel should begin assessing the scene for hazards. Has traffic been slowed or diverted to operate safely at the scene? Are any vehicles on fire? Are hazardous materials involved or is fuel leaking from a vehicle? Are any of the vehicles high-voltage electric vehicles? After arriving at the scene, putting on their PPE to include a reflective vest, and ensuring there are no hazards present, one member of the EMS team should perform a 360-degree scene survey. This practice is common with fire and rescue personnel but is not as commonly performed by EMS personnel. The 360-degree survey involves walking around the entire accident scene to check for hazards, patients, and other potential concerns that could impact scene operations.
With this survey completed, the EMS personnel should be aware of all current scene hazards and be able to communicate them or resolve them to make the scene safe. Also, all patients should be located and rapidly triaged for injury severity. Always consider the risk of a patient being ejected from a vehicle. If ejected from a vehicle, the patient may not be in the immediate accident scene, or they could be trapped under a vehicle. Also, patients may be trapped inside a vehicle and not easily visible. Ask vehicle occupants if anyone else was in the vehicle with them. The EMS team can now request additional resources to assist with scene management, fire or hazardous materials concerns, vehicle stabilization or patient extrication needs, or additional ground ambulance, helicopters, or ALS intercepts.
Vehicle Supplemental Restraint Systems (SRS) and airbags create an additional potential hazard to the patient and emergency personnel. These airbag and restraint systems use small explosive charges to either apply tension to the restraint system or inflate the airbag. If the vehicle extrication process damages one of these devices, they may detonate causing both surprise and potential injury. One practice to reduce this risk is to remove all interior plastic or check underneath the plastic moldings before applying powerful extrication tools to an area of the vehicle.
During the 360-degree scene survey, the EMR should be attentive to locating all patients. Clues like a hole in the windshield or open side windows may have permitted a patient to be ejected from the vehicle. Consider having a later responding EMS personnel repeat the 360-degree survey using a larger circle to potentially locate other patients or hazards.
Role of the EMR with an Entrapped Patient
Caring for the patient may be delayed if the EMS personnel need to wait until the scene is made safe through resolving downed power lines, stabilizing a vehicle, isolating the vehicle’s electrical power supplies, or patching a leaking fuel tank, or containing fuel spill runoff. This emphasizes the need to request additional resources early. Also, once the scene is made safe, the EMR will then be able to access the patient; however, this will likely come with some challenges if a patient is entrapped within a vehicle.
Gaining Access to the Patient
The simplest method for gaining access to a patient is through the vehicle doors. In the perfect world, the door closest to the patient would be undamaged, unlocked, and open easily. However, this may not be the case. So, the EMR may need to gain access to their patient through a different door and then move within the vehicle to their patient. When working inside the vehicle and working to access the patient, there will be additional hazards like electrical wiring, pressurized gas cylinders, sharp metal or glass that could injure an EMR without the correct PPE. So, the EMR should ensure they have a helmet, gloves, protective clothing, and eyewear to help protect themselves from.
In the event no door is accessible, the EMR may then try to gain access to the patient through a window. If it is summer and the windows are open, this is easier. If it occurs during the 11.5 months of winter in Wisconsin (just a Wisconsin joke), the EMR will need to break the glass to gain access. The side windows on vehicles are made of tempered glass. This tempered glass can be broken using a sharp object or a spring-loaded center punch pressed into a lower corner of the window. Before breaking the glass, inform the vehicle occupants what you are doing. Consider breaking a window far away from the patient to not risk shattered glass further injuring the patient, but if the patient is severely injured do not let this delay getting access to care for the patient.
The windshield and some rear windows are made of laminated glass that will require a saw to remove. Side windows are the most desirable for attempting patient access. Note that since 2018 more cars have laminated side windows also. With a window broken open, the EMR may now be able to open the door from the inside in the instance of a locked door. The tempered glass will scratch the patient if the EMR tries to brush it off bare skin. Remove the pieces off the patient during transport if the patient is not in serious condition requiring more important care. Steps for breaking a vehicle window:
- The EMR should be wearing protective clothing, eye protection, and heavy gloves
- Ensure the vehicle is stabilized
- Try all doors first
- Inform the vehicle occupants what you are doing
- Press the spring-loaded center punch into the bottom corner of the window
- Once the window is shattered, attempt to withdraw the broken glass from the window frame and leave outside the vehicle. This does not always work and it is common for some glass to end up inside the vehicle.
- Brush all glass free from the window frame to protect the EMR while entering
- Enter the vehicle through the window
More complex patient access is when doors and window access does not work. These will be incidents when rescue personnel use powerful extrication tools to remove the vehicle from around the patient to allow EMS personnel access to treat and remove the patient. Training on how to use these extrication tools is an entire course in itself, so this EMR course may create an awareness of tool operation and your instructor may coordinate a demonstration day for EMR students to practice and observe extrication techniques, but EMRs should not consider themselves proficient in vehicle extrication through only attending a single session on the topic as vehicle design and extrication tools and techniques are continually evolving requiring advanced initial and ongoing training.
Demonstrate Vehicle Stabilization Techniques
A vehicle that is upright and, on its wheels, while on a flat surface is an easy vehicle to stabilize. The vehicle should remain stable, but the EMR will want to place a chocking block or wedge in front of a front tire and behind a rear tire to prevent the vehicle from rolling. Then, once the wheels are chocked, the EMR can access the vehicle interior and try to place the vehicle transmission in the park setting and activate the vehicle parking brake.
If the vehicle is on its side, it is very unstable and will need more advanced forms of stabilization prior to the EMR accessing the vehicle and patient. Rescue personnel may use longer wooden poles or purpose-built struts, rams, and straps to stabilize a vehicle on its side. These topics are presented in extrication training courses, but exceed the scope of this EMR course. A vehicle that is on its roof is oftentimes quite stable. The EMR may need to place some wooden step cocks or wedges under the corners of the roof to stabilize it, but this should suffice if the vehicle is upside down on level and firm ground.
One concern for overturned vehicles or vehicles on their sides is leaking fuel. The EMR should be aware of this and be sure to assess these vehicles for fuel leaks. If leaking fuel is observed, the fire department should be notified to manage the leak and be prepared for potential fire suppression needs. If a vehicle is not on flat ground, the vehicle will likely be more difficult to stabilize, and rescue trained and equipped personnel should be requested to assist.
View the following supplementary videos on Patient Extrication:
Vehicle Extrication – Vehicle Stabilization
Three person extraction: Vehicle Rapid Extrication (Urgent Move)
This two hour plus video is a compilation of vehicle accident responses, to demonstrate the range of situations and responses: Live Rescue: BIGGEST Car Accident Rescues MEGA-COMPILATION | A&E
17.8 EMS Rescue Awareness
Learning Objectives
- Describe response to a scene that require specialty rescue resources
- Describe various considerations to a variety of specialty rescues
Describe Response Requiring Specialty Rescue Resources
While each EMR might hope that every patient encounter follows the textbook patient complaint presentation and each patient is sitting in a chair easily accessible and easy to transport to the ambulance, this does not happen in real life. The emergency medical work environment is unique, and people find themselves in some very odd predicaments. These patients then call 911 with the expectation that emergency responders can quickly resolve the situation. This is the case for most incidents, but this section will present some unique situations that may require additional resources and creative thinking to establish the Incident Action Plan.
Hazardous or special rescue incidents require EMRs to be aware of the warning signs and indicators for possible additional hazards to protect themselves appropriately. These incidents may require special PPE to provide protection in the hazardous environment or specialty trained technical rescue team to extricate a patient. One acronym to assist with assessing and sizing up a special rescue or hazardous incident is the ASSESS acronym. This stands for:
A: Address: How can the incident location best be described to other responders? These special incidents may happen in remote areas that do not have an exact address. So, how can this site best be described? Also, what additional resources might be needed to get the patient from the site to the ambulance such as a snowmobile, off-road utility vehicle, or boat.
S: Site: What is the site, and what unique hazards does it present? Is this a wilderness rescue situation or an industrial equipment entrapment type situation? Examine the site and review specific hazards that may be present. Then, start managing these hazards to make the site safe.
S: Situation: What is exactly going on with the situation. Is this a trauma situation with entrapment? Is the patient uninjured, but just needing assistance getting themselves out of their predicament. Are they stuck in a tree after falling from a tree stand? Will extrication equipment be needed or confined space or rope rescue equipment?
E: Establish Command: Now that you have explained the scene to other responders, examined the scene for safety hazards, and did a quick assessment of what exactly is occurring, you are the most knowledgeable person on the scene at that time, so take command and request additional resources based on your initial assessment.
S: Safety Officer: An initial safety assessment was completed during arrival at the incident location. However, these are special rescue incidents by their nature and additional safety concerns will likely emerge through the rescue incident. So, this is an incident where the Incident Commander needs to assign a separate Safety Officer to monitor the scene conditions as the incident progresses.
S: Staging: With command established and all the needed resources requested, begin planning where they will stage and how you will get them from the staging area to the incident site.
Considerations of Specialty Rescues
Ice rescue incidents create their own unique hazards as there is already at least one victim in the water and the area around the victim has proven to be unstable. When arriving at an ice rescue incident, the EMR should not drive the ambulance onto the ice or proceed onto the ice without specialized ice rescue training and equipment. If the EMR can see the victim, they should make note of the victim’s location in the event they submerge underwater. This last known location can assist the divers or ice rescue team.

Ice and water rescue scenarios follow the series of steps: throw, row, go. Ambulance services may equip their emergency vehicles with rescue rope throw bags. The EMR can tie off one end of the rope and then attempt to throw the remaining rope and bag to the victim. If using a rope or throw bag is not an option, a flat bottom boat or purpose-built ice rescue sled can be tied with a long rope to a secure item on the shore and the boat or sled used to “row” to the victim’s location. Last, if neither of these solutions are an option, and if the EMR is trained and equipped, they could put on an ice rescue suit, secure themselves to the shore with a long rope and “go” to the victim. The rescuer needs to be aware that the ice is weak as one person has already fallen through. So, crawling or using a sled or ladder to distribute their weight across the ice may be beneficial to help prevent the rescuer from also falling through the ice and needing assistance.
Water rescue incidents are often categorized as static water (lake or pond) or swift water (river or fast-moving stream). When responding to water rescue incidents, the same hazards as ice rescues need to be assessed as the scene already has at least one person in peril and rescuers should not create a situation that puts themselves in need of assistance. When working on or near water, the EMR should wear a Personal Flotation Device (PFD) as part of their PPE. The same concepts of throw, row, and go that were used for ice rescue are frequently implemented for water rescue.
If a patient in a water rescue situation may have endured a spinal column injury, such as in a shallow water diving injury, the rescuers will need to enter the water around the victim, support the patient’s head, neck, and back. Then, a long spine board can be floated underneath the patient and the patient immobilized in the water. An additional consideration occurs with deeper water SCUBA diving incidents. When a diver is forced to rapidly return to the water’s surface, they can experience a condition called decompression sickness or suffer an air embolism. It is unlikely that the EMR will be able to differentiate between these conditions in the field, but any diving patient demonstrating signs or symptoms or shortness of breath should be treated with high flow oxygen and transported to a facility capable of treating the patient with hyperbaric oxygen. Additionally, protocols or medical direction may request the patient to be transported on their left side with their feet elevated. The goal of this position is to keep a potential air embolism on the right side of the heart or lower extremities as it will rise or float on top of the circulating blood and hopefully not relocate to the left side of the heart where it could be pumped to the brain causing an ischemic stroke.
OSHA defines a confined space as a space that is large enough and configured that an individual can bodily enter it, has limited or restricted means for entry and exit, and is not designed for continuous occupancy. Industrial facilities will have numerous confined spaces that present potential risk and hazards to the workers at the company as well as any arriving emergency personnel. Confined spaces may contain limited oxygen atmospheres or chemical vapors that cannot be seen. For these reasons, special air monitoring equipment is required to be used when entering these confined spaces. EMRs should not enter a confined space without proper confined space rescue training. However, EMRs should be able to recognize these spaces and know when to request additional special training rescue resources. EMRs should also inform and help restrict other would-be rescuers from entering the confined space to render aid without the specialized training and equipment.
Industrial incidents may also require specialized technical rope rescue personnel of heavy equipment extrication equipment in addition to the concerns of confined spaces. These are also specialized areas of training that exceed the scope of this EMR course. However, just like confined spaces, industrial entrapment or high-angle rope rescue incidents will have unique hazards that require the EMR to assess the scene’s safety and request additional resources. The EMR should not attempt a rescue themselves without the special training and equipment.
17.9 Hazardous Materials
Learning Objectives
- Identify resources that can be used in the identification and management of hazardous materials
- Discuss the general rules and guidelines for hazardous materials incidents
- Discuss the components of a hazardous materials incident management, incident pre-plans, and safety zones
- Differentiate between radioactive, biological, chemical, and nuclear materials to ensure appropriate patient care
- Demonstrate the use of Emergency Response Guide
- Demonstrate Hazardous Materials Scene Activities
July, 2023: Hazmat teams were called out three separate times this week across Northeast Wisconsin. It was a busy week for Green Bay and Appleton’s fire crews with calls for hazardous materials. On Monday, two people were affected when an irritant leak occurred in a basement lab at Bellin Hospital in Green Bay. Then, late Wednesday night, a tanker crash near Freedom required crews to clean up an alcohol-based chemical that was leaking from the tanker. Last, on Thursday, a potassium hydroxide spill occurred at a warehouse on Green Bay’s west side and required containment.
Resources for Hazardous Materials Identification and Management
The diamond-shaped signs on the back or sides of semi-truck trailers are called hazardous materials placards. These placards provide details about the kind of cargo a truck is hauling. The United States Department of Transportation (DOT) requires carriers to display these placards when moving hazardous goods because they inform emergency responders of what substances the carrier was hauling if it were to be involved in an accident. A hazardous material placard has six main parts, although not every placard will include all six:
- Hazard class number
- UN/NA number
- Compatibility letters
- Color
- Words
- Graphics
View examples of hazardous materials placards:
Liquid Trucking: Top 10 Violations for HazMat Transportation
Hazardous Waste Experts: A Comprehensive Guide to Firefighter Placards
The Emergency Response Guidebook (ERG) will be described in greater detail later, but the first section, colored white, is a great reference for assisting with interpreting placards at a roadway hazardous materials incident.
If the hazardous materials release is the result of a roadway transportation release, the shipping bill of lading will be a great resource as it will list the contents and quantities of the items the carrier was shipping. Similarly, the shipping manifest will have this information for maritime shipments and the rail waybill will have this information for railway incidents.
The OSHA Hazard Communication Standard (HCS), revised in 2012, requires that the chemical manufacturer, distributor, or importer provide Safety Data Sheets (SDSs) for each hazardous chemical to downstream users to communicate information on these hazards. The information contained in the SDS is largely the same as the former Material Safety Data Sheet (MSDS), except now the SDSs are required to be presented in a consistent user-friendly, 16-section format. Safety Data Sheets are valuable tools for EMRs as they will include information to assist in identifying a specific chemical, first aid treatment measures, the required PPE for working with the chemical, and any applicable toxicological information.
Wireless Information System for Emergency Responders (WISER) was a resource used for many years to assist emergency responders at hazardous materials incidents. However, as of February 28th, 2023, NLM has discontinued the Wireless Information System for Emergency Responders (WISER).
Rules and Guidelines
EMRs play a crucial role in hazardous material incidents, providing important medical care and support in difficult conditions. Their responsibilities extend beyond the usual scope of care, requiring specialized training and decision-making to ensure the safety and well-being of both victims and responders. The first priority for EMRs at a hazardous materials incident is to ensure scene safety. They must assess the scene, identify potential hazards, and determine the appropriate level of PPE required. EMRs and other emergency responders will collaborate with the specially trained hazardous materials response team to establish safe zones to minimize the risk of exposure to others.
Decontamination is one step in the incident action plan where EMRs may render assistance. The decontamination process is critical to prevent the spread of hazardous materials and protect both the patients and the emergency responders. EMRs should know how to use decontamination equipment and follow protocols to remove contaminants from patients that may have been exposed to hazardous chemicals.
Providing medical treatment in a hazardous materials incident requires strong attention to patient signs and symptoms to properly treat the patient. EMRs should anticipate managing respiratory issues, chemical burns, and other trauma associated with potential exposure to hazardous materials. If the hazardous materials incident is also an MCI, triage will also be required to allow EMRs to prioritize care based on the severity of injuries and hazardous materials exposure.

Within the ICS structure, the liaison officer works to collaborate and coordinate between various agencies and the EMR should support this communication and collaboration with other entities at a hazardous materials scene. This collaboration helps in sharing critical information, resources, and expertise, improving the overall effectiveness of the response.
Components of a Hazardous Materials Incident
A hazardous material incident will require multiple entities to be working together collaboratively. Because of this, implementing the ICS is vital to the success of a hazardous materials incident. Each entity will bring its area of expertise and sharing this information, collaborating, and developing a uniform incident action plan will help ensure success. If a community has specific target hazard sites for potential hazardous materials incidents, EMS may wish to coordinate with other emergency response entities like fire, law enforcement, and the Local Emergency Planning Committee (LEPC) to identify the hazards that are present and pre-plan how an incident might be managed at that facility.
During a hazardous materials incident, the area of hazard will need to be identified. This hazardous area is often called the “hot zone”. Controlling access in and out of the hot zone is a safety priority at hazardous materials incidents to prevent individuals that lack the proper PPE and training from entering a dangerous area. Because of this, the hot zone is also termed the “exclusion zone”. Outside of the “hot zone” is an area where no hazards exist, and the media, bystanders, and other resources can be staged. This unhazardous area, away from the hot zone is called the “cold zone.” Between these two areas is the “warm zone”. The warm zone is not an area where hazards currently exist, but decontamination and some emergency treatment measures may occur in this warm zone. The warm zone is referred to as the contamination reduction zone as it is the transition between a hazardous environment and a non-hazardous environment.
Chemical, Biological, Radiological, and Nuclear Exposure Patients and Scenes
The acronym CBRN stands for Chemical, Biological, Radiological, and Nuclear and is frequently used to encompass a wide array of terrorism type threats that citizens and emergency responders could be exposed to. Just as trauma casualties present differently (blunt, trauma, gunshot wound, blasts, etc.), CBRN casualties also have varied presentations. For example, chlorine casualties will require more attention to respiratory symptoms contrasted with a mustard casualty’s associated skin blistering trauma. The types of CBRN agents this section will discuss include
- Nerve agents such as GA (Tabun), GB (Sarin), GD (Soman), or VX
- Routes of exposure: inhalation, absorption, ingestion
- Cyanide
- Routes of exposure: inhalation, ingestion, absorption
- Choking agents like chlorine gas and phosgene gas (CG)
- Routes of exposure: inhalation
- Vesicants (blister agents) such as mustard, lewisite, or phosgene oxime (CX)
- Routes of exposure: inhalation, ingestion, absorption
- Opioid incapacitating agents such as fentanyl
- Route of exposure: Inhalation if used as CBRN most likely
- Anticholinergic incapacitating agents such as BZ or QHB
- Route of exposure: inhalation, ingestion, absorption
- Riot control agents such as CS, OC, and CN
- Routes of exposure: inhalation, absorption,
CBRN casualties can be categorized by circumstances of exposure, the presence or absence of trauma from an explosive device, and the signs and symptoms from the CBRN exposure. In a CBRN threat environment, casualties may possess traumatic, CBRN, or mixed injuries. It is important to identify whether CBRN injuries are present in addition to any obvious traumatic injuries to allow responders to implement protective scene control and put on protective PPE.
There will be times when CBRN agent identification may have to be made solely based on clinical assessment of signs and symptoms. The acronym CRESS (Consciousness, Respirations, Eyes, Secretions, Skin) is employed to improve rapid identification of the type of chemical agent exposure. Some CBRN agents, such as nerve agents, can be rapidly fatal; therefore, recognition of such symptoms is the equivalent of identifying massive hemorrhage in the trauma patient. If the EMR fails to recognize the problem quickly, the patient will expire. Clinical clues can be compiled to identify the most likely CBRN agent responsible for symptoms according to the CRESS assessment. Each letter in CRESS corresponds to physical exam findings that can be used to categorize the suspected agent based on the constellation of findings.
| C – Consciousness | (unconscious, seizures, depressed consciousness, agitation) |
|---|---|
| R – Respirations | (present or absent, labored, increased or decreased) |
| E – Eyes | (constricted, dilated, or normal) |
| S – Secretions | (dry, normal, increased) |
| S – Skin | (diaphoretic, dry, hot, cyanosis) |
The acronym CRESS is useful for differentiating exposures to various chemical agents. Exposure to biological agents is unlikely to cause early symptoms. Radiologic exposure may lead to early onset of symptoms (<1 hour post exposure) such as nausea, vomiting, diarrhea, and fever with high dose exposures (>6 Gray). CRESS findings associated with specific chemical agents are shown below.
| CBRN Agent | Consciousness | Respirations | Eyes | Secretions | Skin |
|---|---|---|---|---|---|
| Nerve | Depressed consciousness or unconscious | Increased | Constricted (Miosis) | Increased (lacrimation, rhinorrhea, salivation, bronchial, secretions) | Diaphoretic |
| Cyanide | Depressed consciousness or unconscious | Increased | Normal | Normal | May be flushed or cyanotic when advanced shock |
| Chlorine Phosgene (delayed effects) | Normal (unless asphyxia causes loss of consciousness) | Increased | Normal | Increased (lacrimation, rhinorrhea, salivation)
Delayed fluid in lungs |
Normal |
| Blister agent/Vesicants | Normal (increased if vapor) | Normal | Normal | Increased (lacrimation, rhinorrhea, salivation)
Delayed fluid in lungs at very high doses |
Normal initially |
| Opioid Incapacitating agent | Depressed consciousness or unconscious | Decreased | Constricted (Miosis) | Normal | Normal |
| Anticholinergic Inactivating agent | Agitated | Normal or increased | Normal or dilated (mydriasis) | Decreased | Dry and hot |
| Riot control agents | Normal | Normal or increased | Normal | Lacrimation, rhinorrhea, salivation | Normal |
Emergency Response Guide (ERG)
The ERG is a guidebook intended for use by first responders during the initial phase of a transportation incident involving dangerous goods/hazardous materials. It is important to note that the scope of reference for the ERG is solely transportation goods and emergencies. It is not designed for managing incidents at fixed facilities, but still may be useful for identifying chemicals and their associated hazards. The ERG is broken into six color-coded sections. The first white section includes information on shipping papers, instructions on how to use the ERG, guidance on responding to incidents involving hazardous materials, information on placards and the hazard classification system, and pipeline information.
The next section is highlighted yellow. This second section references materials according to their four-digit identification number. This section is useful when you notice a placard or other identifier that provides you with this four-digit number. It then references the reader to the actual guide number that will provide additional information on this group of chemicals.
The third section is blue in color. This section lists chemical names alphabetically. With this list, a user can scroll through to find a chemical, if known by name, and then be guided to the correct guide number for that chemical.
The fourth section is orange and contains the greatest amount of information. The yellow and blue sections are first used to guide the reader to the correct orange section guide for a specific chemical, or family or chemicals with similar characteristics. The user would rarely start in the orange section; they would first use those earlier sections to gather the information to them move to the orange section. So, when your instructor gives you a chemical to search for and sees you first paging through the orange section, they know you didn’t complete your homework.
The fifth section is green in color and provides protective distances when a hazardous material is considered a Toxic Inhalation Hazard (TIH). These distances are based on the amount of material that has been released, and the time of the day the incident has occurred in. Materials in the Yellow and Blue sections that are highlighted in green refer to this section. The last section is also colored white and in the back of the guidebook. This white section includes use instructions but also contains additional information for potential pressure vessel gas explosions known as Boiling Liquid Expanding Vapor Explosions (BLEVEs) and a glossary of terms for the user.
17.10 EMS Response to Terrorism
Learning Objectives
- Explain the importance of preplanning a response to terrorism involving weapons of mass destruction
- Identify the primary, secondary, and tertiary effects of conventional weapons and incendiary devices used during terrorist events
- Discuss the responsibilities of EMRs during an Active Shooter Incident
Preplanning for a Terrorism Response
Like other MCI events, terrorist attacks can occur anywhere and the idea that these will not occur in a rural community is old thinking. Every community should prepare for terrorism as part of its MCI/ disaster preparedness planning. Coordination with the county Emergency Management department and other public safety entities is paramount to help ensure each entity is preparing for the various terrorism threats the same way.
Effects of Explosives and Incendiary Devices

The easiest to obtain and use of all terrorism weapons is still a conventional explosive device, or improvised bomb, which may be used to cause massive local destruction or to disperse CBRN agents. Explosives are any chemical compound, mixture, or device, the primary or common purpose of which is to function by explosion. The term explosive includes, but is not limited to, black powder, pellet powder, initiating explosives, ammonium nitrate fuel oil (ANFO) mixtures, safety fuses, squibs, mixed binary explosives, and igniters. Explosives are also present in items such as automotive air bag inflators, special industrial tools, fire extinguishers, some pest control devices, some model rocket engines, fireworks, and special effects in the entertainment industry. Incendiary devices are weapons or munitions designed to set fire to objects or cause burn or respiratory injury to people through the action of flame, heat, or combination thereof, resulting from a chemical reaction of a flammable substance such as napalm or white phosphorus.
The components for creating incendiary or explosive devices are readily available, as are detailed instructions on constructing such a device. Improvised explosive devices are categorized as being explosive or incendiary, employing high or low filler explosive materials to explode and/or cause fires. Bombs and firebombs are cheap and easily constructed, involve low technology, and are the terrorist weapon most likely to be encountered. Large, powerful devices can be outfitted with timed or remotely triggered detonators and can be designed to be activated by light, pressure, movement, or radio transmission.
The potential exists for single or multiple bombing incidents in single or multiple municipalities. Historically, less than five percent of actual or attempted bombings were preceded by a threat. Secondary explosive devices may also be used as weapons against responders and the public in coincident acts. Other diversionary events or attacks could also be aimed at responders.
Explosions are physical phenomena that result in the sudden release of energy; they may be chemical, nuclear, or mechanical. This explosive process results in a near-instantaneous pressure rise above atmospheric pressure. The positive pressure rise (“overpressure”) compresses the surrounding medium (air or water) and results in the formation of a blast wave, which extends outward from the explosion in a radial fashion. Explosive blast may have five distinct effects on the body:
- Primary blast effects causing injuries as sole consequences of the shock wave–body interaction
- Secondary blast effects from the fragments of debris propelled by the explosion and connecting with the body, causing penetrating and/or blunt trauma
- Tertiary blast effects from acceleration/deceleration of the body or part of the body
- Quaternary blast effects caused by the transient but intense heat of the explosion (flash burns)
- Quinary blast effects caused by “post-detonation environmental contaminants,” such as bacteria and radiation from dirty bombs, and tissue reactions to fuel and metal residues, among others.
Often, especially in the case of moderate-to-severe blast injuries, the multiple blast effects interact with the body simultaneously creating multi-system trauma.
Responsibilities of EMR During Active Shooter Incident
During an active shooter event, law enforcement’s focus will be on making a safe scene so EMS’s focus should be planning for the treatment of casualties. It is the perpetrator’s intended purpose to kill or injure people. Plan for casualties, when and where they will be treated, and how they will be evacuated from the point of wounding. Preplanning can include determining which agency or personnel will locate casualties, triage them, provide point of wounding medical stabilization, and/or extricate them to a safe location. There should be pre-planning discussions with medical directors, medical control and with the primary receiving medical centers regarding the principles of Tactical Emergency Casualty Care (TECC).
As the civilian equivalent of the military combat medical guidelines, the TECC guidelines account for the unique operational considerations of medical operations in high-risk environments and prioritize and focus medical efforts to only what must immediately be done to affect survival. Considerations should be made for all potential emergency responders, including EMRs to be trained to the basic tenets of TECC. The survival benefit of TECC is based on rapid application of point-of-wounding care, thus the equipment must be forward deployed for care to be immediately implemented. This requires that TECC equipment and supplies be carried with all other medical aid and equipment. In short, TECC equipment could become a valuable part of the standardized equipment for fire/EMS response assets.
Tactical EMS (TEMS) support personnel are not a typical resource for supporting MCI patient care because they are usually very limited in number, not immediately available, and committed to their tactical team’s assignment. This will preclude them from casualty care activities until the tactical team’s objective is met. Considerations, planning and interagency training should occur around the concept of properly trained, armored medical personnel who are escorted into areas of mitigated risk, which are clear but not secure areas, to execute triage, medical stabilization at the point of wounding, and provide for evacuation or sheltering-in-place.
Some jurisdictions accomplish this through the deployment of Rescue Task Forces (RTFs). Under the protection of law enforcement officers these teams treat, stabilize and remove the injured rapidly while wearing ballistic protective equipment. It is recommended that an RTF team should include at least one Advanced Life Support (ALS) provider. When possible, agencies should plan for warm zone area medical operations to provide TECC-driven point-of-wounding care (such as massive hemorrhage control) according to their resources and capabilities. Responders also need to consider secondary devices at the main scene and secondary scenes in close proximity to the main scene.
17.11 EMS Response to Disaster
Learning Objectives
- Explain the importance of preplanning a response to disaster
- Discuss complications for responding crews during disaster
- Explain changes to care in disaster patients
With proper planning, training, and incident action plan implementation, a multiple casualty incident does not have to become a disaster.
The Importance of Preplanning a Response to Disaster
Within emergency services, there is an acronym NIMBY. NIMBY stands for the thought of Not In My Back Yard. This thought was prevalent early in the integration of FEMA’s ICS and NIMS concepts. Many agencies assumed that interoperability and disaster planning was just something that large cities or special events needed to do. However, this mindset has fortunately changed and even the most remote rural community acknowledges that they are not immune to hazardous materials train derailment, plane crash, or an active shooter incident. As the saying goes, an ounce of prevention is worth a pound of cure.
Disaster preplanning is something that each EMS agency should do. Fortunately, there are numerous resources to assist. Each community is required to have an Emergency Operations Plan (EOP). Within the EOP, the Emergency Management office has completed a Target Hazard Identification and Risk Assessment (THIRA). This THIRA assessment looks to assess the community’s vulnerability to various disaster type situations. These hazards are then categorized by the likelihood of occurring, and the potential severity if they were to occur. This categorization then helps emergency management, law enforcement, fire, and EMS develop plans for handling the various types of situations. Having the single operation plan assists in guaranteeing that all agencies are preparing for the same hazards, the same way.
Disaster communications will strain the most robust communication system. During the September 11, 2001, terrorist attacks, the City of New York had a robust communication system, but it still failed to work perfectly. Communities should anticipate communication concerns during disaster response and plan for system redundancy in the event of failure and identify secondary communication methods. Many advancements have been made by narrowing the frequencies of radio communication channels for emergency responders, allowing very High Frequency (VHF) and Ultra High Frequency (UHF) for emergency responders, and encrypting some radio channels to maintain confidentiality of radio communicated messages.
Wisconsin’s motto is “Forward”, and our state has been very forward thinking around disaster mutual aid communication planning. The State established the Mutual Aid Frequency Coordination Group (MFCG) as a committee of the State Interoperability Council to manage the statewide mutual aid/interoperability radio channel resources. The MFCG encourages all public safety agencies in Wisconsin to implement the statewide common frequencies. In some cases, there are local radio frequency assignments that may conflict with the statewide use plan. For this reason, counties and agencies with additional frequencies are encouraged to implement the statewide plan frequencies and make their currently licensed frequencies available for reassignment. The IFERN (Interagency Fire Emergency Radio Network) channels, the MARC (Mutual Aid Response Channel) channels, and the EMS ALS, BLS, and Coordination (A, B, and C) are examples of pre-established mutual aid radio frequencies to support radio communications at disaster events.
Complications for Responding Crews During Disaster

When responding to an incident or while transporting a patient to a healthcare facility, a disaster incident may create additional route planning and driving concerns. Additionally, a terrorist type incident may have planned secondary or diversionary incidents that could impact route planning before, during, or after the peak of the incident. Blocked roads can occur due to severe weather or backed up, or disabled vehicles. Emergency vehicle operators should use sound judgement if electing to leave the paved roadway surface to try and drive around an obstacle. Emergency vehicles are much heavier than commuter vehicles and can easily become stuck in soft soil or overturned if attempting to traverse a sloped surface. When a blocked road situation occurs, consult with dispatch as they may have an alternate route. Last, if a roadway is closed and traffic has stopped due to the incident, it might be possible to travel in the opposing traffic lanes. If exercising this statutorily allowed exemption and traveling against the typical flow of traffic, be sure to activate all emergency lighting and siren and operate with due regard for all on the roadway.
Downed trees are common during Wisconsin severe weather. It could be from a spring flood, a summer tornado, strong winds in the fall, or a winter ice storm. In Wisconsin, we get to do year-round disaster planning! If downed trees are encountered, assess for other potential associated hazards such as downed power lines, flooding, or if the downed tree is the result of a vehicle collision. Then, evaluate if the tree can safely be driven around without leaving the roadway or causing a hazard to others on the roadway. If the tree cannot be navigated around, dispatch may be able to assist with an alternate route, or direct other resources to the area that may be able to clear the tree from the roadway.
Flooding is a common occurrence in Wisconsin and can occur at nearly every time of the year. When the hazard of high water is present, this also needs to be recognized as a hazardous environment. The National Weather Service has a program termed “turn around, don’t drown” to try and keep people from driving through flood water. Also, when vehicles become disabled in flood waters, occupants frequently attempt to leave the vehicle to return to dry ground but are overtaken by floodwater currents. For these reasons, emergency responders should also not attempt to drive through flood waters without purpose-built high-water vehicles. This is another time when dispatchers may be aware of alternate routes to the incident location that are not as severely impacted by floodwaters.
Downed power lines can create concerns for safety both at the site of an incident but also for traveling through or past to get to an incident. Whenever EMRs notice the presence of a downed powerline, they should assume the downed lines to be energized and dangerous until a utility provider has confirmed them to be otherwise. Additionally, the EMRs should communicate this hazard to the Safety Officer at the scene so they can ensure that other responders are aware of the hazard and do not risk exposure to it.
Communication outages can occur due to remote location or failure of the utility networks for landline or cellular phones and radios. Most agencies have protocols to discuss standing orders for when communication failures occur for offline medical direction. However, these incidents can require some out of the box thinking for responders. For example, if the existing radio system is not working, it might be possible to use the radio system of law enforcement or another entity at the incident to relay important messages as their radio system may still be intact. Also, if the cellular network has failed, using the landline phone from the patient’s residence might serve as a valuable option. For this reason, agencies should consider keeping a list of important phone numbers in a location other than just in the cellular phone’s contact listing as this will become useless when the cell phone battery is dead.
Last, when a large-scale incident occurs, there will be high demand on the communication network from both emergency response personnel and civilians wanting to contact loved ones or share information on social media. FEMA created the Government Emergency Telecommunication Service (GETS) to provide priority access to communication networks for emergency responders. Your agency may request a GETS card for vehicles or important personnel to allow for priority communication access in these sorts of incidents.
EMRs may be dispatched to a location that does not have any physical address or road signs to assist with locating. Dispatch can be a tremendous asset during these occurrences by sharing landmarks, longitude and latitude cartesian coordinates, or other information that can assist with locating the incident location or patient. Public safety use of drones has increased in recent years, and this can be a valuable tool to find patients and assist in guiding emergency response to the location.
Changes to Care in Disaster Patients
Large scale incidents or disasters will create a stressful situation for the emergency responders managing the incident. Additionally, these incidents will increase stress on patients. If the incident is an MCI level incident, patients will be delayed in their transport for definitive care as more immediate concerns are addressed. Additionally, they may be triaged to an area where they are surrounded by other injured patients.
17.12 Summary
This chapter presented the EMR with vital information on EMS emergency services operations. The EMR can now recognize safety hazards and safely conduct patient care in a variety of uniquely challenging operational environments.
17.13 References
@Ryan Skabroud – Are there References sources you used that need to be cited here?
Images:
Figure 17.1: This image is derivative of “3112965594_f13238a9a4_b” by Eric Norris and is licensed under CC BY 2.0, “Ambulance_Toronto_March_2010” by Michael Gil from Toronto, ON, Canada is licensed under CC BY 2.0, “Ambulance_with_lights_flashing_at_night” by Kurt Kaiser is licensed under CC0, Public Domain, and “A23-2night1” by MPD01605 is licensed under CC BY-SA 2.5
Figure 17.2: “pexels-nhp-co-456980180-15571631” by NHP&Co, via Pexels.com is licensed under CC0
Figure 17.3: “Pegasus Stride showcases Pittsburgh FCC and 911th AW’s Disaster Response interoperability” by SSgt James Fritz is in the Public Domain. The appearance of U.S. Department of Defense (DoD) visual information does not imply or constitute DoD endorsement.
Figure 17.4:”EMR Switches” by Mark Schwartz, Chippewa Valley Technical College is licensed under CC BY-NC 4.0
Figure 17.5: “manual_power_autoload” by Mark Schwartz, Chippewa Valley Technical College is licensed under CC BY-NC 4.0
Figure 17.6: “Puget Sound Federal Coordinating Center National Disaster Medical System“, by John Wayne Liston is in the Public Domain. The appearance of U.S. Department of Defense (DoD) visual information does not imply or constitute DoD endorsement.
Figure 17.7: “pexels-pixabay-70573” by Pixabay, via Pexels.com is licensed under CC0
Figure 17.8: “Fallon_Ambulance_at_Milton_Music_Festival” by Mangocove is licensed under CC BY-SA 4.0
Figure 17.9: “Coast Guard Sector San Diego medevacs burn victim” by Petty Officer 1st Class Henry G. Dunphy is in the Public Domain. The appearance of U.S. Department of Defense (DoD) visual information does not imply or constitute DoD endorsement.
Figure 17.10: “Water_rescue_training” by Staffsfire is licensed under CC BY-SA 4.0
Figure 17.11: “pexels-joshua-santos-1174893-5564264” by Joshua Santos, via Pexels.com is licensed under CC0
Figure 17.12: “pexels-torbenb-3623114” by Torben Bühl, via Pexels.com is licensed under CC0
Figure17.13: “pexels-rdne-6520108” by RDNE Stock Project, via Pexels.com is licensed under CC0
Videos:
Superior Ambulance. (2024, December 5). Day in the life at Superior Ambulance of Illinois [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=3UOiB0vkhdA
Superior Ambulance. (2024, July 5). Wisconsin day in the life [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=ZHYQchGlpB4
Boston Medflight. (2019, January 24). Landing zone safety full training final [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=w1cWAdAzdhE
Action Training Systems – Fire & EMS Training. (2018, July 18). Vehicle extrication – vehicle stabilization [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=q9szkAdRq6E
911 e-Learning Solutions. (2024, May 18). Vehicle rapid extrication (urgent move) [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=9-E-6_DJgDo
A&E. (2023, February 2). Live rescue: biggest car accident rescues mega-compilation | A&E [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=wFcFiwEsd3E

